Investigations
1st investigations to order
oxygen saturations
Test
Measure oxygen saturations in all patients with suspected HAP.[34]
Result
decreased
chest x-ray
Test
Order a chest x-ray in all patients with suspected HAP as soon as possible.[6]
New and/or persistent shadowing (consolidation) on chest x-ray, which is otherwise unexplained, plus the presence of at least two clinical features (purulent sputum, decline in oxygenation, fever >38ºC [>100ºF], leukocytosis [WBC >10 x 109/L], or leucopenia [WBC <4 x 109/L]) confirms the diagnosis.[1]
In practice, posterior-anterior and lateral views are preferred over anterior-posterior views. Compare with previous chest x-rays if available.
[Figure caption and citation for the preceding image starts]: Portable chest x-ray of a patient with HAP. Note the obscured left hemidiaphragm due to a left lower lobe opacity and an obscured heart border due to a left upper lobe or lingular opacityConsent obtained at University of Louisville, Louisville, KY [Citation ends].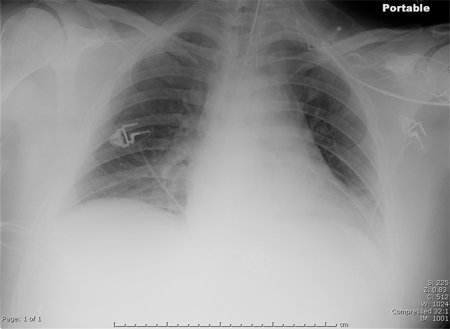
Result
new and/or persistent consolidation
full blood count
Test
Request a full blood count in all patients with suspected HAP to help determine the severity of illness.
Result
may show leukocytosis (WBC >10 x 109/L) or leucopenia (WBC <4 x 109/L)
blood gas
Test
Measure blood gas (including lactate levels). In practice, venous blood gas is preferable to arterial blood gas.
Obtaining a blood gas while the patient is not yet receiving supplemental oxygen provides a more accurate reflection of the oxygenation status, but should not delay supplemental oxygen from any unstable patient.
Result
may show:
hypoxia
respiratory alkalosis
metabolic acidosis (due to hypotension, reduced tissue perfusion, or acute kidney injury)
raised lactate levels
C-reactive protein
Test
Request in all patients with suspected HAP to help rule out other acute respiratory illnesses and as a baseline measure.
High levels of CRP do not necessarily indicate that pneumonia is bacterial or SARS-CoV-2, but low CRP levels make a secondary bacterial infection less likely.[45]
Result
elevated
renal and liver function tests (LFTs)
Test
Request in all patients with suspected HAP to help determine the severity of illness. It can indicate the presence of multiorgan dysfunction.
Pneumonia can cause renal impairment and abnormal LFTs, although this is more likely in someone with pre-existing renal or liver disease.
Result
may be abnormal, particularly if there is underlying or associated pathology
culture of sputum, nasopharyngeal swab, or tracheal aspirate samples
Test
Take sputum samples for culture first, ideally before antibiotics are started.[6][7]
The patient needs to be able to produce a good specimen, which may not be the case in patients with HAP.[52]
Take other non-invasive respiratory samples (nasopharyngeal swab or tracheal aspirate) if the patient cannot produce sputum.[6][7]
Practical tip
Positive cultures need to be correlated clinically. They may be false positives showing evidence of colonisation of the trachea or false negatives due to prior antimicrobial treatment.
Result
growth of causative bacterial pathogen
Investigations to consider
CT scan chest
Test
Consider a chest CT scan:
When there is diagnostic doubt: for example, if the chest x-ray is of poor quality or there is an ill-defined consolidation[6]
In patients with a complex chest x-ray who do not respond to treatment (to guide treatment)[36]
When the chest x-ray shows ‘complicated’ pneumonia or atypical changes, such as cavitation, multifocal consolidation pattern, or pleural effusion.[35] See Differentialssection.
[Figure caption and citation for the preceding image starts]: CT scan showing bi-basilar opacities in a patient with HAPConsent obtained at University of Louisville, Louisville, KY [Citation ends].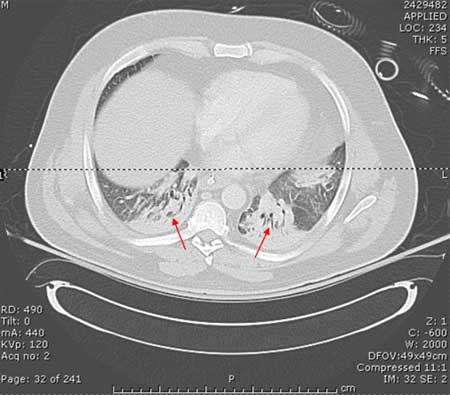
Result
may show an opacity or clarify findings if radiograph is of poor quality
chest ultrasound
Test
Consider chest ultrasound following chest x-ray when there is diagnostic doubt.[34]
Pleural effusion seen on chest x-ray may prompt you to perform a chest ultrasound (with or without guided aspiration and chest CT) to help make an alternative diagnosis such as tuberculosis, lung cancer, or pulmonary embolism.
[Figure caption and citation for the preceding image starts]: Left-sided pleural effusionFrom the collection of Dr R Light; used with permission [Citation ends].
Result
consolidation may be seen; parapneumonic effusion may be seen
thoracocentesis and pleural fluid culture
Test
Arrange an early thoracocentesis in all patients with pleural effusion as this can reveal an infected pleural space consistent with a parapneumonic effusion.[34]
Aspiration of pus and/or a positive Gram stain of pleural fluid indicates an empyema.
Drain the pleural fluid in patients with an empyema or clear pleural fluid with pH <7.2.[34]
Result
purulent exudate; positive Gram stain or culture
urine antigen testing
PCR and/or serological tests including for SARS-CoV-2
Test
Consider polymerase chain reaction (PCR) or serological investigations of sputum, nasopharyngeal swab, or tracheal aspirate if there is a strong suspicion of respiratory viruses (influenza A and B, parainfluenza 1–3, adenovirus, respiratory syncytial virus) or atypical pathogens.[34]
Viruses and atypical pathogens are less commonly associated with HAP than with CAP.[34]
PCR (if available) is preferred over serological investigations.[34]
During the COVID-19 pandemic, order a nucleic acid amplification test, such as real-time PCR, for SARS-CoV-2 in any patient with suspected infection whenever possible.[37][38] See Coronavirus disease 2019 (COVID-19) .
Result
detection of viral/atypical pathogen antigens or antibodies
serum procalcitonin
Test
Although currently excluded from key guidelines, baseline procalcitonin is increasingly being used in critical care settings and in the emergency department to guide decisions on antibiotic treatment in patients with highly suspected sepsis and in those with suspected bacterial infection.[41][46][47][48][49]
Elevated procalcitonin is correlated with bacterial pneumonia, whereas lower values are correlated with viral and atypical pneumonia. Procalcitonin is typically markedly elevated in people with pneumococcal pneumonia.[50][51]
Procalcitonin is a peptide precursor of calcitonin, which is responsible for calcium homeostasis.
Result
may be elevated
Use of this content is subject to our disclaimer