Approach
The diagnosis of mastitis and/or breast infection warrants a detailed history to include potential risk factors, along with a thorough physical examination. While the diagnosis of breast infection is usually made on clinical grounds, investigations may be necessary in certain cases.
Presence of risk factors
Elicit the presence of any risk factors for mastitis or breast abscess. Risk factors strongly associated with mastitis include:[1][2][5][16][19][22][23]
Female sex
Lactation, particularly after 6-8 weeks of breast-feeding or at weaning
Poor breast-feeding technique (may also be due to infant factors such as tongue-tie, also known as ankyloglossia)
Milk stasis (may be secondary to poor breast-feeding technique or tight-fitting bra)
Nipple injury
Previous mastitis
Shaving or plucking areolar hair
Anatomic breast defect, mammoplasty, or scar
Other underlying breast condition, particularly breast cancer
Nipple piercing
Foreign body (e.g., silicone implant)
Skin infection
Positive carrier status for Staphylococcus aureus
Immunosuppression (including diabetes mellitus).
Risk factors strongly associated with breast abscess include ages >30 years, prolonged mastitis and prior breast abscess.
Focused history
A focused history needs to evaluate for:
Symptoms related to possible breast inflammation (e.g., warmth, pain, swelling, firmness, erythema)
Possible abscess (tender lump)
Milk stasis (decreased milk output)
Systemic infection (fever, malaise, myalgia)
Nipple discharge, which may be present with mastitis and occurs more often with duct ectasia (dilated ducts with inflammation); however, purulent discharge is usually indicative of breast infection.
Physical examination
The diagnosis of breast infection is usually made on clinical grounds. General physical examination includes:
Recording the patient's temperature: mastitis may occur with or without pyrexia of >100.4°F (>38°C); breast abscess may or may not be accompanied by fever.
Checking for other signs of systemic infection (e.g., flu-like illness, possible extramammary skin lesions)
Examining for distant skin infections
Checking for possible extramammary tuberculosis (TB) infection, including signs of pleural-pulmonary disease, lymphadenitis, and erythema nodosum.
Breast examination consists of a thorough examination of both breasts and axillary lymph nodes:
Tender axillary lymph nodes may occur with ipsilateral breast infection.
Signs of breast inflammation include breast tenderness, warmth, firmness, swelling, and erythema.
Lactational mastitis tends to involve more peripheral wedge-shaped areas of the breast.
A tender palpable breast mass may indicate localized mastitis or breast abscess.
A fluctuant mass may be palpated in the case of a late breast abscess.
Rarely, nipple retraction or inversion may occur with mastitis.
If a fistula is present, it is usually associated with a draining sinus from an underlying abscess.
Initial investigations
If mastitis develops unexpectedly, such as in an adolescent, a pregnancy test should be considered.
Ultrasonography of an erythematous breast area may help in the initial workup to diagnose an underlying abscess and can direct needle aspiration drainage.[5][30] An abscess may appear as a well-circumscribed, macrolobulated, irregular, or ill-defined echo-poor compound cystic lesion with possible septae.[5][30] A hypoechoic rim may indicate a thick wall of a chronic abscess. [Figure caption and citation for the preceding image starts]: Ultrasound image showing a well-circumscribed hypoechoic breast abscessFrom the collection of Holly S. Mason, MD, Tufts University School of Medicine, MA [Citation ends].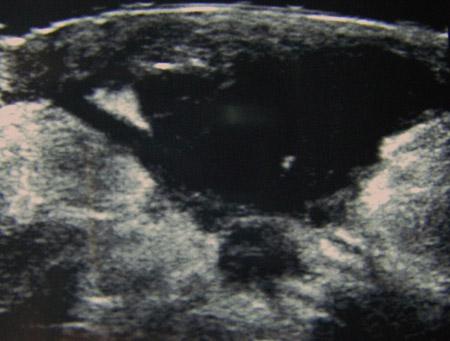
A breast abscess can be drained by needle aspiration for therapeutic and diagnostic purposes.[30] Aspirated material (fluid, pus, blood) from needle drainage of an abscess should be sent for microbiology studies and cytology to look for underlying malignancy in addition to infection. [Figure caption and citation for the preceding image starts]: Needle aspiration of a breast abscess under ultrasound guidance: note the needle piercing the abscess to the right of the imageFrom the collection of Holly S. Mason, MD, Tufts University School of Medicine, MA [Citation ends].
Microbiology and pathology investigations
For routine cases of mastitis, a biopsy is not necessarily indicated. For all other cases, such as a suspected abscess, atypical presentation, uncertain diagnosis, or a potential complication (e.g., recurrent infection or treatment failure), a biopsy may be warranted.[30]
A biopsy includes fine-needle aspiration biopsy (which can be performed with/without ultrasound guidance) and tissue biopsy (which may be an excisional or incisional biopsy involving a core-needle biopsy, other vacuum-assisted device, or a formal surgical procedure).
Fine-needle aspiration biopsy and/or nipple discharge should be sent for evaluation of a possible malignancy as well as infection.[31] Tissue biopsy permits examination of involved tissue for infection, granulomatous inflammation, and malignancy. Excised tissue should be sent for histopathologic evaluation (cytology) for a possible malignancy and infection (e.g., fungal stains and acid-fast bacilli for TB), especially in refractory and recurrent cases. Skin-punch biopsy can be undertaken to diagnose inflammatory breast carcinoma.[30][Figure caption and citation for the preceding image starts]: Aspirated material: a group of benign apocrine cells associated with acute and chronic inflammation in keeping with a breast abscess (ThinPrep stain)From the collection of Liron Pantanowitz, MD, Tufts University School of Medicine, MA [Citation ends].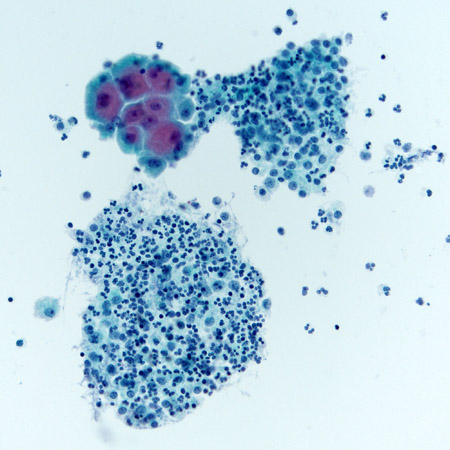
Milk, nipple discharge, aspirated material, or excised tissue can be sent for Gram stain, culture (aerobic and anaerobic) with sensitivity, and fungal and mycobacterial studies.
Culture may be performed in all patients or only in selective cases such as:
Hospital-acquired infection
Severe or unusual cases
Failure to respond to antibiotics within 2 days
Recurrent mastitis.[1]
Expressed milk or a midstream milk sample can be sent for leukocyte counts and microbiology studies, including bacteria quantification.[32] Endogenous breast flora is similar to that present on the skin. Although the presence of pathogenic bacteria and/or high bacterial counts (>10^3/mL of milk) indicates mastitis, the predictive value is low. Therefore, the presence of bacteria in milk does not necessarily indicate infection.[1] Moreover, many lactating women who have potentially pathogenic bacteria on their skin or in their milk will not develop mastitis.[1][33] Alternatively, many women who do develop mastitis may not have pathogenic organisms in their milk.[1] Blood cultures should be obtained in patients who appear toxic.
Mammography
Mammography may be too painful to perform on a breast with an abscess. Also, mammographic findings of breast infection and abscess are nonspecific.[34][35] Breast infection, including TB, can cause the following mammographic findings:
No abnormality
Focal/diffusely increased density
Architectural distortion
A spiculated mass
Skin thickening or retraction
Microcalcification.
The findings may mimic cancer. Therefore, mammography is most useful after the acute phase has resolved. At this stage it can help to identify underlying breast lesions. It should be ordered in women >40 years of age, and whenever the presentation is complicated or atypical, or malignancy is suspected.[36]
Additional investigations
A complete blood count with differential and blood cultures are indicated in patients with suspected systemic infection, abscess, recurrent infection, or treatment failure.
Tests to diagnose possible TB include a tuberculin skin test (purified protein derivative), interferon gamma release assay, microbiology studies, and/or biopsy. See Extrapulmonary tuberculosis (Diagnosis).
When lactational mastitis is suspected, examination of the neonate for candidiasis or skin infection should be considered, specifically with regard to the oral cavity, skin, and diaper area.
Use of this content is subject to our disclaimer