Approach
The diagnosis of brain abscess depends on careful clinical evaluation with emphasis on risk factors in the patient's history, along with neuro-imaging studies.[4]
History
Headache, fever, and new-onset neurological deficits are common symptoms of brain abscess.[29] Recent unexplained fever accompanied by neurological deficit should raise immediate suspicion for cerebral abscess.
Elicit whether the patient has a history of sinusitis, otitis media, or recent dental procedure or infection. History of sinusitis or otitis is especially relevant if a lesion is located in the brain adjacent to the affected area. Ask whether the patient was treated with antibiotics, but antibiotic treatment does not exclude the possibility of brain abscess. Patients who have recently undergone a neurosurgical procedure or head and neck surgery are at an increased risk for brain abscess.[2][14] In this group of patients, a history of wound breakdown or drainage from the incision is highly suggestive.
A known history of or potential risk for HIV or immunocompromised state should be ascertained. Males are at slightly greater risk than females for development of a brain abscess. Intravenous drug use is both an independent risk factor for abscess as well as a risk factor for HIV infection. Known pulmonary arteriovenous malformations (AVM), a predisposition for pulmonary AVM from hereditary haemorrhagic telangiectasia, meningitis, congenital heart disease, endocarditis, cystic fibrosis, diverticular disease, diabetes mellitus, chronic granulomatous disease, dialysis, and premature birth are also risk factors.[16][20][23][24][25][26][30][31][32][33][34][35]
The medical history may help distinguish between neoplasm and brain abscess: for example, smoking or a family history of cancer may raise suspicion for malignancy. The timing of onset of symptoms should also be noted, because infectious processes, including brain abscess, tend to present more rapidly than most neoplasms (several weeks to months for the latter). The presentation of malignancy is also less likely to include symptoms of meningismus or fever, and cultures for an infectious source are negative.
The age of the patient is important in determining the most likely source and the most common aetiological agents of infection. In neonates, Proteus mirabilis and Citrobacter species are the most common isolates, while in children Streptococcus species in combination with cyanotic heart disease is most often responsible. In adults, the most common causative microorganisms are Streptococcus and Staphylococcus species.[2] According to observational data from a UK cohort, Streptococcus intermedius has become the predominant agent and there has been a shift away from staphylococcal brain abscesses.[36]
Physical examination
The physical examination is focused on a potential source of infection, with careful inspection of the ears, sinuses, and oral cavity as well as a search for stigmata of sub-acute bacterial endocarditis and intravenous drug use. Signs of malignancy are pertinent clinical negatives. The neurological examination is important in establishing the patient's initial clinical status, but does little to distinguish between abscess and other mass lesions of the central nervous system. Nuchal rigidity, and Kernig and Brudzinski signs in the presence of neurological deficits, are suggestive of abscess. While patients may present with signs of inflammation, their absence does not exclude the presence of a brain abscess, and it is critical that the absence of these findings is not over-interpreted. Furthermore, most patients who present with fever or meningismus without focal neurological deficit do not have brain abscesses.
It is of critical importance to assess for increased intracranial pressure and impending cerebral herniation. Third or sixth cranial nerve palsies, anisocoria, and papilloedema should all prompt immediate imaging when encountered in an obtunded patient suspected of having brain abscess. Head circumference and assessment of the fontanelles are important in the examination of infants with suspected brain abscess.
Tests
Radiological testing
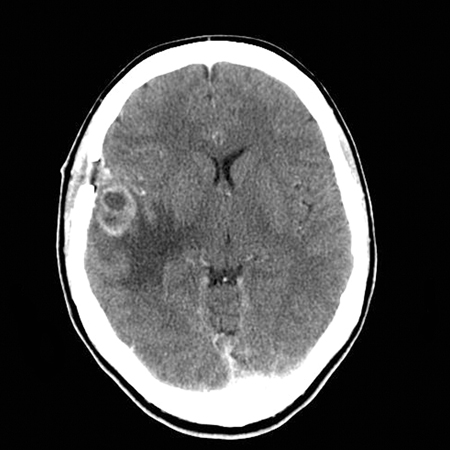
A high index of suspicion is necessary to diagnose brain abscess. Diagnosis in many patients begins with the evaluation of a focal neurological deficit, meningismus, or papilloedema, which in virtually all cases should prompt neuro-imaging with either contrast-enhanced computed tomography (CT) or, preferably, magnetic resonance imaging (MRI).[37] The typical radiological finding in patients with brain abscess (on either CT or MRI) is that of 1 or more ring-enhancing lesions. Although not diagnostic, ring enhancement that is regular with a thin capsule should raise suspicion of brain abscess.[38][Figure caption and citation for the preceding image starts]: CT scan, cerebral abscess within right temporal lobeRafiq MK. An interesting case of cerebral abscess. BMJ Case Reports 2009; doi:10.1136 [Citation ends].
 [Figure caption and citation for the preceding image starts]: Contrast MRI of patient with brain abscessFrom the collection of Walter Hall, SUNY Upstate Medical University [Citation ends].
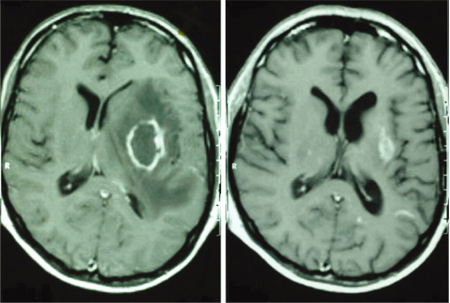
[Figure caption and citation for the preceding image starts]: Contrast MRI of patient with brain abscessFrom the collection of Walter Hall, SUNY Upstate Medical University [Citation ends].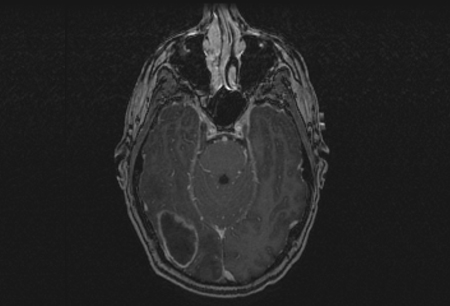
In patients with known HIV infection, or who are otherwise immunocompromised, the threshold for contrast imaging should be low. Persistent headache, signs or symptoms of increased intracranial pressure, and almost any neurological deficit should prompt urgent neuro-imaging studies. The finding of 1 or more contrast-enhancing lesion in such a patient should in turn be investigated with consideration as to the broad spectrum of possible aetiologies. Evidence of mass lesion on whole-body CT imaging is evidence against a brain abscess.[Figure caption and citation for the preceding image starts]: Brain MRI before treatment (left image) and 18 months after antiretroviral therapy (ART) and antitoxoplasmosis therapy (right image)Aldeen T, Lunn M. Solitary ring enhancing brain lesion in a patient with AIDS. BMJ Case Reports 2009; doi:10.1136 [Citation ends].
Ultrasound of the head avoids extensive radiation exposure, but is only useful in infants with open fontanelles.
Magnetic resonance spectroscopy (MRS) is a time-consuming test, and it has been suggested that the analysis of diffusion-weighted imaging sequences of traditional MRI may be more cost effective in most patients.[39] The use of MRS has been recommended by the American College of Radiology if there is the suspicion of a brain infection, especially a brain abscess.[40]
Lumbar puncture (LP)
Should never be performed in any patient with signs of increased intracranial pressure, unless neuro-imaging clearly indicates an absence of intracranial mass lesions and cerebrospinal fluid obstruction.
Performed with extreme caution and only if a lesion is small and Toxoplasma gondii is likely. In the setting of immunocompromise, polymerase chain reaction (PCR) analysis of cerebrospinal fluid (CSF) can support the diagnosis of toxoplasmosis. LP does not play a role when pyogenic abscess is suspected.
Additional tests
Laboratory tests are helpful but never definitive, and should include, at a minimum, full blood count (FBC) with differential, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Leukocytosis, and elevated ESR and CRP, favour abscess over tumour, especially if the patient has not yet received corticosteroids.
Blood cultures should be obtained for any patient with a suspected brain abscess. Positive blood cultures are highly suggestive of the aetiological agent for the abscess.
Preoperative laboratory tests including coagulation profile (platelet count, prothrombin time, partial thromboplastin time, international normalised ratio) should also be ordered immediately for any patient who may need urgent surgical treatment.
In the setting of clinical suspicion for toxoplasmosis, toxoplasma titres are performed.
Bone scan is done as a subsequent test if the patient is not taken for surgery, usually as part of a work-up for metastatic disease. It is usually negative in patients with brain abscess unless there is accompanying osteomyelitis.
Mammography is ordered only if there is a suspicion of breast cancer, such as a family or personal history.
Use of this content is subject to our disclaimer