Approach
Patients may present with features of the underlying cause of the haemolytic anaemia and/or with signs of anaemia such as fatigue, shortness of breath, and dizziness.[37] Association of symptoms with exposure to cold may suggest presence of cold agglutinins.
History
Full history should be taken, including a complete drug history to ascertain whether there is a drug-induced aetiology. Ascertaining the time of onset may narrow the differential diagnosis. For example, an acute onset would indicate an acquired cause, whereas chronicity points more towards an inherited cause.
Physical examination
Examination may show signs of anaemia, jaundice, or splenomegaly, but there are no signs specific to the condition.
Physical findings of the underlying causes are diverse and include generalised lymphadenopathy in cases of lymphoproliferative disease (chronic lymphocytic leukaemia and non-Hodgkin's lymphoma); specific cutaneous and joint signs in autoimmune disease (systemic lupus erythematosus [SLE], rheumatoid arthritis); fever in infectious causes; elevated blood pressure in a pregnant patient with pre-eclampsia or HELLP syndrome (haemolysis, elevated liver enzymes, low platelet count); and skeletal deformities in sickle cell anaemia or thalassaemia, due to increases in haematopoiesis and bone expansion during childhood.
Laboratory tests to determine the presence of haemolysis
The initial tests to perform are a full blood count and comprehensive metabolic panel. Anaemia with an increased mean corpuscular haemoglobin concentration is usually present in haemolysis (due to the increased corpuscular volume of reticulocytes). Red blood cell (RBC) destruction and release of haemoglobin results in an elevated lactate dehydrogenase and unconjugated bilirubin. Urinalysis will show haemoglobinuria in cases of intravascular haemolysis. Haptoglobin should be requested and will be low if haemolysis is present.
A peripheral blood smear is then required to confirm the presence of reticulocytes and will also provide differentiating information as to the cause of haemolysis. The presence of schistocytes suggests a microangiopathic process (disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, haemolytic uraemic syndrome, HELLP syndrome) or traumatic process (prosthetic heart valve, footstrike [march] haemolysis) as a cause. Spherocytes and elliptocytes may indicate hereditary spherocytosis and elliptocytosis. Blister or bite cells indicate the presence of oxidative damage to the cell. Spur cells are present in liver disease. RBC inclusions may be seen in infections such as malaria, babesiosis, and Bartonella infections. [Figure caption and citation for the preceding image starts]: Photomicrograph revealing the presence of what were determined to be numbers of intraerythrocytic Babesia sp. ring-form parasitesCDC/ Dr Mae Melvin [Citation ends].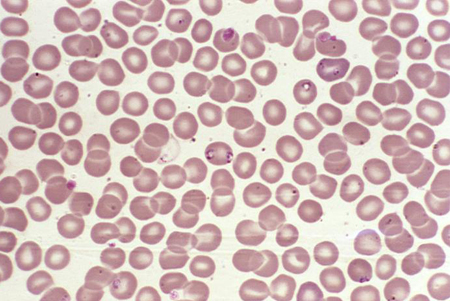 [Figure caption and citation for the preceding image starts]: A photomicrograph of a blood smear showing erythrocytes containing developing Plasmodium vivax parasitesCDC/ Dr Mae Melvin [Citation ends].
[Figure caption and citation for the preceding image starts]: A photomicrograph of a blood smear showing erythrocytes containing developing Plasmodium vivax parasitesCDC/ Dr Mae Melvin [Citation ends].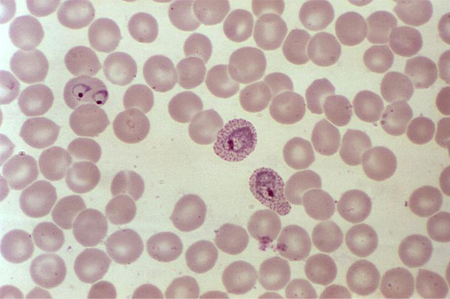
Subsequent testing for specific cause
Should be directed by the suspected diagnosis from clinical evaluation:
A positive direct antiglobulin test (Coombs') indicates the presence of immune causes of haemolytic anemia. The basic direct antiglobulin test typically detects autoantibodies to IgG and complement (C3d).[37][38]
Paroxysmal cold haemoglobinuria is diagnosed in patients with haemolysis (with direct antiglobulin test usually positive for C3 only) and a positive Donath-Landsteiner test.[37][38][39] False-negative results can be avoided by using an indirect method.[37]
Antinuclear antibody should be requested to evaluate for SLE.
Hb electrophoresis detects haemoglobinopathy.
Testing for glucose-6-phosphate dehydrogenase deficiency includes a fluorescent spot test followed by definitive assay of glucose-6-phosphate dehydrogenase activity by spectrophotometry.
Paroxysmal nocturnal haemoglobinuria is evaluated by flow cytometry for CD55/CD59.
Abnormal renal function in the presence of haemolysis suggests haemolytic uraemic syndrome or thrombotic thrombocytopenic purpura.
Elevated liver function tests may indicate liver disease.
Venepuncture and phlebotomy animated demonstrationHow to take a venous blood sample from the antecubital fossa using a vacuum needle.
Use of this content is subject to our disclaimer
