Approach
The goals of treatment are:
1) relief of mass effect when present,
2) identification of a pathological agent by specimen culture,
3) control and eradication of infection,
4) minimisation of loss of neurological function, and
5) systemic supportive care.
Prompt diagnosis and institution of early treatment aids in the accomplishment of all of these goals. The treatment outlined below is applicable to adults. Specialty care is part of the treatment of all patients with brain abscess. However, treatment of children and neonates is beyond the scope of this topic, and sub-specialists should be consulted.
Presumptive treatment in all patients
Antibiotics
Antibiotics are the first-line treatment and should be started immediately unless the patient is to be taken to the operating room, in which case antibiotics are held until aspiration of the lesion contents yields a sample for culture.[4]
Considerations in choosing antibiotics are permeability of the drug across the blood-brain barrier and the barrier's function within the acidic environment of the abscess cavity.
A presumptive regimen in adults commonly includes vancomycin, plus metronidazole or clindamycin, plus a third-generation cephalosporin.[42]
Others have proposed a regimen of empiric antibiotics based upon the location of the abscess in the brain.[43] For example, anaerobes are frequently found on culture of temporal lobe abscesses.
Once the aetiological agent is identified, treatment is tailored to the sensitivity of the specific agent.
Anticonvulsants
Prophylaxis with anticonvulsants should be considered for patients who have had a seizure or those with an abscess near the motor cortex or the brain surface. Routine anticonvulsant prophylaxis is not recommended.[5] There are no studies of anticonvulsant prophylaxis in patients with brain abscess, and anticonvulsant prophylaxis does not reduce the risk of seizures in patients with brain tumours.[44]
Levetiracetam is typically used when anticonvulsant prophylaxis is indicated. It is generally well tolerated and is associated with fewer drug-drug interactions than other anticonvulsants.
Corticosteroids
Cause rapid reduction in vasogenic oedema associated with cerebral abscesses, and may be used in the acutely decompensating patient as a life-saving measure.
However, corticosteroid use is generally avoided in stable patients because of the belief that it may decrease the immune response and partially restore the blood-brain barrier, thereby decreasing the penetration of antimicrobials into the central nervous system.
This is somewhat controversial as some experimental models suggest that inflammatory response may not be adversely affected by administration of corticosteroids.[45] Others have shown a decrease in inflammatory response with increased bacterial survival.[46]
Dexamethasone is generally used when corticosteroid treatment is warranted.
Treatment of suspected or confirmed bacterial brain abscess
Once the aetiological agent is identified, treatment is tailored to the sensitivity of the specific strain if possible. Non-surgical management alone is not recommended for lesions >2.5 cm to 3 cm in diameter.[47] When multiple lesions are present, it is reasonable to aspirate lesions >2.5 cm in diameter and to treat the remaining lesions non-surgically. Several published reports demonstrated successful treatment supporting this strategy.[48] The duration of treatment is variable, but generally patients are treated for 6 to 8 weeks, with serial neuro-imaging performed to ensure a beneficial treatment response. The patient is followed up for at least 1 year with imaging to ensure that there is no abscess recurrence. In the case of presumed bacterial abscess and negative cultures, empirical antibiotics are continued.
[Figure caption and citation for the preceding image starts]: Treatment algorithm for brain abscessFrom the collection of Walter Hall, SUNY Upstate Medical University [Citation ends].
Treatment of suspected or confirmed fungal brain abscess
Patients are treated with antibiotics until fungal disease is suspected or confirmed. Antifungal agents in general have particularly poor penetration across the blood-brain barrier, and medical therapy alone is rarely indicated for fungal brain abscesses. As with bacterial brain abscesses, selection of the appropriate agent is the first line of treatment. Antifungal agents are selected based upon the offending agent.
Candida albicans infection is treated with amphotericin B, fluconazole, or caspofungin.
Cryptococcal infections require amphotericin B and flucytosine, although fluconazole can be used as an alternative. Flucytosine is contraindicated in patients with known complete dihydropyrimidine dehydrogenase (DPD) deficiency due to the risk of life-threatening drug toxicity. Patients with a partial DPD deficiency are also at increased risk of severe toxicity. Although pretesting of DPD status is not required, consider determination of DPD activity if drug toxicity is confirmed or suspected.
Liposomal amphotericin B has increased permeability across the blood-brain barrier and has been used to treat Aspergillus non-surgically, although A fumigatus and Mucormycosis species abscesses are still best treated with surgery followed by antifungal therapy.
Treatment of suspected or confirmed parasitic brain abscess
Patients are treated with antibiotics until parasitic disease is suspected or confirmed. As with bacterial brain abscesses, selection of the appropriate antimicrobial agent is the first line of treatment. Antiparasitic agents are selected based upon the pathological agent. Toxoplasma gondii abscess is treated with pyrimethamine and sulfadiazine. An alternative treatment is trimethoprim-sulfamethoxazole, which has been shown to be equivalent therapeutically to pyrimethamine and sulfadiazine.[49] If toxoplasmosis is the presentation of newly diagnosed HIV, or if the patient has untreated HIV infection, rapid commencement of antiretroviral therapy (ART) is mandatory and may lead to resolution of the toxoplasma infection. Taenia solium is treated with praziquantel. Naegleria fowleri infection is treated with amphotericin B, although this infection is almost invariably fatal. [Figure caption and citation for the preceding image starts]: Brain MRI before treatment (left image) and 18 months after antiretroviral therapy (ART) and antitoxoplasmosis therapy (right image)Aldeen T, Lunn M. Solitary ring enhancing brain lesion in a patient with AIDS. BMJ Case Reports 2009; doi:10.1136 [Citation ends].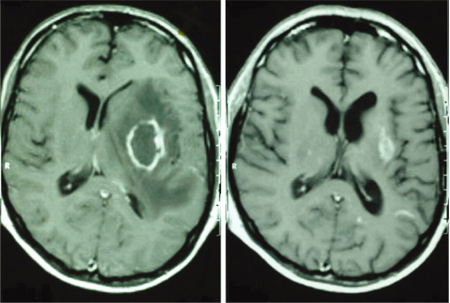
Cryptogenic brain abscess
Most of these are presumed to be bacterial in origin. Single or multiple lesions in a vascular distribution that are suggestive of bacterial abscesses and improve with antibiotic treatment are treated as for bacterial abscess. Lesions clinically suggestive of bacterial abscess upon surgical drainage (e.g., purulence with sterile cultures) are also treated with antibiotics.
Surgical treatment of brain abscesses
Surgery along with antibiotic therapy is the first line of treatment for pyogenic abscesses >2.5 cm in the largest dimension, and the second line of treatment for smaller abscesses that have shown to be refractory to medical therapy. Surgical evacuation offers the advantages of decreasing the infectious burden, obtaining a sample for culture, confirming the diagnosis by sampling the capsular tissue, and relieving the mass effect in the acutely deteriorating patient. Surgery carries the risk of spread of the infectious agent to the ventricular system, resulting in ventriculitis. Open surgery is reserved for large or multi-loculated cortical lesions and cerebellar lesions where obstruction of the cerebrospinal fluid can lead to the rapid decompensation of the patient. Open surgery is also recommended for fungal lesions, because the penetration of antifungal agents across the blood-brain barrier is poor.[3]
Contraindications to surgical excision include the presence of multiple lesions and a deep location of the lesion. When open surgery is performed, a small bone flap is elevated, and the abscess capsule is resected after the contents of the cyst are evacuated, and sent for immediate Gram stain analysis and cultures. The surgical cavity is copiously irrigated, and the bone flap is replaced using a standard plating system. Stereotactic aspiration allows for the relief of mass effect as well as direct culture with less surgical morbidity and, theoretically, less opportunity for iatrogenic ventricular extension.[50] Disadvantages include the need for a repeat procedure in as many as 70% of patients. Aspiration is performed through a single calvarial burr hole with guidance techniques such as frameless neuronavigation (a hand-held imaging device that references stored data of local anatomy), CT guidance, or intra-operative MRI guidance.[3][51][52]
Risk factors for failure of aspiration requiring repeat procedure include inadequate antibiotic coverage, incomplete aspiration, and lack of catheter placement when larger abscesses are drained.[53] A large series of patients in which open surgery, aspiration, or medical management alone was compared found no difference in outcome. However, as these patients were non-randomised, it is likely that the patients who underwent surgical procedures harboured larger lesions and may have been more acutely deteriorating.[54] There are no randomised trials comparing surgical and non-surgical management of brain abscess, and there are not likely to be any such trials in the near future. In the absence of such evidence, a reasonable algorithm is to treat lesions >2.5 cm with aspiration, reserving open surgery for recurrent lesions, lesions in the cerebellum, and fungal lesions.
Use of this content is subject to our disclaimer