History
Patients may report occurrences of skin lesions often accompanied by psychosocial stress (anxiety). Cutaneous lesions are usually painless and nonpruritic and so may also be asymptomatic.[4]Cesarman E, Damania B, Krown SE, et al. Kaposi sarcoma. Nat Rev Dis Primers. 2019 Jan 31;5(1):9.
https://www.nature.com/articles/s41572-019-0060-9
http://www.ncbi.nlm.nih.gov/pubmed/30705286?tool=bestpractice.com
Tumors on the lower leg may affect gait. Lymphedema of the legs, genitalia, and face may be disfiguring and sometimes painful. Oral lesions can bleed and ulcerate, and may affect mastication, speech, and swallowing.
KS of the gastrointestinal (GI) tract can cause weight loss, abdominal pain, nausea and vomiting, ileus, upper or lower GI tract bleeding, malabsorption, intestinal obstruction, and, infrequently, diarrhea.[4]Cesarman E, Damania B, Krown SE, et al. Kaposi sarcoma. Nat Rev Dis Primers. 2019 Jan 31;5(1):9.
https://www.nature.com/articles/s41572-019-0060-9
http://www.ncbi.nlm.nih.gov/pubmed/30705286?tool=bestpractice.com
Pulmonary KS can present with dyspnea, fever, cough, hemoptysis, or chest pain.[4]Cesarman E, Damania B, Krown SE, et al. Kaposi sarcoma. Nat Rev Dis Primers. 2019 Jan 31;5(1):9.
https://www.nature.com/articles/s41572-019-0060-9
http://www.ncbi.nlm.nih.gov/pubmed/30705286?tool=bestpractice.com
KS may also be an incidental finding in people presenting with, or being followed for, an underlying condition such as HIV infection or organ transplantation.
Existing human herpesvirus-8 (HHV-8) infection is necessary for the development of KS. Individuals with other HHV-8-related diseases, such as multicentric Castleman disease and primary effusion lymphoma (PEL), are also at risk for developing concomitant KS.[26]Sullivan RJ, Pantanowitz L, Casper C, et al. HIV/AIDS: epidemiology, pathophysiology, and treatment of Kaposi sarcoma-associated herpesvirus disease: Kaposi sarcoma, primary effusion lymphoma, and multicentric Castleman disease. Clin Infect Dis. 2008 Nov 1;47(9):1209-15.
https://academic.oup.com/cid/article/47/9/1209/461483
http://www.ncbi.nlm.nih.gov/pubmed/18808357?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Multiple pink-purple Kaposi sarcoma nodules on the lower extremityFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
Examination
Initial evaluation of a patient with KS includes a complete physical examination with special attention to areas frequently affected by lesions, such as the lower extremities, face, oral mucosa, and genitalia.[4]Cesarman E, Damania B, Krown SE, et al. Kaposi sarcoma. Nat Rev Dis Primers. 2019 Jan 31;5(1):9.
https://www.nature.com/articles/s41572-019-0060-9
http://www.ncbi.nlm.nih.gov/pubmed/30705286?tool=bestpractice.com
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
Lymph nodes should be examined.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
Mucocutaneous lesions and lymphedema may be extensive and should be documented.
Skin lesions of KS typically have the following characteristics:[3]Lebbe C, Garbe C, Stratigos AJ, et al; European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO), and the European Organisation for Research and Treatment of Cancer (EORTC). Diagnosis and treatment of Kaposi's sarcoma: European consensus-based interdisciplinary guideline (EDF/EADO/EORTC). Eur J Cancer. 2019 Jun;114:117-27.
http://www.ncbi.nlm.nih.gov/pubmed/31096150?tool=bestpractice.com
Multifocal
Asymmetrically distributed
Varied size
Varied color (pink, red, purple, brown, or blue)
Nodular
Papular
Plaque-like
Bullous-like
Indurated (woody)
Verrucous
Fungating
Ulcerated
Infected.
[Figure caption and citation for the preceding image starts]: Multiple pink-purple Kaposi sarcoma nodules on the lower extremityFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Kaposi sarcoma cutaneous purple-brown plaque on the footFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Kaposi sarcoma cutaneous purple-brown plaque on the footFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
Visceral involvement, with and without mucocutaneous lesions, should be determined with attention specifically directed to the lymph nodes, GI tract, and respiratory system.
Investigations
If HIV status is unknown, an HIV test should be performed in individuals presenting with KS.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[3]Lebbe C, Garbe C, Stratigos AJ, et al; European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO), and the European Organisation for Research and Treatment of Cancer (EORTC). Diagnosis and treatment of Kaposi's sarcoma: European consensus-based interdisciplinary guideline (EDF/EADO/EORTC). Eur J Cancer. 2019 Jun;114:117-27.
http://www.ncbi.nlm.nih.gov/pubmed/31096150?tool=bestpractice.com
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
If the patient is HIV-positive, a CD4+ T-cell count and HIV viral load should be obtained.
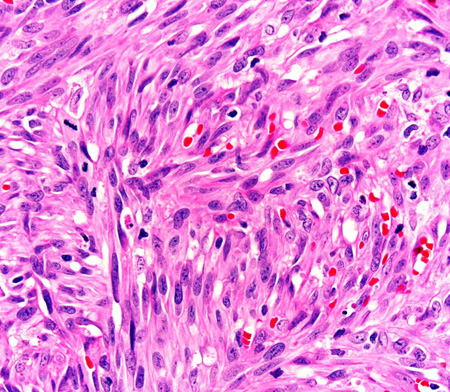
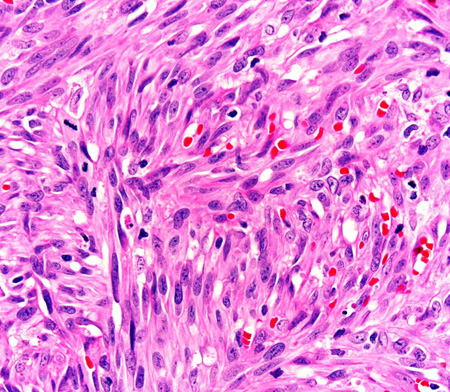
Clinically suspected skin lesions should be confirmed by a small punch biopsy of 2-4 mm with histopathology. Skin punch biopsies are easy to perform and readily help exclude mimics. Histopathology shows characteristic atypical spindle-shaped cells.[36]Radu O, Pantanowitz L. Kaposi sarcoma. Arch Pathol Lab Med. 2013 Feb;137(2):289-94.
https://meridian.allenpress.com/aplm/article/137/2/289/65260/Kaposi-Sarcoma
http://www.ncbi.nlm.nih.gov/pubmed/23368874?tool=bestpractice.com
Immunohistochemistry techniques can be used to detect the following markers expressed by Kaposi sarcoma lesional cells: latency-associated nuclear antigen-1 (LANA-1, a surrogate marker for HHV-8); CD31/CD34 (vascular endothelial cell immunomarkers), and D2-40 (a lymphatic cell immunomarker).[37]Jary A, Veyri M, Gothland A, et al. Kaposi's sarcoma-associated herpesvirus, the etiological agent of all epidemiological forms of Kaposi's sarcoma. Cancers (Basel). 2021 Dec 9;13(24):6208.
https://www.doi.org/10.3390/cancers13246208
http://www.ncbi.nlm.nih.gov/pubmed/34944828?tool=bestpractice.com
[38]Rosado FG, Itani DM, Coffin CM, et al. Utility of immunohistochemical staining with FLI1, D2-40, CD31, and CD34 in the diagnosis of acquired immunodeficiency syndrome-related and non-acquired immunodeficiency syndrome-related Kaposi sarcoma. Arch Pathol Lab Med. 2012 Mar;136(3):301-4.
https://meridian.allenpress.com/aplm/article/136/3/301/185684/Utility-of-Immunohistochemical-Staining-With-FLI1
http://www.ncbi.nlm.nih.gov/pubmed/22372906?tool=bestpractice.com
A positive LANA-1 stain can establish KS diagnosis; CD31 and CD34 may be useful if it is unclear whether the tumor is vascular in origin.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
[38]Rosado FG, Itani DM, Coffin CM, et al. Utility of immunohistochemical staining with FLI1, D2-40, CD31, and CD34 in the diagnosis of acquired immunodeficiency syndrome-related and non-acquired immunodeficiency syndrome-related Kaposi sarcoma. Arch Pathol Lab Med. 2012 Mar;136(3):301-4.
https://meridian.allenpress.com/aplm/article/136/3/301/185684/Utility-of-Immunohistochemical-Staining-With-FLI1
http://www.ncbi.nlm.nih.gov/pubmed/22372906?tool=bestpractice.com
Determination of HHV-8 (polymerase chain reaction [PCR]) and assays for HHV-8 antibodies are not typically warranted in routine clinical practice, but may be available on an individual basis.[3]Lebbe C, Garbe C, Stratigos AJ, et al; European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO), and the European Organisation for Research and Treatment of Cancer (EORTC). Diagnosis and treatment of Kaposi's sarcoma: European consensus-based interdisciplinary guideline (EDF/EADO/EORTC). Eur J Cancer. 2019 Jun;114:117-27.
http://www.ncbi.nlm.nih.gov/pubmed/31096150?tool=bestpractice.com
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
Bone marrow function, and hepatic and renal function, will need to be evaluated in patients requiring systemic chemotherapy. Obtaining a CBC and comprehensive metabolic panel forms part of the initial work up.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
Imaging studies and subsequent investigations
Lung imaging with chest x-ray is useful to screen for pulmonary KS in patients with advanced disease or respiratory symptoms.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
Concomitant pulmonary infection must be excluded. Chest computed tomography (CT) and bronchoscopy can be used to establish a diagnosis of pulmonary KS in patients with an abnormal chest x-ray.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
Biopsy of respiratory tract lesions is relatively contraindicated because of the risk of bleeding.[39]Pitchenik AE, Fischl MA, Saldana MJ. Kaposi's sarcoma of the tracheobronchial tree. Clinical, bronchoscopic, and pathologic features. Chest. 1985 Jan;87(1):122-4.
http://www.ncbi.nlm.nih.gov/pubmed/3965256?tool=bestpractice.com
[40]Zibrak JD, Silvestri RC, Costello P, et al. Bronchoscopic and radiologic features of Kaposi's sarcoma involving the respiratory system. Chest. 1986 Oct;90(4):476-9.
http://www.ncbi.nlm.nih.gov/pubmed/3489584?tool=bestpractice.com
[41]Kodra A, Walczyszyn M, Grossman C, et al. Case report: pulmonary Kaposi sarcoma in a non-HIV patient. F1000Res. 2015 Oct 7;4:1013.
https://f1000research.com/articles/4-1013/v1
http://www.ncbi.nlm.nih.gov/pubmed/26664711?tool=bestpractice.com
Lymphadenopathy should be examined histologically if a coexisting disorder (e.g., infection, lymphoma, multicentric Castleman disease) is suspected.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[42]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Castleman disease [internet publication].
https://www.nccn.org/guidelines/category_1
Fecal occult blood is useful to screen for GI tract disease if visceral involvement is suspected.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
GI endoscopy and CT of the abdomen/pelvis in symptomatic individuals are not recommended as part of routine evaluation in the absence of iron deficiency, GI blood loss, or GI symptoms.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Kaposi sarcoma [internet publication].
https://www.nccn.org/guidelines/category_1
[4]Cesarman E, Damania B, Krown SE, et al. Kaposi sarcoma. Nat Rev Dis Primers. 2019 Jan 31;5(1):9.
https://www.nature.com/articles/s41572-019-0060-9
http://www.ncbi.nlm.nih.gov/pubmed/30705286?tool=bestpractice.com
CT scan, positron emission tomography (PET) scan, and magnetic resonance imaging (MRI) may be helpful for evaluating deep nodal and visceral KS, and bone lesions. Bone lesions are best detected by CT scan and MRI, as they frequently go undetected on plain x-ray or bone scans.[43]Caponetti G, Dezube BJ, Restrepo C, et al. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer. 2007 Mar 15;109(6):1040-52.
https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.22500
http://www.ncbi.nlm.nih.gov/pubmed/17265518?tool=bestpractice.com
If chemotherapy or radiation therapy is planned, pregnancy testing should be performed in patients of childbearing potential.[5]Esser S, Schöfer H, Hoffmann C, et al. S1 guidelines for the Kaposi sarcoma. J Dtsch Dermatol Ges. 2022 Jun;20(6):892-904.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14788
http://www.ncbi.nlm.nih.gov/pubmed/35657085?tool=bestpractice.com
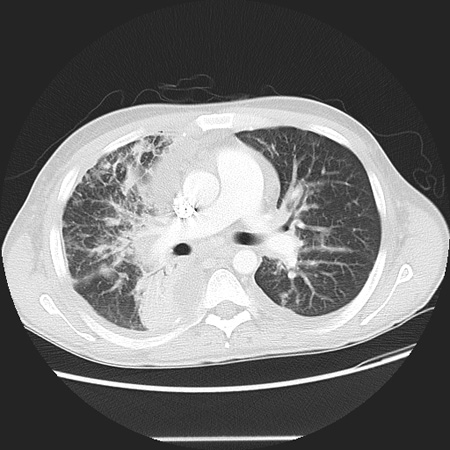
[Figure caption and citation for the preceding image starts]: Photomicrograph of the histopathology of Kaposi sarcoma showing fascicles of vasoformative spindle-shaped tumor cells (hematoxylin and eosin stain)From the collection of Dr Liron Pantanowitz; used with permission [Citation ends].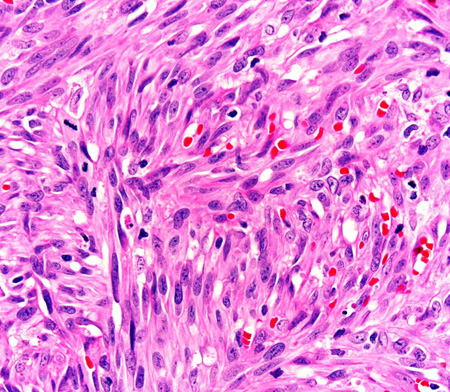 [Figure caption and citation for the preceding image starts]: CT scan of the chest showing a reticular pattern due to pulmonary involvement by Kaposi sarcomaFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of the chest showing a reticular pattern due to pulmonary involvement by Kaposi sarcomaFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].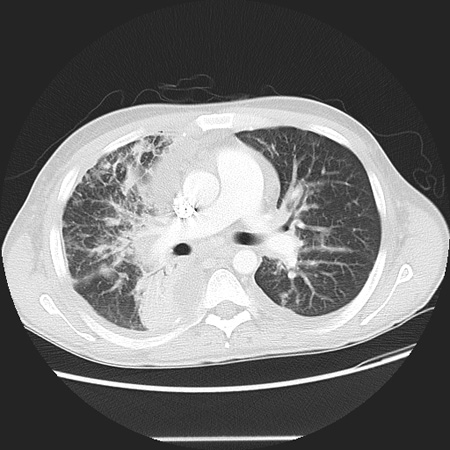

 [Figure caption and citation for the preceding image starts]: Kaposi sarcoma cutaneous purple-brown plaque on the footFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Kaposi sarcoma cutaneous purple-brown plaque on the footFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: CT scan of the chest showing a reticular pattern due to pulmonary involvement by Kaposi sarcomaFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of the chest showing a reticular pattern due to pulmonary involvement by Kaposi sarcomaFrom the collection of Dr Bruce J. Dezube; used with permission [Citation ends].