Aetiology
There are many causes of haemolysis.
Hereditary causes fall into three broad categories:[1][2]
Inherited red blood cell (RBC) defects (membrane defects) - hereditary spherocytosis, elliptocytosis, pyropoikilocytosis
Enzyme deficiencies - glucose-6-phosphate dehydrogenase deficiency, pyruvate kinase deficiency
Abnormal Hb production - sickle cell anaemia, thalassaemia.
Acquired haemolytic anaemia can be subdivided into immune and non-immune aetiologies:
Autoantibodies - the cause of immune-mediated haemolytic anaemias, most often as part of other autoimmune conditions (e.g., systemic lupus erythematosus, rheumatoid arthritis, scleroderma) or related to a lymphoproliferative disorder (non-Hodgkin's lymphoma, chronic lymphocytic leukaemia).
Immune haemolytic anaemias - divided into warm- or cold-reacting antibodies, depending on the temperature at which the antibody binds most avidly to the RBCs.
Alloimmune haemolytic anaemias - include haemolytic disease of the newborn or transfusion reaction.
Drugs - some through immune-mediated mechanisms and others through non-immune-mediated mechanisms.
Other non-immune-mediated causes - include infection, trauma in various forms (microangiopathic haemolysis such as disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, haemolytic uraemic syndrome, malignant hypertension, eclampsia, HELLP syndrome [haemolysis, elevated liver enzymes, low platelet count] in pregnancy, mechanical prosthetic heart valves, march haemolysis, thermal injury, osmotic lysis), hypersplenism, and liver disease.
Paroxysmal nocturnal haemoglobinuria - a rare disorder resulting in an acquired RBC membrane defect and subsequent haemolysis.
Pathophysiology
Haemolytic anaemia results from either intravascular or extravascular red blood cell (RBC) destruction.
Extravascular haemolysis results from accelerated red cell destruction by cells of the reticuloendothelial system, due to immune targeting by antibodies, as occurs in a warm autoimmune haemolytic anaemia. Intravascular haemolysis results from red cell destruction within the vasculature, due to complement-mediated lysis or direct red cell trauma from a prosthetic heart valve or microangiopathic process.
Autoimmune haemolysis is most often due to extravascular destruction of red cells coated with an autoantibody (positive direct antiglobulin test [Coombs' positive]). Because sections of the RBC membrane are removed by the reticuloendothelial cells, RBCs with a smaller surface area appear as spherocytes on the peripheral smear. In contrast, traumatic disruption of red cells by microangiopathic processes results in the production of red cell fragments, or schistocytes, on the smear. This also results in the release of RBC lactate dehydrogenase and haemoglobin (Hb) into the circulation, which can result in haemoglobinuria. Free Hb is bound by haptoglobin, resulting in the decrease in haptoglobin that is observed in many cases of haemolytic anaemia.
Hereditary causes of haemolytic anaemia, including membrane defects, enzyme mutations, and haemoglobinopathies, generally result in anaemia due to significantly shortened RBC lifespan and removal of senescent red cells by the spleen. [Figure caption and citation for the preceding image starts]: Peripheral blood smear with spherocytes, reticulocytes, and a nucleated red blood cellFrom the collection of John Densmore, Department of Medicine, University of Virginia [Citation ends].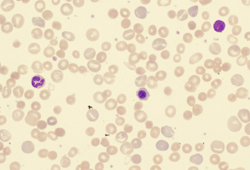 [Figure caption and citation for the preceding image starts]: Peripheral blood smear with red blood cell fragments, or schistocytes (arrow)From the collection of John Densmore, Department of Medicine, University of Virginia [Citation ends].
[Figure caption and citation for the preceding image starts]: Peripheral blood smear with red blood cell fragments, or schistocytes (arrow)From the collection of John Densmore, Department of Medicine, University of Virginia [Citation ends].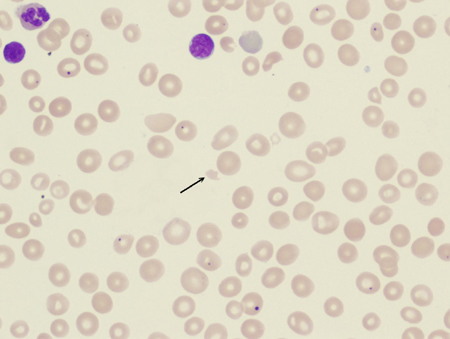
Classification
Acquired haemolytic anaemia: immune or non-immune
Immune (direct antiglobulin test often positive):
Warm antibody autoimmune haemolytic anaemia: antibody (usually IgG) binds most avidly at core body temperature. Associated with underlying diseases such as systemic lupus erythematosus, lymphoma, and chronic lymphocytic leukaemia.
Cold antibody autoimmune haemolytic anaemia: antibody binds red blood cell at temperature below body temperature (often IgM, but may be IgG). Can be idiopathic, or associated with infection or malignancy.
Drug-induced immune haemolytic anaemia.
Alloimmune haemolytic anaemia: haemolytic disease of the newborn or transfusion reaction.
Non-immune (direct antiglobulin test negative):
Infection: malaria, babesiosis, bartonellosis.
Bacterial toxins: Clostridium perfringens infection.
Drug-induced (by non-immune mechanism).
Trauma: microangiopathic haemolysis such as disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, haemolytic uraemic syndrome, eclampsia, HELLP syndrome (haemolysis, elevated liver enzymes, low platelet count) in pregnancy; mechanical prosthetic heart valve; march haemolysis.
Membrane disorder (acquired): paroxysmal nocturnal haemoglobinuria, liver disease.
Thermal injury.
Osmotic lysis.
Hypersplenism.
Congenital haemolytic anaemia[1][2]
Red cell membrane disorders:
Hereditary spherocytosis
Elliptocytosis
Pyropoikilocytosis
Red cell enzyme defects:
Glucose-6-phosphate dehydrogenase deficiency
Pyruvate kinase deficiency
Haemoglobinopathies:
Sickle cell anaemia
Thalassaemia
Use of this content is subject to our disclaimer