Aetiology
Brain abscess may arise from infection with bacterial, fungal, or parasitic organisms, with different risk factors for each agent. Bacteria may enter the brain through contiguous spread from a parameningeal site of infection (e.g., sinus, middle ear), or through haematogenous dissemination (e.g., endocarditis).[5]
Any microorganism pathogenic to humans is potentially capable of causing cerebral abscess, and the following list should not be considered complete. Bacterial abscesses may be polymicrobial. Additionally, 10% or more of abscesses are cryptogenic; most of these are presumed to be bacterial in origin.[3] Causative organisms for brain abscess may include:
Bacterial
Streptococcus pyogenes, S milleri, other streptococcal species, Staphylococcus aureus, Bacteroides fragilis, Citrobacter species, Enterobacter species, Klebsiella pneumoniae, Neisseria meningitides, Serratia marcescens, Actinomyces species, Nocardia asteroides, Mycobacterium tuberculosis, Mycoplasma species, Eikenella corrodens, Prevotella species.
Fungal
Aspergillus fumigates, Candida albicans, Cryptococcus neoformans.
Parasitic
Toxoplasma gondii, Trypanosoma species, Echinococcus granulosus, Entamoeba histolytica, Naegleria fowleri, Balamuthia mandrillaris.
[Figure caption and citation for the preceding image starts]: Contrast MRI of patient with brain abscessFrom the collection of Walter Hall, SUNY Upstate Medical University [Citation ends].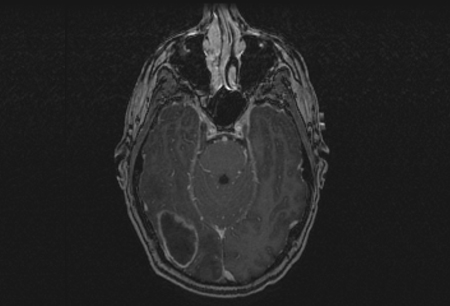 [Figure caption and citation for the preceding image starts]: Brain MRI before treatment (left image) and 18 months after antiretroviral therapy (ART) and antitoxoplasmosis therapy (right image)Aldeen T, Lunn M. Solitary ring enhancing brain lesion in a patient with AIDS. BMJ Case Reports 2009; doi:10.1136 [Citation ends].
[Figure caption and citation for the preceding image starts]: Brain MRI before treatment (left image) and 18 months after antiretroviral therapy (ART) and antitoxoplasmosis therapy (right image)Aldeen T, Lunn M. Solitary ring enhancing brain lesion in a patient with AIDS. BMJ Case Reports 2009; doi:10.1136 [Citation ends].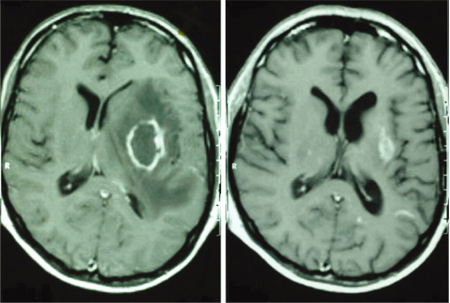
Pathophysiology
Brain abscess most often originates in ischaemic white matter adjacent to the cortex, where increased vascular density may facilitate collagen deposition and capsule formation.[3] Cerebral abscesses proceed through relatively well-characterised stages.[6]
Early cerebritis: lasts approximately 3 days and is characterised by local inflammation, tissue necrosis, neutrophilic infiltrate, and activation of microglia and astrocytes.
Late cerebritis: occurs on days 4 to 9 and is represented by increased organisation where lymphocytic and microglial infiltration is seen.
Frank abscess formation: present after day 10 and is characterised by encapsulation and a suppurative collection.
Entry of organisms into the brain may be through direct extension or haematogenous spread. Haematogenous spread is the most likely route in cases of multiple abscesses and abscesses arising from the grey-white junction. Increased permeability of the blood-brain barrier is present throughout the stages of abscess development, and is apparent by the radiographical finding of contrast enhancement. It allows for better penetration of antibiotics and causes ring enhancement of the abscess on scans.
Use of this content is subject to our disclaimer