Initial evaluation
Initial assessment includes evaluation of the airway (breathing, pulse oximetry, oral pooling of secretions) and circulation (blood pressure [BP], vascular access).[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
A brief history of stroke symptoms and a streamlined neurologic exam are performed at the same time or immediately following medical stabilization.
Rapid identification and treatment of stroke patients may be provided remotely through the use of telemedicine, which improves access to effective healthcare in community hospitals and rural areas without specialized expertise in stroke.[61]Blacquiere D, Lindsay MP, Foley N, et al. Canadian stroke best practice recommendations: telestroke best practice guidelines update 2017. Int J Stroke. 2017 Oct;12(8):886-95.
https://journals.sagepub.com/doi/10.1177/1747493017706239
http://www.ncbi.nlm.nih.gov/pubmed/28441928?tool=bestpractice.com
[62]Demaerschalk BM, Berg J, Chong BW, et al. American Telemedicine Association: telestroke guidelines. Telemed J E Health. 2017 May;23(5):376-89.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5802246
http://www.ncbi.nlm.nih.gov/pubmed/28384077?tool=bestpractice.com
Stroke scales
The NIH Stroke Scale is a rapid physical assessment tool for stroke signs.
[
NIH Stroke Score
Opens in new window
]
The Intracerebral Hemorrhage (ICH) Score is the most widely used severity-of-illness grading scale for prognosticating outcomes early after onset of intracerebral hemorrhage. Elements of the ICH score include:
ICH volume (>30 cm² = 1 point)
Glasgow Coma Score (GCS) (3-4 = 2 points, 5-12 = 1 point)
Intraventricular hemorrhage (yes = 1 point)
Infratentorial ICH location (yes = 1 point)
Age (>80 years = 1 point).[25]Hemphill JC 3rd, Bonovich DC, Besmertis L, et al. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001 Apr;32(4):891-7.
https://www.ahajournals.org/doi/10.1161/01.STR.32.4.891
http://www.ncbi.nlm.nih.gov/pubmed/11283388?tool=bestpractice.com
Other useful scales are the Glasgow Coma Scale and FUNC score (prediction of functional outcome in patients with primary intracerebral hemorrhage).
Massachusetts General Hospital Stroke Service: FUNC score calculator
Opens in new window
Although these scales are used as formal prognostic instruments, a study has shown that early subjective judgment of physicians correlated more closely with 3-month outcome than did the ICH and FUNC scores.[63]Hwang DY, Dell CA, Sparks MJ, et al. Clinician judgment vs formal scales for predicting intracerebral hemorrhage outcomes. Neurology. 2016 Jan 12;86(2):126-33.
http://www.ncbi.nlm.nih.gov/pubmed/26674335?tool=bestpractice.com
Medical history
The medical history may identify diseases associated with impaired coagulation, including liver disease and hematologic disorders.
A complete medication history is important for identifying patients with anticoagulant-associated hemorrhage.
One meta-analysis of observational studies found that although nonsteroidal anti-inflammatory drugs (NSAIDs) as a single group were not associated with a significantly increased risk of hemorrhagic stroke, a significantly increased risk was observed among users of specific agents (diclofenac and meloxicam).[47]Ungprasert P, Matteson EL, Thongprayoon C. Nonaspirin nonsteroidal anti-inflammatory drugs and risk of hemorrhagic stroke: a systematic review and meta-analysis of observational studies. Stroke. 2016 Feb;47(2):356-64.
http://www.ncbi.nlm.nih.gov/pubmed/26670086?tool=bestpractice.com
Statins have been proven not to increase the risk of hemorrhage, and studies have demonstrated better outcome for patients presenting with intracerebral hemorrhage who were using statins prior to admission.[64]McKinney JS, Kostis WJ. Statin therapy and the risk of intracerebral hemorrhage: a meta-analysis of 31 randomized controlled trials. Stroke. 2012 Aug;43(8):2149-56.
http://www.ncbi.nlm.nih.gov/pubmed/22588266?tool=bestpractice.com
[65]Biffi A, Devan WJ, Anderson CD, et al. Statin use and outcome after intracerebral hemorrhage: case-control study and meta-analysis. Neurology. 2011 May 3;76(18):1581-8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3100126
http://www.ncbi.nlm.nih.gov/pubmed/21451150?tool=bestpractice.com
No relationship has been found between initial intracerebral hemorrhage volume or 24-hour hematoma volume growth and the use of statins at the time of acute intracerebral hemorrhage.[66]Priglinger M, Arima H, Anderson C, et al; INTERACT Investigators. No relationship of lipid-lowering agents to hematoma growth: pooled analysis of the Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trials studies. Stroke. 2015 Mar;46(3):857-9.
https://www.ahajournals.org/doi/full/10.1161/strokeaha.114.007664
http://www.ncbi.nlm.nih.gov/pubmed/25657175?tool=bestpractice.com
[67]Ma Y, Li Z, Chen L, et al. Blood lipid levels, statin therapy and the risk of intracerebral hemorrhage. Lipids Health Dis. 2016 Mar 1;15:43.
https://lipidworld.biomedcentral.com/articles/10.1186/s12944-016-0213-8
http://www.ncbi.nlm.nih.gov/pubmed/26932585?tool=bestpractice.com
Symptoms and signs
In most cases, the symptoms of intracerebral hemorrhage evolve over seconds or minutes. The most common symptoms are:
Presenting signs of intracerebral hemorrhage are variable and depend on the brain regions involved.[68]Passero S, Rocchi R, Rossi S, et al. Seizures after spontaneous supratentorial intracerebral hemorrhage. Epilepsia. 2002 Oct;43(10):1175-80.
http://www.ncbi.nlm.nih.gov/pubmed/12366733?tool=bestpractice.com
Seizure sometimes occurs at the onset of hemorrhage.[68]Passero S, Rocchi R, Rossi S, et al. Seizures after spontaneous supratentorial intracerebral hemorrhage. Epilepsia. 2002 Oct;43(10):1175-80.
http://www.ncbi.nlm.nih.gov/pubmed/12366733?tool=bestpractice.com
Most common findings on neurologic exam are:
Decreased mental status
Partial or total loss of strength in upper and/or lower extremities (usually unilateral)
Fluent or nonfluent language dysfunction
Sensory loss in upper and/or lower extremities (associated with sensory neglect if nondominant hemisphere stroke)
Gaze paresis (often horizontal and unidirectional)
Visual field loss
Dysarthria
Difficulty with fine motor coordination and gait.
There is no sign that reliably distinguishes between intracerebral hemorrhage and ischemic stroke, but intracerebral hemorrhage is more frequently associated with reduced level of consciousness and signs of increased intracranial pressure.[69]Runchey S, McGee S. Does this patient have a hemorrhagic stroke?: clinical findings distinguishing hemorrhagic stroke from ischemic stroke. JAMA. 2010 Jun 9;303(22):2280-6.
http://www.ncbi.nlm.nih.gov/pubmed/20530782?tool=bestpractice.com
Brain stem and cerebellar hemorrhages are more frequently associated with altered level of consciousness, coma, and vomiting than are ischemic strokes.
Subsequent testing
In patients presenting with stroke-like symptoms, urgent neuroimaging with computed tomography (CT) or magnetic resonance imaging (MRI) is recommended to confirm the diagnosis.[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
[70]Cordonnier C, Demchuk A, Ziai W, et al. Intracerebral haemorrhage: current approaches to acute management. Lancet. 2018 Oct 6;392(10154):1257-68.
http://www.ncbi.nlm.nih.gov/pubmed/30319113?tool=bestpractice.com
[71]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-e467.
https://www.doi.org/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Additional testing is recommended to identify etiology: identifying the underlying cause is important, as survivors of primary intracranial hemorrhage are at higher risk of subsequent recurrent intracranial hemorrhage than of subsequent ischemic stroke or myocardial infarction.[72]Bailey RD, Hart RG, Benavente O, et al. Recurrent brain hemorrhage is more frequent than ischemic stroke after intracranial hemorrhage. Neurology. 2001 Mar 27;56(6):773-7.
http://www.ncbi.nlm.nih.gov/pubmed/11274313?tool=bestpractice.com
Computed tomography (CT) of brain
Urgent imaging, typically a noncontrast head CT, is mandatory to discriminate between ischemic and hemorrhagic stroke.[71]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-e467.
https://www.doi.org/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Many neurologic conditions can mimic stroke, so definitive diagnosis is vital. Noncontrast CT may also be used as a follow-up exam to evaluate for expansion and worsening mass effect.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
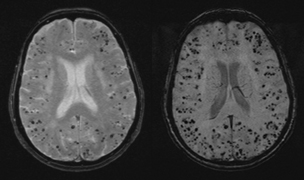
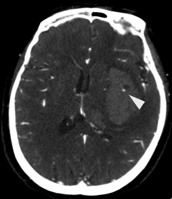
[Figure caption and citation for the preceding image starts]: Intracranial hemorrhage on CT scanMassachusetts General Hospital personal case files; used with permission [Citation ends].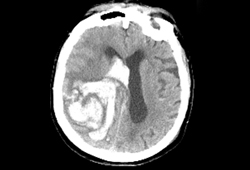
If a hemorrhage is identified, its location and morphology, and presence or absence of associated lesions, such as arteriovenous malformation (AVM), tumor, or signs of infarction, will help identify a possible secondary cause.
Some centers combine CT with CT angiography (CTA), which rapidly excludes the presence of secondary causes such as AVM or aneurysm. CTA has a sensitivity and specificity exceeding 90% compared with catheter arteriography for the identification of these culprit vascular lesions.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
[73]Cheong E, Toner P, Dowie G, et al. Evaluation of a CTA-triage based transient ischemic attack service: a retrospective single center cohort study. J Stroke Cerebrovasc Dis. 2018 Dec;27(12):3436-42.
http://www.ncbi.nlm.nih.gov/pubmed/30193811?tool=bestpractice.com
[74]Delgado Almandoz JE, Schaefer PW, Forero NP, et al. Diagnostic accuracy and yield of multidetector CT angiography in the evaluation of spontaneous intraparenchymal cerebral hemorrhage. AJNR Am J Neuroradiol. 2009 Jun;30(6):1213-21.
https://www.ajnr.org/content/30/6/1213.long
http://www.ncbi.nlm.nih.gov/pubmed/19342546?tool=bestpractice.com
[75]Josephson CB, White PM, Krishan A, et al. Computed tomography angiography or magnetic resonance angiography for detection of intracranial vascular malformations in patients with intracerebral haemorrhage. Cochrane Database Syst Rev. 2014 Sep 1;2014(9):CD009372.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009372.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/25177839?tool=bestpractice.com
[76]Mechtouff L, Boussel L, Cakmak S, et al. Multilevel assessment of atherosclerotic extent using a 40-section multidetector scanner after transient ischemic attack or ischemic stroke. AJNR Am J Neuroradiol. 2014 Mar;35(3):568-72.
https://www.ajnr.org/content/35/3/568.long
http://www.ncbi.nlm.nih.gov/pubmed/24136645?tool=bestpractice.com
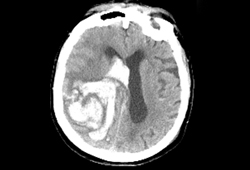
In addition, the presence of hyperdense contrast material in the hematoma bed on postinjection CT images (spot sign) is associated with greater risk of subsequent hematoma expansion.[77]Wada R, Aviv RI, Fox AJ, et al. CT angiography "spot sign" predicts hematoma expansion in acute intracerebral hemorrhage. Stroke. 2007 Apr;38(4):1257-62.
https://www.ahajournals.org/doi/full/10.1161/01.str.0000259633.59404.f3
http://www.ncbi.nlm.nih.gov/pubmed/17322083?tool=bestpractice.com
[78]Goldstein JN, Fazen LE, Snider R, et al. Contrast extravasation on CT angiography predicts hematoma expansion in intracerebral hemorrhage. Neurology. 2007 Mar 20;68(12):889-94.
http://www.ncbi.nlm.nih.gov/pubmed/17372123?tool=bestpractice.com
A spot sign score predicts hematoma expansion and poor clinical outcomes.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
[79]Delgado Almandoz JE, Yoo AJ, Stone MJ, et al. Systematic characterization of the computed tomography angiography spot sign in primary intracerebral hemorrhage identifies patients at highest risk for hematoma expansion: the spot sign score. Stroke. 2009 Sep;40(9):2994-3000.
https://www.ahajournals.org/doi/full/10.1161/strokeaha.109.554667
http://www.ncbi.nlm.nih.gov/pubmed/19574553?tool=bestpractice.com
[80]Almandoz JE, Yoo AJ, Stone MJ, et al. The spot sign score in primary intracerebral hemorrhage identifies patients at highest risk of in-hospital mortality and poor outcome among survivors. Stroke. 2010 Jan;41(1):54-60.
http://www.ncbi.nlm.nih.gov/pubmed/19910545?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Spot sign on CT angiogram (arrowhead), indicating the presence of hyperdense contrast material within the hematoma bed on postinjection CT; this has been associated with greater risk of subsequent hematoma expansionFoothills Medical Center personal case files; used with permission [Citation ends].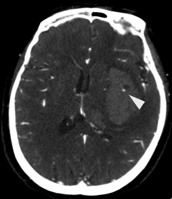
At least one more brain imaging study should be performed after the initial diagnostic CT to assess for expansion and determine the final hematoma size.[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
[81]Naidech AM. Diagnosis and management of spontaneous intracerebral hemorrhage. Continuum (Minneap Minn). 2015 Oct;21(5 Neurocritical Care):1288-98.
http://www.ncbi.nlm.nih.gov/pubmed/26426231?tool=bestpractice.com
Blood tests and ECG
Simultaneously, basic blood tests (complete blood count [CBC], electrolytes, blood urea nitrogen [BUN], creatinine, and partial thromboplastin and prothrombin times) and ECG (to rule out cardiac ischemia or arrhythmia) are recommended to exclude hypocoagulability and other comorbid conditions.[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
Vascular imaging
Acute CTA plus consideration of CT venography (CTV) is recommended to exclude macrovascular causes of cerebral venous thrombosis in the following groups:[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
Lobar spontaneous intracerebral hemorrhage and age <70 years, or
Deep/posterior fossa spontaneous intracerebral hemorrhage and age <45 years, or
Deep/posterior fossa and age 45 to 70 years without history of hypertension.
Based on clinical experience in practice, acute magnetic resonance angiogram (MRA) plus venography may be considered in the same patient groups if CTA or CTV cannot be obtained (due to inaccessibility or contrast allergy) or if there is concern about renal impairment. MRA may also be useful to exclude underlying vascular malformations if the etiology is uncertain.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
However, acute MRA plus venography has lower spatial resolution than CTA/CTV.
If there is a high index of suspicion for AVM, but noninvasive imaging is not diagnostic, conventional invasive angiography is recommended.[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
Conventional invasive angiography can demonstrate small AVMs that would otherwise be missed by noninvasive techniques, but its routine use has been supplanted in many centers by safer, noninvasive vessel imaging methods.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
In patients with spontaneous intraventricular hemorrhage and no detectable parenchymal hemorrhage, catheter intra-arterial digital subtraction angiography (DSA) is recommended to exclude a macrovascular cause.[9]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
In the acute period, catheter arteriography may miss vascular malformations that are detected by repeat arteriography several weeks later.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
[82]Hino A, Fujimoto M, Yamaki T, et al. Value of repeat angiography in patients with spontaneous subcortical hemorrhage. Stroke. 1998 Dec;29(12):2517-21.
https://www.ahajournals.org/doi/10.1161/01.str.29.12.2517
http://www.ncbi.nlm.nih.gov/pubmed/9836762?tool=bestpractice.com
Magnetic resonance imaging (MRI)
Recommended when certain disease processes are part of the differential diagnosis (e.g., vascular malformation, tumor, cerebral infarction, or cerebral sinus/venous thrombosis) that may not be readily apparent on CT.[2]Smith EE, Rosand J, Greenberg SM. Hemorrhagic stroke. Neuroimaging Clin N Am. 2005 May;15(2):259-72.
http://www.ncbi.nlm.nih.gov/pubmed/16198939?tool=bestpractice.com
[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
[83]Wijman CA, Venkatasubramanian C, Bruins S, et al. Utility of early MRI in the diagnosis and management of acute spontaneous intracerebral hemorrhage. Cerebrovasc Dis. 2010;30(5):456-63.
https://karger.com/ced/article/30/5/456/69445/Utility-of-Early-MRI-in-the-Diagnosis-and
http://www.ncbi.nlm.nih.gov/pubmed/20733299?tool=bestpractice.com
[84]Dylewski DA, Demchuk AM, Morgenstern LB. Utility of magnetic resonance imaging in acute intracerebral hemorrhage. J Neuroimaging. 2000 Apr;10(2):78-83.
http://www.ncbi.nlm.nih.gov/pubmed/10800260?tool=bestpractice.com
MRI is useful for evaluating alternative etiologies in patients ages <55 years who do not have typical hypertensive hemorrhage.[13]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
[83]Wijman CA, Venkatasubramanian C, Bruins S, et al. Utility of early MRI in the diagnosis and management of acute spontaneous intracerebral hemorrhage. Cerebrovasc Dis. 2010;30(5):456-63.
https://karger.com/ced/article/30/5/456/69445/Utility-of-Early-MRI-in-the-Diagnosis-and
http://www.ncbi.nlm.nih.gov/pubmed/20733299?tool=bestpractice.com
[85]Kamel H, Navi BB, Hemphill JC 3rd. A rule to identify patients who require magnetic resonance imaging after intracerebral hemorrhage. Neurocrit Care. 2013 Feb;18(1):59-63.
http://www.ncbi.nlm.nih.gov/pubmed/21761271?tool=bestpractice.com
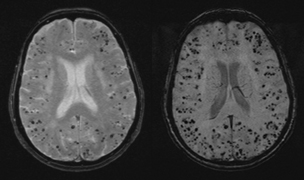
A gradient-echo sequence, which is sensitive to susceptibility effects of iron from hemorrhage, is performed to identify whether microbleeds are present. The presence of multiple microbleeds restricted to lobar brain locations suggests a diagnosis of cerebral amyloid angiopathy in the absence of other causes.[15]Smith EE, Greenberg SM. Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Curr Atheroscler Rep. 2003 Jul;5(4):260-6.
http://www.ncbi.nlm.nih.gov/pubmed/12793966?tool=bestpractice.com
Cerebral amyloid angiopathy has a worse prognosis for recurrent hemorrhage than other cases of primary intracerebral hemorrhage, and thus it is important to identify.[86]Viswanathan A, Rakich SM, Engel C, et al. Antiplatelet use after intracerebral hemorrhage. Neurology. 2006 Jan 24;66(2):206-9.
http://www.ncbi.nlm.nih.gov/pubmed/16434655?tool=bestpractice.com
Susceptibility-weighted imaging (SWI) may be more sensitive for identification of microbleeds and small cerebral cavernous malformations than MRI gradient-echo sequence.[87]Mittal S, Wu Z, Neelavalli J, et al. Susceptibility-weighted imaging: technical aspects and clinical applications, part 2. AJNR Am J Neuroradiol. 2009 Feb;30(2):232-52.
http://www.ajnr.org/content/30/2/232.long
http://www.ncbi.nlm.nih.gov/pubmed/19131406?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: 80-year-old woman with numerous punctate foci of hypointensity (black dots) on MRI gradient-echo (GRE) sequence (left), suggesting multiple lobar microbleeds caused by cerebral amyloid angiopathy. MRI susceptibility-weighted imaging (SWI) sequence (right) demonstrates numerous additional microbleeds not seen on the GRE sequenceFoothills Medical Center personal case files; used with permission [Citation ends].