The diagnosis of NS is typically made clinically. It is a clinically heterogeneous disorder.
A thorough history of the pregnancy, family, and individual, followed by a meticulous physical exam, with particular attention to the features of the head and face, neck, and chest, are usually diagnostic. If NS is suspected, the patient should be investigated for coagulation and cardiac abnormalities, which are common.
Genetic testing may be necessary when the diagnosis is equivocal, or for family reasons (e.g., parental diagnosis, determination of the risk for recurrence, or reproductive planning).
History
Pregnancy and perinatal history
Family history
When there is no known history of NS in a close relative, it is important to inquire about relatives with short stature, congenital heart disease, and learning difficulties.
Feeding
Feeding difficulties occur in approximately 77% of infants. They include poor sucking with prolonged feeding time, slow feeding with recurrent vomiting, or severe feeding problems requiring tube-feeding for ≥2 weeks.[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
[30]Shaw AC, Kalidas K, Crosby AH, et al. The natural history of Noonan syndrome: a long-term follow-up study. Arch Dis Child. 2007 Feb;92(2):128-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083343
http://www.ncbi.nlm.nih.gov/pubmed/16990350?tool=bestpractice.com
[31]Shah N, Rodriguez M, St Louis D, et al. Feeding difficulties and foregut dysmotility in Noonan's syndrome. Arch Dis Child. 1999 Jul;81(1):28-31.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1717976
http://www.ncbi.nlm.nih.gov/pubmed/10373129?tool=bestpractice.com
The feeding difficulties are usually related to hypotonia (low muscle tone) and poor coordination of oral musculature. However, immature gut motility and delayed GI motor development have been documented in some cases.[31]Shah N, Rodriguez M, St Louis D, et al. Feeding difficulties and foregut dysmotility in Noonan's syndrome. Arch Dis Child. 1999 Jul;81(1):28-31.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1717976
http://www.ncbi.nlm.nih.gov/pubmed/10373129?tool=bestpractice.com
Failure to thrive can occur in up to 40% of neonates. This is self-limited, however, and usually resolves by 18 months of age.[30]Shaw AC, Kalidas K, Crosby AH, et al. The natural history of Noonan syndrome: a long-term follow-up study. Arch Dis Child. 2007 Feb;92(2):128-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083343
http://www.ncbi.nlm.nih.gov/pubmed/16990350?tool=bestpractice.com
Growth
The growth history is important. While birth length is generally normal, childhood growth tends to follow the third centile, with an attenuated or absent pubertal growth spurt.[32]Witt DR, Keena BA, Hall JG, et al. Growth curves for height in Noonan syndrome. Clin Genet. 1986 Sep;30(3):150-3.
http://www.ncbi.nlm.nih.gov/pubmed/3780030?tool=bestpractice.com
Puberty
Pubertal delay is relatively more common in boys than girls.[33]Elsawi MM, Pryor JP, Klufio G, et al. Genital tract function in men with Noonan syndrome. J Med Genet. 1994 Jun;31(6):468-70.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1049925
http://www.ncbi.nlm.nih.gov/pubmed/7915331?tool=bestpractice.com
Inquiry should be made about undescended testes in boys at birth.
Development
Mild cognitive impairment is observed in a subset of individuals with NS. IQ typically ranges from 64 to 127.[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
[34]Allanson JE. Noonan syndrome. J Med Genet. 1987 Jan;24(1):9-13.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1049850
http://www.ncbi.nlm.nih.gov/pubmed/3543368?tool=bestpractice.com
About 50% of patients will show mild to moderate clumsiness and coordination problems.
There is a 25% likelihood of a learning disability with specific visual-constructional problems, verbal-performance discrepancy, and language delay/impairment.[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
[35]Lee DA, Portnoy S, Hill P, et al. Psychological profile of children with Noonan syndrome. Dev Med Child Neurol. 2005 Jan;47(1):35-8.
http://www.ncbi.nlm.nih.gov/pubmed/15686287?tool=bestpractice.com
[36]Sarimski K. Developmental and behavioural phenotype in Noonan syndrome? Genet Couns. 2000;11(4):383-90.
http://www.ncbi.nlm.nih.gov/pubmed/11140417?tool=bestpractice.com
[37]Pierpont EI, Weismer SE, Roberts AE, et al. The language phenotype of children and adolescents with Noonan syndrome. J Speech Lang Hear Res. 2010 Aug;53(4):917-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3086511
http://www.ncbi.nlm.nih.gov/pubmed/20543023?tool=bestpractice.com
Children with NS have a specific impairment in the global processing of visuospatial information.[38]Alfieri P, Cesarini L, De Rose P, et al. Visual processing in Noonan syndrome: dorsal and ventral stream sensitivity. Am J Med Genet A. 2011 Oct;155A(10):2459-64.
http://www.ncbi.nlm.nih.gov/pubmed/21910245?tool=bestpractice.com
Adults with NS may experience specific difficulties in information processing, but this rarely has an impact on cognition.[39]Wingbermühle E, Roelofs RL, van der Burgt I, et al. Cognitive functioning of adults with Noonan syndrome: a case-control study. Genes Brain Behav. 2012 Oct;11(7):785-93.
http://onlinelibrary.wiley.com/doi/10.1111/j.1601-183X.2012.00821.x/full
http://www.ncbi.nlm.nih.gov/pubmed/22783933?tool=bestpractice.com
Strengths include verbal comprehension, abstract reasoning, and social awareness and judgment.[40]Singer ST, Hurst D, Addiego JE Jr. Bleeding disorders in Noonan syndrome: three case reports and review of the literature. J Pediatr Hematol Oncol. 1997 Mar-Apr;19(2):130-4.
http://www.ncbi.nlm.nih.gov/pubmed/9149742?tool=bestpractice.com
Weaknesses include inability to organize perceptual information, lack of planning abilities, and lack of spatial knowledge.
Increased bruising or bleeding
Many patients may report easy bruising.[41]Sharland M, Patton MA, Talbot S, et al. Coagulation-factor deficiencies and abnormal bleeding in Noonan's syndrome. Lancet. 1992 Jan 4;339(8784):19-21.
http://www.ncbi.nlm.nih.gov/pubmed/1345952?tool=bestpractice.com
Mild-to-moderate bleeding tendency is not uncommon.[42]van der Burgt I. Noonan syndrome. Orphanet J Rare Dis. 2007 Jan 14;2:4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1781428
http://www.ncbi.nlm.nih.gov/pubmed/17222357?tool=bestpractice.com
Severe hemorrhage has been reported to occur in 3% of cases.
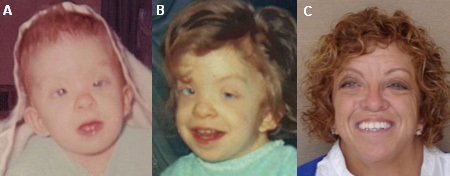
Physical exam
Examination of the head and face may be the most diagnostically important part of the exam, as particular facial characteristics are common, although they change with age.[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
[34]Allanson JE. Noonan syndrome. J Med Genet. 1987 Jan;24(1):9-13.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1049850
http://www.ncbi.nlm.nih.gov/pubmed/3543368?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Young male with Noonan syndrome, seen at age 3 months (A), 2 years (B), 6 years (C), and 17 years (D)From the collection of Judith E. Allanson [Citation ends]. The facial features of NS are often subtle, but perhaps most florid in newborns and adolescents. These features are difficult to recognize in adults, and many adults are only diagnosed after the birth of a child with more obvious features.
The facial features of NS are often subtle, but perhaps most florid in newborns and adolescents. These features are difficult to recognize in adults, and many adults are only diagnosed after the birth of a child with more obvious features.
Head and face
The newborn has a tall forehead, wide-spaced and down-slanting eyes, epicanthal folds, a depressed nasal root with upturned nasal tip, a deeply grooved philtrum (depression between nose and lips) with high, wide peaks of the vermilion (resembling a cupid's bow), high-arched palate, small chin, low-set and posteriorly angulated ears with thick helices, and excessive neck skin with low posterior hairline.
During infancy, the head seems relatively large, with a tall and prominent forehead. Ptosis or thick, hooded eyelids are characteristic. The nose is short and wide, with a depressed root.
In later childhood, the face may appear coarse, hypotonic, or myopathic, as it has rounded features and little expression. Facial shape becomes more triangular with age, as the face lengthens. The patient may have sparse or absent eyebrows and lashes.
In the adolescent and young adult, the nose has a narrow and prominent bridge and a wide base. The neck is longer, with accentuated webbing (pterygium colli) or a prominent trapezius muscle.
In older adults, unusually prominent nasolabial folds and thin, transparent skin are present.[34]Allanson JE. Noonan syndrome. J Med Genet. 1987 Jan;24(1):9-13.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1049850
http://www.ncbi.nlm.nih.gov/pubmed/3543368?tool=bestpractice.com
Mean adult head circumference in males is 22.2 inches (56.4 cm), and in females is 21.6 inches (54.9 cm).[30]Shaw AC, Kalidas K, Crosby AH, et al. The natural history of Noonan syndrome: a long-term follow-up study. Arch Dis Child. 2007 Feb;92(2):128-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083343
http://www.ncbi.nlm.nih.gov/pubmed/16990350?tool=bestpractice.com
Hair may be wispy and sparse or curly, thick, and wooly.[34]Allanson JE. Noonan syndrome. J Med Genet. 1987 Jan;24(1):9-13.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1049850
http://www.ncbi.nlm.nih.gov/pubmed/3543368?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Female with Noonan syndrome seen at age 4 months (A), 4 years (B), and as an adult (C)From the collection of Judith E. Allanson [Citation ends].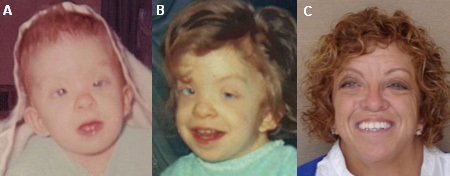
Eyes
Ocular findings are among the most common features of NS, and observed in up to 95% of cases.
They include strabismus (crossed eyes), refractive errors, amblyopia (lazy eye), ptosis, and nystagmus (involuntary eye movement).
Anterior segment changes, such as prominent corneal nerves, anterior stromal dystrophy, cataracts, and panuveitis, have been reported.
Fundal changes are less frequent, and include optic head drusen, optic disk hypoplasia, colobomas, and myelinated nerves.[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
[30]Shaw AC, Kalidas K, Crosby AH, et al. The natural history of Noonan syndrome: a long-term follow-up study. Arch Dis Child. 2007 Feb;92(2):128-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083343
http://www.ncbi.nlm.nih.gov/pubmed/16990350?tool=bestpractice.com
[43]van Trier DC, van der Burgt I, Draaijer RW, et al. Ocular findings in Noonan syndrome: a retrospective cohort study of 105 patients. Eur J Pediatr. 2018 Aug;177(8):1293-98.
https://www.doi.org/10.1007/s00431-018-3183-1
http://www.ncbi.nlm.nih.gov/pubmed/29948256?tool=bestpractice.com
The iris is often vivid blue or blue-green, and frequently out of keeping with familial eye color, providing an excellent diagnostic clue.
Musculoskeletal system
A particular pectus deformity, with pectus carinatum superiorly and pectus excavatum inferiorly, is noted in 70% to 95% of cases. [Figure caption and citation for the preceding image starts]: Chest demonstrating typical pectus deformity with a marked inferior excavatum and subtle superior carinatumFrom the collection of Judith E. Allanson [Citation ends].
The thorax is broad, with widely spaced nipples. During childhood, the upper chest appears long; nipples appear low-set, and there is axillary webbing, which persists into adulthood. Shoulders may be rounded, probably because of hypotonic posturing.
Cubitus valgus (an increased carrying angle of the forearm) is present in 50% of cases, and short fingers with blunt fingertips are seen in up to one third of cases. Joint hyperextensibility occurs in 30% of cases.[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
Less common skeletal anomalies include talipes equinovarus (clubfoot), joint contractures, scoliosis, and radioulnar synostosis (fusion of radius and ulna).
Muscle weakness as measured by grip strength has been documented.[44]Stevenson DA, Allen S, Tidyman WE, et al. Peripheral muscle weakness in RASopathies. Muscle Nerve. 2012 Sep;46(3):394-9.
http://www.ncbi.nlm.nih.gov/pubmed/22907230?tool=bestpractice.com
Cardiovascular system
Congenital heart defects may occur in up to 75% of cases.[1]Jorge AA, Malaquias AC, Arnhold IJ, et al. Noonan syndrome and related disorders: a review of clinical features and mutations in genes of the RAS/MAPK pathway. Horm Res. 2009;71(4):185-93.
https://www.karger.com/Article/FullText/201106
http://www.ncbi.nlm.nih.gov/pubmed/19258709?tool=bestpractice.com
The most common anomaly is a dysplastic and/or stenotic pulmonary valve, noted in 50% to 65% of affected children.[30]Shaw AC, Kalidas K, Crosby AH, et al. The natural history of Noonan syndrome: a long-term follow-up study. Arch Dis Child. 2007 Feb;92(2):128-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083343
http://www.ncbi.nlm.nih.gov/pubmed/16990350?tool=bestpractice.com
Congenital structural heart defects and hypertrophic cardiomyopathy may present in the prenatal period, the newborn period, or later in childhood.
Skin
Pigmentary changes such as café au lait spots, pigmented nevi, and lentigines may be seen.
Adults may show difficulty in growing a beard, due to keratosis pilaris atrophicans faciei (small, scarlike depressions in the face).[45]Pierini DO, Pierini AM. Keratosis pilaris atrophicans faciei (ulerythema ophryogenes): a cutaneous marker in the Noonan syndrome. Br J Dermatol. 1979 Apr;100(4):409-16.
http://www.ncbi.nlm.nih.gov/pubmed/454568?tool=bestpractice.com
Pregnant women
During pregnancy, the most common features suggesting a diagnosis are polyhydramnios (excess of amniotic fluid) and cystic hygroma (cystic lymphatic lesion).[29]Sharland M, Burch M, McKenna WM, et al. A clinical study of Noonan syndrome. Arch Dis Child. 1992 Feb;67(2):178-83.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793396
http://www.ncbi.nlm.nih.gov/pubmed/1543375?tool=bestpractice.com
[46]Achiron R, Heggesh J, Grisaru D, et al. Noonan syndrome: a cryptic condition in early gestation. Am J Med Genet. 2000 May 29;92(3):159-65.
http://www.ncbi.nlm.nih.gov/pubmed/10817648?tool=bestpractice.com
[47]Benacerraf BR, Greene MF, Holmes LB. The prenatal sonographic features of Noonan's syndrome. J Ultrasound Med. 1989 Feb;8(2):59-63.
http://www.ncbi.nlm.nih.gov/pubmed/2651692?tool=bestpractice.com
[48]Houweling AC, de Mooij YM, van der Burgt I, et al. Prenatal detection of Noonan syndrome by mutation analysis of the PTPN11 and the KRAS genes. Prenat Diagn. 2010 Mar;30(3):284-6.
http://www.ncbi.nlm.nih.gov/pubmed/20112233?tool=bestpractice.com
Other features noted on ultrasound include scalp edema, increased nuchal translucency, pleural or pericardial effusion, ascites, and/or hydrops (abnormal accumulation of fluid in body cavities).[46]Achiron R, Heggesh J, Grisaru D, et al. Noonan syndrome: a cryptic condition in early gestation. Am J Med Genet. 2000 May 29;92(3):159-65.
http://www.ncbi.nlm.nih.gov/pubmed/10817648?tool=bestpractice.com
[49]Bawle EV, Black V. Nonimmune hydrops fetalis in Noonan's syndrome. Am J Dis Child. 1986 Aug;140(8):758-60.
http://www.ncbi.nlm.nih.gov/pubmed/3728401?tool=bestpractice.com
Splenomegaly
Enlargement of the spleen has been observed and may be a feature of myelodysplasia.[40]Singer ST, Hurst D, Addiego JE Jr. Bleeding disorders in Noonan syndrome: three case reports and review of the literature. J Pediatr Hematol Oncol. 1997 Mar-Apr;19(2):130-4.
http://www.ncbi.nlm.nih.gov/pubmed/9149742?tool=bestpractice.com
Renal malformations
Found in up to 10% of cases, these features include malformations such as duplex collecting system, distal ureteric stenosis, renal hypoplasia, unilateral renal agenesis, and unilateral renal ectopia.[50]George CD, Patton MA, El Sawi M, et al. Abdominal ultrasound in Noonan syndrome: a study of 44 patients. Pediatr Radiol. 1993;23(4):316-8.
http://www.ncbi.nlm.nih.gov/pubmed/8414765?tool=bestpractice.com
Diagnostic criteria: scoring systems
Several scoring systems have been devised to help the diagnostic process.[42]van der Burgt I. Noonan syndrome. Orphanet J Rare Dis. 2007 Jan 14;2:4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1781428
http://www.ncbi.nlm.nih.gov/pubmed/17222357?tool=bestpractice.com
[51]Duncan WJ, Fowler RS, Farkas LG, et al. A comprehensive scoring system for evaluating Noonan syndrome. Am J Med Genet. 1981;10(1):37-50.
http://www.ncbi.nlm.nih.gov/pubmed/7294061?tool=bestpractice.com
The most recent scoring system was developed in 1994.[42]van der Burgt I. Noonan syndrome. Orphanet J Rare Dis. 2007 Jan 14;2:4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1781428
http://www.ncbi.nlm.nih.gov/pubmed/17222357?tool=bestpractice.com
In this system, NS is defined as typical facial features plus 1 major or 2 minor clinical characteristics, or suggestive facial features plus 2 major or 3 minor clinical characteristics. However, the typical facial features can be subtle and often require evaluation from an experienced dysmorphologist. Molecular testing for mutations in the genes known to cause NS may be required if the diagnosis is in question.
Major characteristics
Cardiac: pulmonary valve stenosis and/or typical ECG
Height: <third centile
Chest wall: pectus carinatum/excavatum
Family history: first-degree relative with definite diagnosis
Cognitive impairment, cryptorchidism, lymphatic dysplasia: all 3 present.
Minor characteristics
Cardiac: other defects than those described as major characteristics
Height: <tenth centile; short stature may be present at birth or postnatal in origin
Chest: broad thorax
Family: first-degree relative with suggestive diagnosis
Cognitive impairment, cryptorchidism, lymphatic dysplasia: any of the 3 present.
Laboratory investigations
Reports have documented multiple types of coagulation defects and bleeding diatheses in NS, and a wide range of clinical presentations.[52]Derbent M, Oncel Y, Tokel K, et al. Clinical and hematologic findings in Noonan syndrome patients with PTPN11 gene mutations. Am J Med Genet A. 2010 Nov;152A(11):2768-74.
http://www.ncbi.nlm.nih.gov/pubmed/20954246?tool=bestpractice.com
If NS is suspected, the patient should be screened for coagulation abnormalities. Initially, a CBC with platelet count and coagulation profile (i.e., prothrombin time, activated partial thromboplastin time, bleeding time) can be considered.[53]Briggs BJ, Dickerman JD. Bleeding disorders in Noonan syndrome. Pediatr Blood Cancer. 2012 Feb;58(2):167-72.
http://www.ncbi.nlm.nih.gov/pubmed/22012616?tool=bestpractice.com
Males with evidence of pubertal delay should have an evaluation of testicular function as Sertoli cell dysfunction has been described.[54]Marcus KA, Sweep CG, van der Burgt I, et al. Impaired Sertoli cell function in males diagnosed with Noonan syndrome. J Pediatr Endocrinol Metab. 2008 Nov;21(11):1079-84.
http://www.ncbi.nlm.nih.gov/pubmed/19189703?tool=bestpractice.com
Other investigations
ECG and echocardiogram
Congenital heart defects are present in up to 75% of cases, so a thorough cardiovascular exam should be performed.[1]Jorge AA, Malaquias AC, Arnhold IJ, et al. Noonan syndrome and related disorders: a review of clinical features and mutations in genes of the RAS/MAPK pathway. Horm Res. 2009;71(4):185-93.
https://www.karger.com/Article/FullText/201106
http://www.ncbi.nlm.nih.gov/pubmed/19258709?tool=bestpractice.com
An ECG and echocardiogram should identify the features of the most common cardiac anomalies (i.e., dysplastic and/or stenotic pulmonary valve, hypertrophic cardiomyopathy, septal defects, and tetralogy of Fallot).[30]Shaw AC, Kalidas K, Crosby AH, et al. The natural history of Noonan syndrome: a long-term follow-up study. Arch Dis Child. 2007 Feb;92(2):128-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083343
http://www.ncbi.nlm.nih.gov/pubmed/16990350?tool=bestpractice.com
[55]Burch M, Sharland M, Shinebourne E, et al. Cardiologic abnormalities in Noonan syndrome: phenotypic diagnosis and echocardiographic assessment of 118 patients. J Am Coll Cardiol. 1993 Oct;22(4):1189-92.
http://www.sciencedirect.com/science/article/pii/0735109793904365?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/8409059?tool=bestpractice.com
[56]Ishizawa A, Oho S, Dodo H, et al. Cardiovascular abnormalities in Noonan syndrome: the clinical findings and treatments. Acta Paediatr Jpn. 1996 Feb;38(1):84-90.
http://www.ncbi.nlm.nih.gov/pubmed/8992869?tool=bestpractice.com
[57]Noonan JA, O'Connor W. Noonan syndrome: a clinical description emphasizing the cardiac findings. Acta Paediatr Jpn. 1996;38:76-83.
http://www.ncbi.nlm.nih.gov/pubmed/8992867?tool=bestpractice.com
Molecular genetic testing
This may be necessary when the diagnosis is equivocal, or for family reasons (e.g., parental diagnosis, determination of the risk for recurrence, or reproductive planning).
Clinical diagnostic testing for the genes in the Ras/MAPK pathway known to cause NS is available. However, a proportion of people with NS will not have a mutation in any of the genes currently known to cause this condition.
PTPN11 mutations are found in 50% to 60% of affected individuals.[11]Tartaglia M, Mehler EL, Goldberg R, et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet. 2001 Dec;29(4):465-8.
http://www.ncbi.nlm.nih.gov/pubmed/11704759?tool=bestpractice.com
[12]Tartaglia M, Kalidas K, Shaw A, et al. PTPN11 mutations in Noonan syndrome: molecular spectrum, genotype-phenotype correlation, and phenotypic heterogeneity. Am J Hum Genet. 2002 Jun;70(6):1555-63.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC379142
http://www.ncbi.nlm.nih.gov/pubmed/11992261?tool=bestpractice.com
SOS1 mutations are found in approximately 10% to 15% of cases.[3]Roberts AE, Araki T, Swanson KD, et al. Germline gain-of-function mutations in SOS1 cause Noonan syndrome. Nat Genet. 2007 Jan;39(1):70-4.
http://www.ncbi.nlm.nih.gov/pubmed/17143285?tool=bestpractice.com
[4]Tartaglia M, Pennacchio LA, Zhao C, et al. Gain-of-function SOS1 mutations cause a distinctive form of Noonan syndrome. Nat Genet. 2007 Jan;39(1):75-9.
http://www.ncbi.nlm.nih.gov/pubmed/17143282?tool=bestpractice.com
RAF1 mutations are found in approximately 5% of cases.[5]Pandit B, Sarkozy A, Pennacchio LA, et al. Gain-of-function RAF1 mutations cause Noonan and LEOPARD syndromes with hypertrophic cardiomyopathy. Nat Genet. 2007 Aug;39(8):1007-12.
http://www.ncbi.nlm.nih.gov/pubmed/17603483?tool=bestpractice.com
[6]Razzaque MA, Nishizawa T, Komoike Y, et al. Germline gain-of-function mutations in RAF1 cause Noonan syndrome. Nat Genet. 2007 Aug;39(8):1013-7.
http://www.ncbi.nlm.nih.gov/pubmed/17603482?tool=bestpractice.com
KRAS mutations are found in approximately 1% of cases.[7]Schubbert S, Zenker M, Rowe SL, et al. Germline KRAS mutations cause Noonan syndrome. Nat Genet. 2006 Mar;38(3):331-6.
http://www.ncbi.nlm.nih.gov/pubmed/16474405?tool=bestpractice.com
[16]Carta C, Pantaleoni F, Bocchinfuso G, et al. Germline missense mutations affecting KRAS isoform B are associated with a severe Noonan syndrome phenotype. Am J Hum Genet. 2006 Jul;79(1):129-35.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1474118
http://www.ncbi.nlm.nih.gov/pubmed/16773572?tool=bestpractice.com
Rarely, mutations in other genes (e.g., NRAS, BRAF, or MAP2K1) will be identified.[8]Cirstea IC, Kutsche K, Dvorsky R, et al. A restricted spectrum of NRAS mutations causes Noonan syndrome. Nat Genet. 2010 Jan;42(1):27-9.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3118669
http://www.ncbi.nlm.nih.gov/pubmed/19966803?tool=bestpractice.com
[9]Nyström AM, Ekvall S, Berglund E, et al. Noonan and cardio-facio-cutaneous syndromes: two clinically and genetically overlapping disorders. J Med Genet. 2008 Aug;45(8):500-6.
http://www.ncbi.nlm.nih.gov/pubmed/18456719?tool=bestpractice.com
[10]Sarkozy A, Carta C, Moretti S, et al. Germline BRAF mutations in Noonan, LEOPARD, and cardiofaciocutaneous syndromes: molecular diversity and associated phenotypic spectrum. Hum Mutat. 2009 Apr;30(4):695-702.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4028130
http://www.ncbi.nlm.nih.gov/pubmed/19206169?tool=bestpractice.com
Mutation "hotspots" are observed in some of these genes.
Some laboratories suggest testing in a tiered manner, beginning with the PTPN11 hotspots (serial single gene testing). Other laboratories use a multigene panel that simultaneously tests for all genes known to cause Noonan syndrome.
If there are existing genetic test results, do not perform repeat testing unless there is uncertainty about the existing result, e.g., the result is inconsistent with the patient’s clinical presentation or the test methodology has changed.[58]American College of Medical Genetics and Genomics. Five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2021 [internet publication].
https://web.archive.org/web/20230326143738/https://www.choosingwisely.org/societies/american-college-of-medical-genetics-and-genomics
In pregnancies complicated by cystic hygroma, increased nuchal translucency, or hydrops, where chromosome analysis is normal, PTPN11 mutations are found in 3% to 11% of cases, depending on the ultrasound finding.[48]Houweling AC, de Mooij YM, van der Burgt I, et al. Prenatal detection of Noonan syndrome by mutation analysis of the PTPN11 and the KRAS genes. Prenat Diagn. 2010 Mar;30(3):284-6.
http://www.ncbi.nlm.nih.gov/pubmed/20112233?tool=bestpractice.com
[59]Lee KA, Williams B, Roza K, et al. PTPN11 analysis for the prenatal diagnosis of Noonan syndrome in fetuses with abnormal ultrasound findings. Clin Genet. 2009 Feb;75(2):190-4.
http://www.ncbi.nlm.nih.gov/pubmed/18759865?tool=bestpractice.com
Abdominal ultrasound
This should be performed if enlargement of the spleen is suspected. Splenomegaly may be a feature of myelodysplasia.[40]Singer ST, Hurst D, Addiego JE Jr. Bleeding disorders in Noonan syndrome: three case reports and review of the literature. J Pediatr Hematol Oncol. 1997 Mar-Apr;19(2):130-4.
http://www.ncbi.nlm.nih.gov/pubmed/9149742?tool=bestpractice.com
Renal ultrasound
This should be performed if renal malformation is suspected (e.g., malformations such as duplex collecting system, distal ureteric stenosis, renal hypoplasia, unilateral renal agenesis, or unilateral renal ectopia); such malformations may be present in up to 10% of cases.[50]George CD, Patton MA, El Sawi M, et al. Abdominal ultrasound in Noonan syndrome: a study of 44 patients. Pediatr Radiol. 1993;23(4):316-8.
http://www.ncbi.nlm.nih.gov/pubmed/8414765?tool=bestpractice.com
 The facial features of NS are often subtle, but perhaps most florid in newborns and adolescents. These features are difficult to recognize in adults, and many adults are only diagnosed after the birth of a child with more obvious features.
The facial features of NS are often subtle, but perhaps most florid in newborns and adolescents. These features are difficult to recognize in adults, and many adults are only diagnosed after the birth of a child with more obvious features.