Hypernatremia is essentially a laboratory diagnosis, defined as a serum sodium concentration of >145 mEq/L. Severe hypernatremia has variously been defined as a serum sodium concentration of >152 mEq/L, 155 mEq/L, or >160 mEq/L.[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79.[3]Nur S, Khan Y, Nur S, et al. Hypernatremia: correction rate and hemodialysis. Case Rep Med. 2014;2014:736073.
https://www.hindawi.com/journals/crim/2014/736073
http://www.ncbi.nlm.nih.gov/pubmed/25431600?tool=bestpractice.com
[4]Cabassi A, Tedeschi S. Severity of community acquired hypernatremia is an independent predictor of mortality: a matter of water balance and rate of correction. Intern Emerg Med. 2017 Jul 1;12(7):909-11.
http://www.ncbi.nlm.nih.gov/pubmed/28669048?tool=bestpractice.com
However, there is no consensus as to the exact level. Hypernatremia is hospital acquired in the majority of cases.[11]Sterns RH. Hypernatremia in the intensive care unit: instant quality - just add water. Crit Care Med. 1999 Jun;27(6):1041-2.
http://www.ncbi.nlm.nih.gov/pubmed/10397193?tool=bestpractice.com
[12]Palevsky PM, Bhagrath R, Greenberg A. Hypernatremia in hospitalized patients. Ann Intern Med. 1996 Jan 15;124(2):197-203.
https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=e83a8ef7849fb3ab65a62b5e366897be24895be5
http://www.ncbi.nlm.nih.gov/pubmed/8533994?tool=bestpractice.com
[13]Long CA, Marin P, Bayer AJ, et al. Hypernatraemia in an adult in-patient population. Postgrad Med J. 1991 Jul;67(789):643-5.
https://pmj.bmj.com/content/postgradmedj/67/789/643.full.pdf
http://www.ncbi.nlm.nih.gov/pubmed/1924049?tool=bestpractice.com
[15]Salahudeen AK, Doshi SM, Shah P. The frequency, cost, and clinical outcomes of hypernatremia in patients hospitalized to a comprehensive cancer center. Support Care Cancer. 2013 Jul;21(7):1871-8.
http://www.ncbi.nlm.nih.gov/pubmed/23404230?tool=bestpractice.com
A detailed history and thorough physical examination (including an evaluation of the patient’s volume status and mental status) are important to diagnose the underlying cause.[1]Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015 Mar 1;91(5):299-307.
https://www.aafp.org/afp/2015/0301/p299.html
http://www.ncbi.nlm.nih.gov/pubmed/25822386?tool=bestpractice.com
Evaluation of urine osmolality and electrolytes is also helpful in determining the underlying cause and aids in formulating a treatment plan.
History
The history should focus on the following three factors:
Risk factors for the development of hypernatremia include:
High urine or stool output (e.g., renal dysfunction, Clostridium difficile infection)
The inability to drink water/limited access to water (e.g., older/dementia patients, ventilated/intubated patients in intensive care unit, impaired mental status)
The inability to concentrate urine (e.g., diabetes insipidus, osmotic diuresis, obstructive uropathy, renal failure).
The patient's age may give a clue to the underlying etiology:
Neonates may develop hypernatremic dehydration due to inadequate fluid intake, usually related to poor lactation or insufficient maternal milk supply.[69]Bischoff AR, Dornelles AD, Carvalho CG. Treatment of hypernatremia in breastfeeding neonates: a systematic review. Biomed Hub. 2017 Jan-Apr;2(1):1-10.
https://www.karger.com/Article/FullText/454980
http://www.ncbi.nlm.nih.gov/pubmed/31988896?tool=bestpractice.com
Neonatal hypernatremic dehydration is associated with a free water deficit.[70]Sarin A, Thill A, Yaklin CW. Neonatal hypernatremic dehydration. Pediatr Ann. 2019 May 1;48(5):e197-200.
http://www.ncbi.nlm.nih.gov/pubmed/31067335?tool=bestpractice.com
The neonates may present with nonspecific features such as jaundice, high temperature, poor oral intake, lethargy and low urine output.[69]Bischoff AR, Dornelles AD, Carvalho CG. Treatment of hypernatremia in breastfeeding neonates: a systematic review. Biomed Hub. 2017 Jan-Apr;2(1):1-10.
https://www.karger.com/Article/FullText/454980
http://www.ncbi.nlm.nih.gov/pubmed/31988896?tool=bestpractice.com
Correction of sodium levels in neonates should be undertaken cautiously to avoid adverse effects. There is no consensus as to method or rate of correction, though common recommendations are to correct sodium levels by no more that 0.5 mEq/L/hour with gradual correction over 48 hours.[69]Bischoff AR, Dornelles AD, Carvalho CG. Treatment of hypernatremia in breastfeeding neonates: a systematic review. Biomed Hub. 2017 Jan-Apr;2(1):1-10.
https://www.karger.com/Article/FullText/454980
http://www.ncbi.nlm.nih.gov/pubmed/31988896?tool=bestpractice.com
[70]Sarin A, Thill A, Yaklin CW. Neonatal hypernatremic dehydration. Pediatr Ann. 2019 May 1;48(5):e197-200.
http://www.ncbi.nlm.nih.gov/pubmed/31067335?tool=bestpractice.com
Infants are at risk of hypernatremia if they inadvertently ingest a large volume of salt, as they do not often have free access to water. Central diabetes insipidus can be a congenital condition, usually due to a vasopressin (V2) mutation on the X chromosome.[54]Martin PY, Schrier RW. Role of aquaporin-2 water channels in urinary concentration and dilution defects. Kidney Int Suppl. 1998 Apr;65:S57-62.
http://www.ncbi.nlm.nih.gov/pubmed/9551433?tool=bestpractice.com
Congenital nephrogenic diabetes insipidus is rare.
Older patients are particularly at risk of hypernatremia due to various factors, including an inability to concentrate urine properly, lack of thirst (e.g., due to dementia), an inability to access water (e.g., due to altered mental status from illness, stroke, immobility), and/or increased insensible losses (e.g., due to fever and/or infection). Older patients living in nursing homes are most likely to develop hypovolemic hypernatremia due to inadequate free water intake, especially patients with dementia.[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79.[71]Cappola AR, Auchus RJ, El-Hajj Fuleihan G, et al. Hormones and aging: an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2023 Jul 14;108(8):1835-74.
https://academic.oup.com/jcem/article/108/8/1835/7192004
http://www.ncbi.nlm.nih.gov/pubmed/37326526?tool=bestpractice.com
A complete medical history, including the presence of any chronic conditions (e.g., poorly controlled diabetes mellitus, renal impairment) or acute conditions (e.g., viral gastroenteritis) should be elicited. A history of traumatic brain injury or any other insult to the brain (e.g., vascular syndromes, infections, tumors, or aggressive surgery for craniopharyngioma, Rathke cleft cyst, or other hypothalamic tumors) may be suggestive of central diabetes insipidus.[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79. Recent extreme heat exposure or exercise, cutaneous burns, fever, or infection may point toward fluid loss as a cause.
A complete medication history should be taken, as the following drugs have been associated with hypernatremia:
Lithium: a mood stabilizer that is commonly associated with nephrogenic diabetes insipidus in adults, usually after chronic administration. This is possibly due to a significant down-regulation of the aquaporin 2 collecting duct (AQP2) gene.[52]Rej S, Looper K, Segal M. Do antidepressants lower the prevalence of lithium-associated hypernatremia in the elderly? A retrospective study. Can Geriatr J. 2013 Jun 3;16(2):38-42.
http://www.ncbi.nlm.nih.gov/pubmed/23737927?tool=bestpractice.com
[54]Martin PY, Schrier RW. Role of aquaporin-2 water channels in urinary concentration and dilution defects. Kidney Int Suppl. 1998 Apr;65:S57-62.
http://www.ncbi.nlm.nih.gov/pubmed/9551433?tool=bestpractice.com
Patients on chronic lithium therapy have a 50% chance of developing nephrogenic diabetes insipidus,[55]Berl T, Schrier RW. Disorders of water homeostatis. In: Schrier RW, 7th ed. Renal and electrolyte disorders. Philadelphia, PA: Lippincott, Williams and Wilkins; 2010:1-44. which can sometimes persist even after lithium therapy is stopped.
Other drugs reported to cause diabetes insipidus more rarely include: vasopressin receptor antagonists, demeclocycline, ethanol, foscarnet, temozolomide, dexmedetomidine, cisplatin, aminoglycosides, amphotericin B, penicillin derivatives, vitamin A or D excess, colchicine, vinblastine, and phenytoin.[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79.[53]Navarro JF, Quereda C, Quereda C, et al. Nephrogenic diabetes insipidus and renal tubular acidosis secondary to foscarnet therapy. Am J Kidney Dis. 1996 Mar;27(3):431-4.
http://www.ncbi.nlm.nih.gov/pubmed/8604715?tool=bestpractice.com
[56]Liamis G, Milionis HJ, Elisaf M. A review of drug-induced hypernatraemia. NDT Plus. 2009 Oct;2(5):339-46.
https://academic.oup.com/ckj/article/2/5/339/454718
http://www.ncbi.nlm.nih.gov/pubmed/25949338?tool=bestpractice.com
[59]Ji F, Liu H. Intraoperative hypernatremia and polyuric syndrome induced by dexmedetomidine. J Anesth. 2013 Aug;27(4):599-603.
http://www.ncbi.nlm.nih.gov/pubmed/23377505?tool=bestpractice.com
[60]Faje AT, Nachtigall L, Wexler D, et al. Central diabetes insipidus: a previously unreported side effect of temozolomide. J Clin Endocrinol Metab. 2013 Oct;98(10):3926-31.
https://academic.oup.com/jcem/article/98/10/3926/2833818
http://www.ncbi.nlm.nih.gov/pubmed/23928668?tool=bestpractice.com
[61]Dixit S, Salvage D, Rajaraman C, et al. Hypernatremia-associated myelinolysis following the management of sepsis in a patient with glioblastoma treated with radiotherapy and temozolomide. Acta Neurol Belg. 2013 Dec;113(4):527-30.
http://www.ncbi.nlm.nih.gov/pubmed/23389807?tool=bestpractice.com
Loop diuretics: cause an increase in free water excretion.
Intravenous mannitol: can cause osmotic diuresis.
Laxative or bowel cleansing agents: can cause severe diarrhea.
Activated charcoal/sorbitol: hypernatremia has been reported in patients treated with this drug combination for poisoning due to profuse diarrhea.[28]Gazda-Smith E, Synhavsky A. Hypernatremia following treatment of theophylline toxicity with activated charcoal and sorbitol. Arch Intern Med. 1990 Mar;150(3):689, 692.
http://www.ncbi.nlm.nih.gov/pubmed/2310292?tool=bestpractice.com
[29]Moore CM. Hypernatremia after the use of an activated charcoal-sorbitol suspension. J Pediatr. 1988 Feb;112(2):333.
http://www.ncbi.nlm.nih.gov/pubmed/3339521?tool=bestpractice.com
Sodium polystyrene sulfonate/sorbitol: has been associated with hypernatremia when used to treat patients with hyperkalemia.
Corticosteroids: increase urea production and are associated with an increased risk of hypernatremia, particularly when used in high doses e.g., in treatment of sepsis.[56]Liamis G, Milionis HJ, Elisaf M. A review of drug-induced hypernatraemia. NDT Plus. 2009 Oct;2(5):339-46.
https://academic.oup.com/ckj/article/2/5/339/454718
http://www.ncbi.nlm.nih.gov/pubmed/25949338?tool=bestpractice.com
[58]Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids for treating sepsis in children and adults. Cochrane Database Syst Rev. 2019 Dec 6;12(12):CD002243.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002243.pub4/full
http://www.ncbi.nlm.nih.gov/pubmed/31808551?tool=bestpractice.com
Fosfomycin (when administered intravenously), has been associated with hypernatremia.[73]Scavone C, Mascolo A, Bernardi FF, et al. Hypernatremia during intravenous treatment with fosfomycin: a retrospective medical record review study and an analysis of spontaneous reports in the EudraVigilance database. Front Pharmacol. 2022;13:844122.
https://www.frontiersin.org/articles/10.3389/fphar.2022.844122/full
http://www.ncbi.nlm.nih.gov/pubmed/35422698?tool=bestpractice.com
Topiramate can cause hypernatremia.[74]Muaddi L, Osman O, Clark B. Topiramate-induced severe electrolyte abnormalities and hypernatremia leading to central pontine myelinolysis. BMJ Case Rep. 2021 Nov 30;14(11):e245870.
https://casereports.bmj.com/content/14/11/e245870
http://www.ncbi.nlm.nih.gov/pubmed/34848414?tool=bestpractice.com
Iatrogenic causes (e.g., inadvertent administration of hypertonic saline, administration of hypertonic sodium bicarbonate solution in patients with metabolic acidosis) are common in hospitalized patients.[11]Sterns RH. Hypernatremia in the intensive care unit: instant quality - just add water. Crit Care Med. 1999 Jun;27(6):1041-2.
http://www.ncbi.nlm.nih.gov/pubmed/10397193?tool=bestpractice.com
[12]Palevsky PM, Bhagrath R, Greenberg A. Hypernatremia in hospitalized patients. Ann Intern Med. 1996 Jan 15;124(2):197-203.
https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=e83a8ef7849fb3ab65a62b5e366897be24895be5
http://www.ncbi.nlm.nih.gov/pubmed/8533994?tool=bestpractice.com
[13]Long CA, Marin P, Bayer AJ, et al. Hypernatraemia in an adult in-patient population. Postgrad Med J. 1991 Jul;67(789):643-5.
https://pmj.bmj.com/content/postgradmedj/67/789/643.full.pdf
http://www.ncbi.nlm.nih.gov/pubmed/1924049?tool=bestpractice.com
[75]Lindner G, Funk GC, Schwarz C, et al. Hypernatremia in the critically ill is an independent risk factor for mortality. Am J Kidney Dis. 2007 Dec;50(6):952-7.
http://www.ncbi.nlm.nih.gov/pubmed/18037096?tool=bestpractice.com
Ingestion of large quantities of salt (either intentionally or accidentally) should also be considered, especially in children. Rarely, features of Cushing syndrome or hyperaldosteronism may be present in mild cases of hypernatremia.
Symptoms of hypernatremia are nonspecific and depend on the underlying cause and the severity. If hypernatremia is acute (generally defined as onset within <48 hours), the higher osmolality in the extracellular space causes water to move out of brain cells causing the brain to shrink. This shrinkage can lead to neurological manifestations, including lethargy, weakness, and irritability. If severe, adverse manifestations can include intracranial hemorrhage, seizures, stupor, coma, and death.[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79.[66]Sterns RH. Disorders of plasma sodium - causes, consequences, and correction. N Engl J Med. 2015 Jan 1;372(1):55-65.
http://www.ncbi.nlm.nih.gov/pubmed/25551526?tool=bestpractice.com
Severe polyuria, polydipsia, and dilute urine may indicate diabetes insipidus.
Physical examination
Examination should focus on the volume status, particularly noting severe hypovolemia, which generally needs urgent correction. Hypernatremia that presents on admission to the hospital generally occurs in the setting of hypovolemia and inadequate free water intake, and is most commonly associated with older dementia patients who have a fever and/or infection.[1]Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015 Mar 1;91(5):299-307.
https://www.aafp.org/afp/2015/0301/p299.html
http://www.ncbi.nlm.nih.gov/pubmed/25822386?tool=bestpractice.com
[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79.[12]Palevsky PM, Bhagrath R, Greenberg A. Hypernatremia in hospitalized patients. Ann Intern Med. 1996 Jan 15;124(2):197-203.
https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=e83a8ef7849fb3ab65a62b5e366897be24895be5
http://www.ncbi.nlm.nih.gov/pubmed/8533994?tool=bestpractice.com
[23]Shah MK, Workeneh B, Taffet GE. Hypernatremia in the geriatric population. Clin Interv Aging. 2014 Nov 19;9:1987-92.
https://www.dovepress.com/hypernatremia-in-the-geriatric-population-peer-reviewed-fulltext-article-CIA
http://www.ncbi.nlm.nih.gov/pubmed/25429210?tool=bestpractice.com
[24]Mahowald JM, Himmelstein DU. Hypernatremia in the elderly: relation to infection and mortality. J Am Geriatr Soc. 1981 Apr;29(4):177-80.
http://www.ncbi.nlm.nih.gov/pubmed/7204813?tool=bestpractice.com
[25]Maggs FG. The management of patients presenting with hypernatraemia: is aggressive management appropriate? Clin Med. 2014 Jun;14(3):260-3.
http://www.ncbi.nlm.nih.gov/pubmed/24889569?tool=bestpractice.com
[26]Wolff A, Stuckler D, McKee M. Are patients admitted to hospitals from care homes dehydrated? A retrospective analysis of hypernatraemia and in-hospital mortality. J R Soc Med. 2015 Jul;108(7):259-65.
https://journals.sagepub.com/doi/10.1177/0141076814566260
http://www.ncbi.nlm.nih.gov/pubmed/25592963?tool=bestpractice.com
Signs of hypovolemia include:
Diabetes insipidus is characterized by the output of a large volume of dilute urine. The presence of dilute urine in the context of hypernatremia is diagnostic for diabetes insipidus. Most of these patients never develop hypernatremia as they have an intact thirst mechanism and, therefore, are able to drink water when necessary. However, in those unable to drink water, severe hypernatremia can develop rapidly. See Diabetes insipidus.
Adipsia or hypodipsia is a very rare cause of hypovolemic hypernatremia and can be seen in patients with normal mental status who lack a sense of thirst.[31]Hammond DN, Moll GW, Robertson GL, et al. Hypodipsic hypernatremia with normal osmoregulation of vasopressin. N Engl J Med. 1986 Aug 14;315(7):433-6.
http://www.ncbi.nlm.nih.gov/pubmed/3736620?tool=bestpractice.com
[32]Assadi FK, Johnston B, Dawson M, et al. Recurrent hypertonic dehydration due to selective defect in the osmoregulation of thirst. Pediatr Nephrol. 1989 Oct;3(4):438-42.
http://www.ncbi.nlm.nih.gov/pubmed/2642114?tool=bestpractice.com
[33]Nakamura-Utsunomiya A, Hiyama TY, Okada S, et al. Characteristic clinical features of adipsic hypernatremia patients with subfornical organ-targeting antibody. Clin Pediatr Endocrinol. 2017 Sep 28;26(4): 197-205.
https://www.jstage.jst.go.jp/article/cpe/26/4/26_2016-0036/_pdf/-char/en
http://www.ncbi.nlm.nih.gov/pubmed/29026268?tool=bestpractice.com
[76]Sabzghabaei F, Rastegar A. Adipsic hypernatremic myopathy. Iran J Kidney Dis. 2015 May;9(3):256-8.
http://www.ijkd.org/index.php/ijkd/article/view/1924/779
http://www.ncbi.nlm.nih.gov/pubmed/25957431?tool=bestpractice.com
Initial investigations
A full serum electrolyte panel with glucose, blood urea nitrogen, and creatinine should be ordered in all patients to assess for the presence of other electrolyte abnormalities, renal impairment, and uncontrolled diabetes mellitus. A serum sodium concentration >145 mEq/L confirms the presence of hypernatremia.[1]Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015 Mar 1;91(5):299-307.
https://www.aafp.org/afp/2015/0301/p299.html
http://www.ncbi.nlm.nih.gov/pubmed/25822386?tool=bestpractice.com
Severe hypernatremia has variously been defined as a serum sodium concentration of >152 mEq/L, >155 mEq/L, or >160 mEq/L.[2]Sam R, Ing TS. Sodium and water disturbances. In: Lai KN, ed. A practical manual of renal medicine, nephrology, dialysis and transplantation. Singapore: World Scientific Publishing C.; 2009:45-79.[3]Nur S, Khan Y, Nur S, et al. Hypernatremia: correction rate and hemodialysis. Case Rep Med. 2014;2014:736073.
https://www.hindawi.com/journals/crim/2014/736073
http://www.ncbi.nlm.nih.gov/pubmed/25431600?tool=bestpractice.com
[4]Cabassi A, Tedeschi S. Severity of community acquired hypernatremia is an independent predictor of mortality: a matter of water balance and rate of correction. Intern Emerg Med. 2017 Jul 1;12(7):909-11.
http://www.ncbi.nlm.nih.gov/pubmed/28669048?tool=bestpractice.com
However, no consensus has been reached on the exact level. Extremely high serum sodium levels occur in salt poisoning.
Once hypernatremia has been confirmed, further investigations should be ordered to help determine the etiology and formulate a treatment plan, and include:
Urine osmolality
Urine electrolytes
Urine flow rate.
Urine osmolality should be measured in all patients with hypernatremia as it may help determine the underlying etiology.[Figure caption and citation for the preceding image starts]: Possible etiologies of hypernatremia based on urine osmolalityCreated by the BMJ Knowledge Centre [Citation ends].
Urine electrolytes and urine flow rate are used to calculate the electrolyte-free water excretion (also known as electrolyte-free water clearance).[Figure caption and citation for the preceding image starts]: Electrolyte-free water excretion formula. V = urine flow rate. UNa = urine concentration of sodium (mEq/L). UK = urine concentration of potassium (mEq/L). PNa = plasma concentration of sodium (mEq/L)Created by the BMJ Knowledge Centre [Citation ends].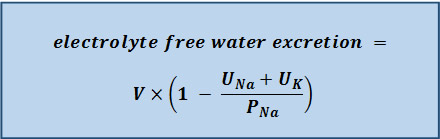 The electrolyte-free water excretion value indicates how much electrolyte-free water is being lost through the urine at any given time.[64]Edelman IS, Leibman J, O'Meara MP, et al. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. J Clin Invest. 1958 Sep;37(9):1236-56.
https://www.jci.org/articles/view/103712/pdf
http://www.ncbi.nlm.nih.gov/pubmed/13575523?tool=bestpractice.com
[68]Bodonyi-Kovacs G, Lecker SH. Electrolyte-free water clearance: a key to the diagnosis of hypernatremia in resolving acute renal failure. Clin Exp Nephrol. 2008 Feb;12(1):74-8.
http://www.ncbi.nlm.nih.gov/pubmed/18180873?tool=bestpractice.com
[77]Ing TS, Lew SQ, Tzamaloukas AH, et al. Solute-free water excretion and electrolyte-free water excretion are better terms than solute-free water clearance and electrolyte-free water clearance. Int Urol Nephrol. 2021 Oct;53(10):2191-2.
http://www.ncbi.nlm.nih.gov/pubmed/33687641?tool=bestpractice.com
However, it does not provide a value for the total amount of free water needed to correct the hypernatremia.[78]Goldberg M. Hyponatremia. Med Clin N Am. 1981 Mar;65(2):251-69.
http://www.ncbi.nlm.nih.gov/pubmed/7230957?tool=bestpractice.com
A low value (<0.5 L/day) suggests inadequate free water intake, a high value (≥1 L/day) suggests large free water losses, while a very high value (>5 L/day) suggests diabetes insipidus.
The electrolyte-free water excretion value indicates how much electrolyte-free water is being lost through the urine at any given time.[64]Edelman IS, Leibman J, O'Meara MP, et al. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. J Clin Invest. 1958 Sep;37(9):1236-56.
https://www.jci.org/articles/view/103712/pdf
http://www.ncbi.nlm.nih.gov/pubmed/13575523?tool=bestpractice.com
[68]Bodonyi-Kovacs G, Lecker SH. Electrolyte-free water clearance: a key to the diagnosis of hypernatremia in resolving acute renal failure. Clin Exp Nephrol. 2008 Feb;12(1):74-8.
http://www.ncbi.nlm.nih.gov/pubmed/18180873?tool=bestpractice.com
[77]Ing TS, Lew SQ, Tzamaloukas AH, et al. Solute-free water excretion and electrolyte-free water excretion are better terms than solute-free water clearance and electrolyte-free water clearance. Int Urol Nephrol. 2021 Oct;53(10):2191-2.
http://www.ncbi.nlm.nih.gov/pubmed/33687641?tool=bestpractice.com
However, it does not provide a value for the total amount of free water needed to correct the hypernatremia.[78]Goldberg M. Hyponatremia. Med Clin N Am. 1981 Mar;65(2):251-69.
http://www.ncbi.nlm.nih.gov/pubmed/7230957?tool=bestpractice.com
A low value (<0.5 L/day) suggests inadequate free water intake, a high value (≥1 L/day) suggests large free water losses, while a very high value (>5 L/day) suggests diabetes insipidus.
Other investigations
A desmopressin challenge test should be ordered in patients with suspected diabetes insipidus. The result can be used to differentiate between central diabetes insipidus (where a lack of vasopressin, also known as arginine vasopressin [AVP] or antidiuretic hormone [ADH], responds to exogenous vasopressin administration) and nephrogenic diabetes insipidus. Patients with central diabetes insipidus will respond with decreased urine output and increased urine osmolality. Nephrogenic diabetes insipidus is diagnosed in a patient who is suspected of having diabetes insipidus who does not respond to exogenous vasopressin administration.
A serum AVP level may be useful to help distinguish central diabetes insipidus from nephrogenic diabetes insipidus as the level is low in patients with central diabetes insipidus.
Magnetic resonance imaging or computed tomography of the brain is recommended in patients with central diabetes insipidus to determine the underlying cause.
Other tests may be required, as determined by the history and exam, to evaluate the underlying cause, including serum creatine phosphokinase (CPK) level (may be helpful in hypernatremia associated with rhabdomyolysis), and renal ultrasound (in patients with renal disease).
Assessing dehydration in older patients
Stand-alone diagnostic tests (including bioelectrical impedance assessment of intracellular or extracellular water, dry mouth, feeling thirsty, fluid intake, heart rate, urine color, urine specific gravity, and urine volume) should not be relied upon to assess water-loss dehydration in older people.[79]Hooper L, Abdelhamid A, Attreed NJ, et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst Rev. 2015 Apr 30;(4):CD009647.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009647.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/25924806?tool=bestpractice.com
Individual tests lack specificity and/or sensitivity in this population.

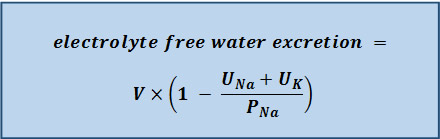 The electrolyte-free water excretion value indicates how much electrolyte-free water is being lost through the urine at any given time.[64][68][77] However, it does not provide a value for the total amount of free water needed to correct the hypernatremia.[78] A low value (<0.5 L/day) suggests inadequate free water intake, a high value (≥1 L/day) suggests large free water losses, while a very high value (>5 L/day) suggests diabetes insipidus.
The electrolyte-free water excretion value indicates how much electrolyte-free water is being lost through the urine at any given time.[64][68][77] However, it does not provide a value for the total amount of free water needed to correct the hypernatremia.[78] A low value (<0.5 L/day) suggests inadequate free water intake, a high value (≥1 L/day) suggests large free water losses, while a very high value (>5 L/day) suggests diabetes insipidus.