Etiology
Hypernatremia typically requires lack of access to water or impaired thirst mechanism. The main causes of hypernatremia can be broadly divided into the following categories.
Free water losses:
Osmotic diuresis/renal losses (e.g., recovery from renal failure, poorly controlled diabetes mellitus, use of intravenous mannitol or loop diuretics, recovery from obstructive uropathy, diabetes insipidus). One case report found severe hypernatremia in three patients with mixed diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome to be associated with excess carbohydrate beverage consumption.[27]
Gastrointestinal losses (e.g., severe diarrhea/prolonged vomiting, profuse diarrhea secondary to treatment with activated charcoal/sorbitol for poisoning, use of sodium polystyrene sulfonate/sorbitol in patients with hyperkalemia)[28][29]
Insensible or sweat losses (e.g., exercise, fever, heat exposure, burns) are unlikely to cause severe hypernatremia, but can contribute to worsening of hypernatremia
During peritoneal dialysis, when using dialysates that are high in dextrose (occurs in patients who are unable to drink water normally).[30]
Inadequate free water intake:
Inability to drink water or limited access to water (e.g., older patients with dementia)
Impaired thirst mechanism (e.g., primary hypodipsia due to brain tumors, congenital hypothalamic lesions, granulomatous disease, presence of subfornical organ-targeting antibody)[31][32][33]
It should be noted that all patients with hypernatremia have a deficit in free water intake; however, in the two settings described above, the only abnormality is the inability to drink water (or there is limited access to water) or an impaired thirst mechanism.
Sodium overload:
Administration of large volumes of hypertonic sodium bicarbonate solutions (e.g., patients with metabolic acidosis)[2] or hypertonic saline
Mineralocorticoid excess (e.g., Cushing syndrome, primary aldosteronism), although hypernatremia is typically mild and these patients usually have a concomitant abnormality in their access to water in order to develop significant hypernatremia
Intake of large amounts of salt (e.g., deliberate ingestion of household-strength bleach [sodium hypochlorite], inadvertent infusion with 5% saline [rather than 5% dextrose], sea water drowning [in survivors thereof], inappropriately high concentration of sodium bicarbonate or sodium chloride in dialysate for hemodialysis treatment, ingestion of bamboo salt [sea salt roasted in bamboo tubes], or massive intake of seasoning soy sauce or general excessive salt ingestion [usually in pediatric patients mistaking salt for sugar]).[2][29][34][35][36][37][38][39][Figure caption and citation for the preceding image starts]: Possible etiologies of hypernatremiaCreated by the BMJ Knowledge Centre [Citation ends].
Free water losses are the most common cause of hypernatremia. Generally speaking, inadequate free water intake is a less common cause; however, it can occur in older patients with dementia.[2] Patients with dementia who present with hypernatremia typically have a concomitant infection, are volume depleted, and have severe hypernatremia on admission to the hospital. Free water losses and inadequate free water intake can occur simultaneously. In addition to fluid imbalance in patients with infection, retrospective data suggest a possible role for sodium as an immune enhancer, such that inflammatory states (e.g., sepsis) may contribute multifactorially to hypernatremia.[22]
Altered thirst sensation without altered mental status is very rare, but has been described in pediatric patients and in two patients with advanced HIV infection plus cytomegalovirus encephalitis.[40] One study described three patients with adipsic hypernatremia attributed to the presence of antibodies to the subfornical organ of the brain. The subfornical organ is a circumventricular organ that forms a sensory interface between the blood and brain, and is a critical site for generating physiologic responses to dehydration and hyperosmolality.[33][40]
Hypernatremia associated with excessive sodium intake is not as common as hypernatremia due to free water losses. It usually occurs in hospitalized patients. The most common scenario is a patient with severe metabolic acidosis who is given multiple doses of hypertonic sodium bicarbonate (≥7%).[2][41]
Hypernatremia is more likely to occur in a hospital setting, and these patients are more likely to be hypervolemic (particularly if they have been treated in the intensive care unit), hypotensive, and have previously received large amounts of normal saline (0.9%).[6][7][8][11][41][42][43][44][45][46] There is often an association with large losses of urine or stool in this setting.[6][7][8][41][43][46] Often, there is co-existing renal disease (e.g., renal failure) with an inability to maximally concentrate urine, and osmotic diuresis may also play a large role.[6][7][8][12][41][47][48][49][50][51]
Diabetes insipidus is an uncommon cause of hypernatremia; typically, the patient's thirst mechanism is sufficiently intact to prevent the development of electrolyte abnormalities. There are two types of diabetes insipidus:
Nephrogenic:
Acquired: causes include specific drugs (e.g., lithium, demeclocycline, foscarnet, cisplatin, aminoglycosides, amphotericin B, penicillin derivatives, vitamin A or D excess, colchicine, vinblastine, vasopressin receptor antagonists, high-dose corticosteroids), sickle cell disease, amyloidosis, obstructive uropathy, other tubulointerstitial diseases, hypokalemia, and hypercalcemia.
[2][52][53][54][55][56][57][58] Dexmedetomidine, a sedative used prior to and/or during surgical procedures, has been reported to cause polyuria and urinary concentrating defect through an unknown mechanism, which may cause partial central or nephrogenic diabetes insipidus.[59]
Congenital: caused by a mutation in the gene for the vasopressin (V2) receptor in the majority of cases and is X-linked; however, a minority of patients have mutations in the aquaporin 2 collecting duct (AQP2) gene.[54]
Central (or hypothalamic):
Acquired: a history of traumatic brain injury or any other insult to the brain (e.g., vascular syndromes, infections, tumors, or aggressive surgery for craniopharyngioma, Rathke cleft cyst, or other hypothalamic tumors) is often present.[2] Temozolomide (a chemotherapy agent) has been reported to cause central diabetes insipidus, as have phenytoin, immune checkpoint inhibitors, and ethanol.[56][60][61][62] Central diabetes insipidus has also been linked to acute myelogenous leukemia.[63]
Congenital: this is rare.
Pathophysiology
Hypernatremia represents a deficit of water relative to sodium, and most commonly occurs when free water losses are not replaced by increased intake.
Hypernatremia is generally associated with large fluid losses (usually via urine), as the sodium plus potassium concentration of most body fluids is often significantly less than the sodium concentration of serum. Therefore, electrolyte-free water excretion is high and serum sodium concentration increases unless water intake is increased to match the water loss. However, many of these patients are still hypervolemic despite a high urine output because they have previously received large volumes of normal saline and are massively edematous.[6][7][8][45]
Both diarrhea and urinary loss can result in hypernatremia. In the case of urinary loss, electrolyte-free water excretion (also known as electrolyte-free water clearance) is calculated using the following equation.[Figure caption and citation for the preceding image starts]: Electrolyte-free water excretion formula. V = urine flow rate. UNa = urine concentration of sodium (mEq/L). UK = urine concentration of potassium (mEq/L). PNa = plasma concentration of sodium (mEq/L)Created by the BMJ Knowledge Centre [Citation ends].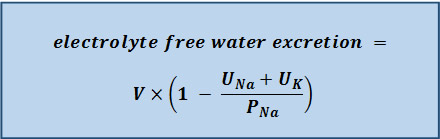 This formula is derived from Edelman’s equation, which showed the importance of total body sodium and potassium in determining serum sodium concentration.[64]
This formula is derived from Edelman’s equation, which showed the importance of total body sodium and potassium in determining serum sodium concentration.[64]
Electrolyte-free water excretion can be a positive or negative value:[55]
UNa + UK < PNa: electrolyte-free water excretion is positive, a process that will tend to raise the serum sodium concentration
UNa + UK > PNa: electrolyte-free water excretion is negative, a process that will tend to lower the serum sodium concentration
where UNa = urine concentration of sodium; UK = urine concentration of potassium; PNa = plasma concentration of sodium.
People with normal renal function who receive large amounts of saline can concentrate their urine to excrete the sodium load that they have been given and, therefore, have very little electrolyte-free water excretion. However, patients who are unable to concentrate their urine, as is the case in kidney dysfunction or diabetes insipidus, cannot excrete the extra sodium load and may develop hypernatremia.[2][41][65]
In acute hypernatremia (generally defined as onset within <48 hours), the higher osmolality in the extracellular space causes water to move out of brain cells causing the brain to shrink. This shrinkage can lead to neurological consequences, including lethargy, weakness, and irritability. If severe, adverse manifestations can include intracranial hemorrhage, seizures, stupor, coma, and death.[2][66] Chronic hypernatremia (generally defined as onset over ≥48 hours) leads to fewer changes in brain cell volume as the brain cells can adapt to the chronic hyperosmolality by increasing intracellular osmolality. Brain cells do this by first accumulating sodium chloride and potassium chloride, and later by increasing intracellular brain solutes such as glutamate, taurine, and myoinositol.[66][67]
In central diabetes insipidus, there is a lack of vasopressin (also known as arginine vasopressin [AVP] or antidiuretic hormone [ADH]) due to a congenital or acquired condition that impairs vasopressin synthesis. However, in nephrogenic diabetes insipidus, the kidneys do not respond appropriately to vasopressin secretion.
Patients with hypernatremia often have a high blood urea nitrogen (BUN) and/or creatinine level. The high BUN level may worsen the hypernatremia by causing an osmotic diuresis. As a result, the amounts of sodium and potassium excreted in the urine will be relatively small (i.e., UNa + UK < PNa), thus bringing about an increase in electrolyte-free water excretion.[51][68]
Classification
Serum sodium concentration
Hypernatremia: >145 mEq/L
Severe hypernatremia has variously been defined as a serum sodium concentration of >152 mEq/L, >155 mEq/L, or >160 mEq/L.[2][3][4] However, there is no consensus as to the exact level.
Time of onset
Patients with hypernatremia that has developed slowly (e.g., over days, weeks, or months) are commonly asymptomatic, while patients with hypernatremia that has developed rapidly (e.g., over a few hours) will be symptomatic. Hypernatremia that develops in <48 hours is usually classified as acute, while hypernatremia that develops over ≥48 hours is chronic.
Total body sodium content
Low total body sodium content:
Both intracellular and extracellular fluid spaces are decreased, while total body sodium is also decreased. Patients usually present to the hospital (rather than already being hospitalized) and volume expansion is necessary to correct the volume depletion.[5] Also known as hypovolemic hypernatremia.
High total body sodium content:
Extracellular fluid volume is expanded and intracellular space is decreased, while total body sodium is high. May be the most common cause of hypernatremia in patients who develop hypernatremia in the hospital. Salt should be restricted and water should be given to correct the sodium abnormality.[6][7][8] Also known as hypervolemic hypernatremia.
Normal total body sodium content:
Extracellular and intracellular fluid spaces are decreased (much less than the reductions in patients with hypernatremia due to low total body sodium content). Total body sodium is normal. Probably uncommon; however evidence is lacking.[2] Also known as euvolemic hypernatremia.
Use of this content is subject to our disclaimer