Differentials
Common
Transient synovitis of the hip (toxic synovitis/irritable hip)
History
age between 2 and 12 years; more common in boys; hip motion may be limited; pain on hip movement; may be history of upper respiratory illness
Exam
patient will usually allow movement through a limited arc of motion; restriction of motion may be particularly apparent in abduction and internal rotation; some patients do not display any restriction in hip movement; may be tenderness on palpation of the hip or groin; patient will typically be able to walk, but with a noticeable limp and for limited distances; positive log roll (patient lies supine and the leg is rolled gently from side to side. A positive test results in involuntary muscle guarding in the affected limb); patient will typically rest with hip abducted and externally rotated; temperature <38.5°C (<101.3°F)
1st investigation
- FBC:
WBC count may be slightly elevated
- erythrocyte sedimentation rate (ESR)/CRP:
ESR may be slightly elevated, CRP may be slightly elevated
- x-ray of hip:
typically normal; may reveal subtle signs early in the disease process, such as capsular distension, joint space widening, diminution of the definition of soft tissue planes around the hip joint, or slight de-mineralisation of the bone of the proximal femur
More
Other investigations
- ultrasound:
effusion (increased fluid in joint)
More
Toddler's fracture (spiral non-displaced fracture of tibia with fibula intact)
History
young child (≤4 years of age); trauma/falls (especially rotational injury); trauma may be unwitnessed; child may present as reluctant to weight-bear (antalgic gait); pain often not localised or non-vocalised (child is distressed); consider child abuse if incongruous history and inconsistencies in the history from carer and other injuries are present
Exam
tenderness along shaft of the tibia (uni-lateral), often no swelling or discoloration
1st investigation
- x-ray lower limb:
spiral fracture
More
Other investigations
Legg-Calvé-Perthes disease
History
age 4 to 10 years (median age 6 years); limp; antalgic gait; pain often referred to thigh or knee; may be indolent history (weeks) or sub-acute (days); may be recent history of transient synovitis
Exam
typically a well child with antalgic gait, reduced flexion and internal rotation of hip
1st investigation
- x-ray of hip (including frog view):
flattening, sclerosis, and ultimately fragmentation and collapse of femoral epiphysis, with widening of femoral neck
More
Other investigations
- MRI of hip:
reduced vascularity of the femoral head may be seen in early disease; flattening, sclerosis, and ultimately fragmentation and collapse of femoral epiphysis, with widening of femoral neck
More
Non-accidental injury
History
inconsistent/incongruent history from parent/carer (e.g., fractures in a non-mobile child); frequent hospital visits and injuries; delay in presentation to healthcare practitioner; recurrent trauma episodes without adequate explanation; very young age (one third <12 months; half <2 years)
Exam
signs of neglect and/or poor growth; certain behaviour or emotional states that cannot be explained by medical causes and are inconsistent with the child’s age and development (e.g., appearing fearful or withdrawn, or displaying over-friendliness to strangers or excessive clinginess); suspicious pattern of injury (metaphyseal 'bucket handle' fractures, posterior rib fractures, spiral fractures, unexpected old fractures); injuries at various sites in various stages of healing and distinct from expected injuries in active pre-school child (bruises, finger marks, burns, scratches, scalds); guarding or reduced range of movement; palpable callus in healing fractures (shin bruises, knee grazes); antalgic gait; limp
1st investigation
- x-rays of suspicious areas:
soft-tissue swelling, fractures, callus from healing fractures
More
Osgood-Schlatter disease
History
active older child or adolescent; more frequent in boys, often during periods of active growth; pain after activity in knees, exacerbated by certain sports (e.g., football)
Exam
painful, tender swelling of anterior tibial tuberosity
1st investigation
- x-ray of tibia:
expanded, occasional fragmented, tibial tuberosity
More
Other investigations
Juvenile idiopathic arthritis (JIA)
History
age <16 years at onset, history varies by sub-type; oligoarticular JIA (<5 joints affected in first 6 months): most common, peak pre-school age, more frequent in girls, well child with indolent limp, diurnal variation, gelling after rest, pain may be non-vocalised and include behaviour changes in younger child (irritability, sleep disturbance), regression in achieved motor milestones (e.g., walking), older children, particularly boys, may have history of localised joint involvement (hip, knee, ankle) or painful red eye, which suggests HLA B27-related arthritis; polyarticular JIA: more common in girls and older child, fatigue, low-grade fevers, rash, malaise, may be acute, sub-acute or indolent presentation; systemic JIA: unwell, high swinging fever (worse in evenings), rash, malaise, arthralgia, myalgia, sore throat, often acute presentation
Exam
oligoarticular JIA: well child, limp, asymmetric involvement of the knee and or ankle most common, joint effusion, limited joint movement, evidence of chronicity suggested by muscle wasting, contractures; accompanying enthesitis (heel, knee, sole of foot), often in older boys, suggestive of enthesitis-related arthritis (HLA B27 related); polyarticular JIA: low-grade fever, pallor, rash, symmetric joint involvement (upper and lower limbs, neck); systemic JIA: fever (quotidien), rash (maculopapular at time of fever), lymphadenopathy, hepatosplenomegaly, pericarditis; skin (scalp, umbilicus, natal cleft) and nails (pitting) involvement
1st investigation
Other investigations
- FBC and blood film:
leukocytosis (neutrophilia), anaemia, thrombocytosis
More - erythrocyte sedimentation rate (ESR)/CRP:
elevated
- x-ray of joints/limbs:
soft-tissue swelling, effusion, peri-articular osteoporosis
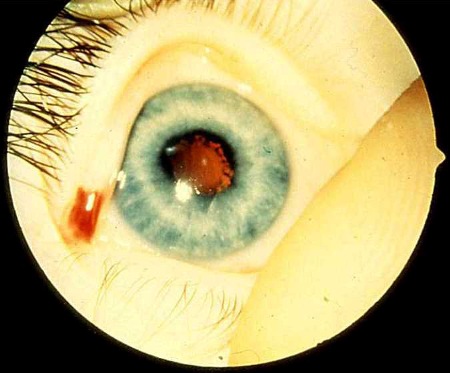
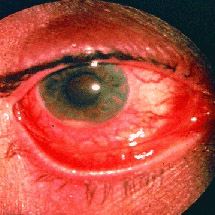
More - slit lamp examination:
chronic anterior uveitis
More - HLA-B27:
positive
More - ferritin:
elevated ferritin suggests systemic-onset JIA
More - bone marrow tests:
normal
More - clotting screen:
negative
More
Cerebral palsy
History
perinatal history may include prematurity; infection in pregnancy; low birth weight, hypoxia, or multiple births; postnatal history of meningitis; early irritability; feeding difficulties; failure to thrive; delay in motor milestones (may show persistent toe walking); motor asymmetry including early hand preference (<18 months); delay in speech, hearing, vision or fine motor skills; learning difficulties; clumsy/poor balance; delayed continence; behavioural problems; epilepsy[44]
Exam
abnormalities of tone including hypotonia, increased tone and dystonia; clonus; hyperactive reflexes; persistent primitive reflexes (>6 months); possible global developmental delay (speech, hearing, vision and fine motor skills, learning difficulties); poor growth parameters; spastic cerebral palsy (most common) includes hemiplegia (weak hip flexion, ankle dorsiflexion, hip hiking/circumduction, upper extremity posturing); diplegic gait; scissoring gait (hips flexed and adducted, knees flexed with valgus stress, equinus ankles); ataxic cerebral palsy includes wide based unsteady gait; athetoid cerebral palsy: exaggerated step, hip and knee hyper-extension, backwards lean
1st investigation
- none:
diagnosis is usually clinical
More
Other investigations
- brain imaging (MRI/CT scan):
congenital malformations, intracranial haemorrhage, periventricular leukomalacia, focal infarcts, cortical/subcortical lesions
More - congenital infection screen:
may be positive
More - genetic testing:
may show evidence of chromosomal disorder such as Angelman's syndrome
More - screening tests for other causes of developmental delay:
results vary according to cause; may show raised muscle enzymes, abnormal thyroid function, low/normal calcium, low phosphate, low vitamin D
More
Spina bifida
History
abnormal screening test (alpha fetoprotein); abnormal ultrasound scan in pregnancy; delayed motor milestones (especially gross motor milestones involving lower limbs); disturbance of continence; orthopaedic problems; hydrocephalus
Exam
hairy naevus; midline lipoma; haemangioma over lumbosacral spine; complex multi-system involvement with both upper and lower motor syndromes; variable neurological deficits; spinal deformity (scoliosis, kyphosis); lower limb flaccid paralysis; progressive lower extremity contractures; hip dislocations; foot varus deformity or equinovarus (clubfoot); possible limb deformities; hydrocephalus; ambulation dependent on level of lesion; gait features include overall lower limb hypotonia, flexed posturing of the lower limbs and possibly steppage gait
1st investigation
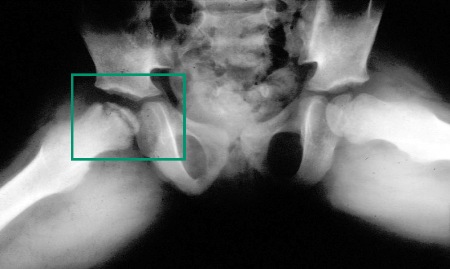
- x-ray of hip:
abnormal relationship between femoral head and acetabulum
More - plain films and advanced imaging modalities (e.g., MRI):
incomplete union of the posterior elements of vertebral levels demonstrating various degrees of failure of neural tube closure.
Other investigations
Appendicitis
History
adolescent or young adult, abdominal pain, anorexia, nausea, fever
Exam
right lower quadrant abdominal tenderness (McBurney's sign); localised rebound tenderness, if appendix is anterior; pain in the right lower quadrant after compressing the left lower quadrant (Rovsing's sign); diminished bowel sounds
1st investigation
- FBC:
mild leukocytosis (10,000-18,000/microlitre), increased polymorphonuclear leukocytes (>75%)
More
Other investigations
Uncommon
Slipped capital femoral epiphysis
History
well child; acute or indolent limp; antalgic gait; groin pain or pain referred to knee; older child or adolescent (peak age 11 to 15 years); associated with obesity, hypothyroidism, and delayed secondary sexual characteristics; more frequent in boys; bilateral in one third of patients
Exam
well child, often obesity, affected leg may be short, leg held in flexion and external rotation, thigh atrophy
1st investigation
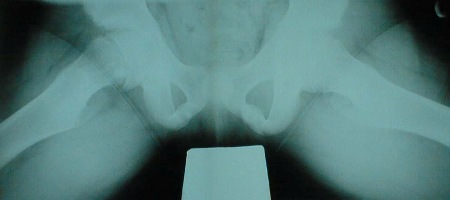
- x-ray of both hips (frog views required):
slipped capital femoral epiphysis
More
Other investigations
Developmental hip dysplasia
History
first-born females; breech birth; family history; oligohydramnios; late diagnoses may present with delayed walking
Exam
neonates: clicky hips, positive Barlow's manoeuvre, positive Ortolani's manoeuvre; older child/toddler: leg length discrepancy (short ipsilateral side), asymmetric skin creases (posterior thigh), positive and bi-lateral Trendelenberg's gait (rolling-waddling gait)
1st investigation
- x-ray both hips:
dislocated/dysplastic hips
More
Other investigations
- ultrasound both hips:
dislocated hips
More
Tarsal coalition
History
older child or adolescent; painful rigid flat feet; chronic pain after walking; limping; can be unilateral
Exam
non-mobile painful flat feet; neurological examination normal (to exclude neurological disorder such as spina bifida)
1st investigation
- x-ray of feet:
additional bone/cartilaginous bar in medial arch
More
Other investigations
- CT of feet:
cartilaginous bar in medial arch
More
Sever's disease
History
active older child or adolescent; more frequent in boys, often during periods of active growth; pain after activity in heel
Exam
painful heel, tender posterior calcaneum, distal to Achilles tendon insertion
1st investigation
- x-ray of heel:
expanded, occasional fragmented calcaneum
More
Other investigations
Spondylolysis
History
may be asymptomatic; preceding trauma; pain with extension and/or rotation of the lumbar spine; it is associated with certain sports (e.g., fast bowler in cricket, gymnastics)
Exam
abnormal gait; spinal abnormalities, areas of spinal tenderness and muscle spasm; numbness; paraesthesias; extremity sensation, and motor function; muscle spasm; weakness; bowel/bladder changes; loss of vertebral disc height; presence of osteophytes; disc, ligament, and nerve abnormalities
1st investigation
- x-ray of lumbar spine:
loss of vertebral disc height, presence of cracks, fractures, and osteophytes
More
Juvenile dermatomyositis
History
children of all ages; indolent presentation common; fatigue; rash (photosensitive, face, neck and arms); myalgia; arthralgia; regression of motor milestones (walking, running, going up and down stairs, difficulty swallowing/speaking)
Exam
muscle weakness (proximal) with positive Gower's sign; Trendelenberg's gait; rash (face, neck, arms, heliotrope over eyelids); Gottron's papules (purple keratotic atrophic lesions often on the back of hands, knees, elbows); calcinosis suggests chronicity and poor disease control; nailfold capillary loop dilatation; arthritis usually mild and affecting small joints; difficulty with swallowing; altered (nasal) speech or intermittent cough may suggest bulbar involvement and warrants urgent assessment
1st investigation
- muscle enzymes:
elevated creatinine phosphokinase, aldolase, lactate dehydrogenase, and alanine transaminase levels
More - antinuclear antibodies (ANA) and other myositis-specific antibodies:
positive
Other investigations
- MRI of muscles:
muscle oedema, inflammatory changes in skin, subcutaneous tissue, fascia
More - muscle biopsy:
inflammatory lymphocytic cell infiltrate, characteristic increased MHC class I expression
More - pulmonary function tests:
restrictive pattern is suggestive of chest wall weakness
More - speech and language assessment:
swallowing, speech difficulties, or cough suggests bulbar involvement
More - electromyography (EMG):
spontaneous fibrillations, decreased amplitude polyphasic, short duration of action potentials
More
Systemic lupus erythematosus (SLE)
History
female; age 15 to 45 years; African/Asian descent in Europe and US; fatigue; weight loss; fever; oral ulcers; alopecia; malar (butterfly) rash; photosensitive rash; discoid rash; arthralgia/arthritis; fibromyalgia; chest pain and shortness of breath; vomiting or diarrhoea
Exam
fever; oral ulcers; alopecia; malar (butterfly) rash; photosensitive rash; discoid rash; arthralgia/arthritis; Raynaud's phenomenon; hypertension; lymphadenopathy; abdominal pain; venous or arterial thrombosis
1st investigation
- antinuclear antibodies (ANA), double-stranded DNA (dsDNA), Smith antigen, extractable nuclear antigen (ENA) (Ro and La):
positive
More - FBC and differential:
anaemia, leukopenia, thrombocytopenia; rarely pancytopenia
More - activated PTT:
may be prolonged in patients with antiphospholipid antibodies
More - urea and electrolytes:
elevated urea and creatinine
More - erythrocyte sedimentation rate (ESR)/CRP:
elevated (non-specific)
More
Septic arthritis
History
age usually under 10 years (generally 3 to 7); hip most common site; sudden-onset limp; refusal to sit, stand, or walk; illness, irritability, or fever; may be localised pain (severe) referred to thigh, groin, or knee; family history of hand-foot syndrome; history of travel to an endemic area for Lyme disease with acute/subacute monoarthritis; consider history of foreign travel/gastroenteritis with reactive arthritis (especially if also acute red eye); consider sexual history in older child/adolescent with reactive arthritis (acute monoarthritis or oligoarticular presentation)
Exam
refusal to weight-bear or walk; refusal to sit (consider spinal abscess, hip disease); swollen, tender, immobilised joint; pseudoparalysis in very young; tender, paraspinal muscle spasm (discitis/spinal abscess)
1st investigation
- joint aspiration and synovial fluid culture:
fluid appears turbid, raised white cell count in fluid, gram stain, and stains for acid-fast bacilli
More - blood culture:
positive growth
More - Lyme-specific IgM and IgG:
positive
More - FBC and blood film (± electrophoresis):
leukocytosis >10x10^6, Howell-Jolly bodies (sickle cell disease)
More - erythrocyte sedimentation rate (ESR)/CRP:
very elevated
More - x-ray of bone/joint:
soft-tissue swelling, effusion, periosteal elevation, osteopenia, fragmentation
More
Other investigations
- CT of bone/joint:
hot spots to show foci of infection
More
Osteomyelitis
History
age usually below 10 years (generally 3 to 7 years); hip most common site; sudden-onset limp; refusal to sit, stand or walk; illness, irritability, or fever; may be localised pain (severe) referred to thigh, groin, or knee; family history of hand-foot syndrome
Exam
refusal to weight-bear or walk; refusal to sit (consider spinal abscess, hip disease); swollen, tender, immobilised joint over the metaphysis; pseudoparalysis in very young; tender, paraspinal muscle spasm (discitis/spinal abscess)
1st investigation
- joint aspiration and synovial fluid culture:
fluid appears turbid, raised WBC in fluid, Gram stain, and stains for acid-fast bacilli
More - blood culture:
positive
More - erythrocyte sedimentation rate (ESR)/CRP:
elevated: ESR >100 mm/hour, CRP >95.2 nanomol/L (>10 mg/L)
More - x-ray of joint:
infected areas typically appear dark, soft-tissue swelling, effusion, periosteal elevation, osteopenia, fragmentation
More
Other investigations
- CT of joint:
hot spots show foci of infection
More
Charcot-Marie-Tooth disease (CMT)
History
significant family history; slowly progressing weakness (begins in distal limb muscles); onset usually under 20 years; difficulty walking/tripping; frequent ankle sprains/falls; steppage; pes cavus; symptoms related to foot abnormalities (calluses, ulcers, cellulitis, lymphangitis); hand weakness; possibly pain (musculoskeletal and neuropathic types); muscle cramping; autonomic symptoms are usually absent
Exam
stork leg or inverted champagne bottle appearance; pes cavus; spinal deformities; absent or diminished deep tendon reflexes; decreased vibration sensation; possibly sensory gait ataxia (Romberg's test usually positive); sensation of pain; essential tremor; enlarged/palpable peripheral nerves; phrenic nerve involvement is rare; vocal cord involvement and hearing loss can occur in rare forms
1st investigation
- electromyography (EMG):
marked slowing of nerve conduction (sensory and motor)
More
Other investigations
- genetic testing:
gene mutation associated with specific CMT subtype
More
Muscular dystrophies
History
more frequent in boys, delayed walking (>18 months), family history (carrier status)
Exam
proximal muscle weakness (Gower's sign positive), Trendelenberg's gait, inability to jump, prominent but weak 'pseudo-hypertrophied' calf muscles (symmetric), cardiomyopathy, scoliosis, non-ambulant by teenage years
1st investigation
Other investigations
- muscle biopsy:
necrosis, marked variation in muscle fibre size
More - electromyography (EMG):
decrease in duration and area to amplitude ratio of the action potential, decrease in the number of motor units in the muscle
More - TFTs:
normal
More - infection screen (coxsackie, influenza, echo viruses):
normal
More - calcium, vitamin D, urea and electrolytes tests:
may show low/normal calcium, low phosphate, low vitamin D levels, low 1,25-OH vitamin, low serum bicarbonate, high serum chloride
More
Haemophilia
History
toddler or preschool boy (girls usually carriers); possible family history (X-linked recessive inherited); bruising; bleeding tendency; soft-tissue and muscle haematomas; haemarthrosis with minor trauma; gum and tongue bleeding
Exam
antalgic gait, bruises, ecchymoses (often unusual sites and disproportionate to trauma), haemarthrosis (chronic joint involvement without adequate treatment results in deformity), muscle wasting; contracture
1st investigation
Other investigations
- genetic screening:
DNA-based analysis of the X chromosome to identify a specific genetic mutation
More
Sickle cell disease
History
abdominal pain; acute crises affecting bones and joints; infection (fever, cough, urinary symptoms, shortness of breath or dyspnoea); aphasia; unilateral weakness; paraesthesias; visual blurring; neck stiffness; severe headaches; pallor; syncope; surgical history; previous haemoglobin levels and transfusions; preceding trauma; family history of sickle cell disease; immunisation history (pneumococcal, influenza or hepatitis B); more common in black children
Exam
dactylitis, tachycardia, frontal and parietal bossing and prominent maxilla, longer than normal extremities; pain, swelling, and warmth of the involved extremity
1st investigation
Other investigations
- blood culture:
negative
More
Leukaemia
History
joint and bone pain, fatigue, malaise, bruising
Exam
unwell, low-grade fever, pallor, bone/joint tenderness, soft-tissue swelling, joint effusion, abdominal masses/organomegaly
1st investigation
Other investigations
- bone marrow biopsy:
blasts and abnormal primitive cells, cytopenia
Neuroblastoma
History
most common in children under 5 years; joint and bone pain; limp; fatigue; malaise; bruising; headache
Exam
unwell; unexplained fever or bone pain; enlarged lymph nodes; pallor; bone/joint tenderness; soft-tissue swelling; joint effusion; abdominal masses/organomegaly
1st investigation
Other investigations
- bone marrow biopsy:
cytopenia, malignant cells or infiltration
Benign bone tumour
History
most common osteoid osteoma; localised aching or 'boring' nature of pain, worse at night and increasing with rest or elevation; night pain often relieved by NSAIDs; limping; stiffness; most common sites are proximal femur, spine, and proximal tibia
Exam
well child; afebrile; may be limping, localised tenderness (bone/joint); soft-tissue swelling; may be joint effusion if sited near joint; scoliosis may be apparent if sited in spine
1st investigation
- x-rays of the bone:
may be normal; typical change is solitary lucent nucleus surrounded by sclerosis (nidus)
More
Other investigations
- FBC and blood film:
normal
More - erythrocyte sedimentation rate (ESR)/CRP:
normal
More - bone scan:
hot spot
More - MRI or CT of bone:
typical change is sclerotic central nidus surrounded by granulation tissue and in turn surrounded by sclerotic reactive bone
More - biopsy:
nidus is composed of osteoid, bone and blood vessels surrounded by a fibrovascular layer
Osteosarcoma
History
adolescent or young adult (15 to 25 years), more frequent in males; asymmetric persistent deep pain, most common site in thigh, knee, occasionally heel, pain is worse at night and not related to activity; weight loss, malaise and low-grade fever
Exam
unwell, low-grade fever, pallor, bone/joint tenderness, soft-tissue swelling, joint effusion, abdominal masses/organomegaly; arises in metaphysis and most common sites are around the knee (distal femur/upper tibia) and proximal humerus; tumour are highly malignant and metastasise early (and to lungs in particular)
1st investigation
Ewing's sarcoma
History
most common in early adolescents (10 to 15 years); asymmetric persistent deep pain and local swelling, most common sites: mid thigh and shin knee, systemic features such as weight loss and low-grade fever are common; very malignant and metastasises early (lungs and other bones)
Exam
unwell, low-grade fever, pallor, bone/joint tenderness, soft-tissue swelling, joint effusion, abdominal masses/organomegaly; arises in diaphysis of long bones, most common sites: femur, humerus, or tibia, or innominate bone, but can be present in any bone including spine
1st investigation
Rickets
History
all ages especially toddler and preschool; association with chronic renal disease and malabsorption syndromes (coeliac disease); family history (X-linked hypophosphataemic vitamin D-resistant rickets); failure to thrive; developmental delay (motor); regression in motor milestones; limb pain
Exam
small, thin size, bowing of long bones (genu varum); proximal muscle weakness; Trendelenberg's gait; short height (<25th centile) suggests hypophosphataemic vitamin D-resistant rickets
1st investigation
Other investigations
Lysosomal storage disorders
History
toddler and preschool child, family history of lysosomal storage disorders, failure to thrive, hypotonia (infants), developmental delay (motor), recurrent otitis media, cardiorespiratory symptoms, cytopenias, limb and bone pain, temperature changes intolerance, impaired sweating; more subtle forms can present with predominantly musculoskeletal features without multi-system features (clumsy walking, persistent toe walking, poor hand function, and finger stiffness with no diurnal variation and no response to NSAIDs
Exam
severe forms: short stature, thin, dysmorphic features, hepatosplenomegaly, cardiomegaly, corneal clouding, proximal muscle weakness, scoliosis; milder forms: joint contractures, trigger finger, carpal tunnel syndrome with no evidence of inflammatory arthritis/tenosynovitis
1st investigation
- urine for glycosaminoglycans:
raised glycosaminoglycans levels
More
Complex regional pain syndrome
History
adolescent females predominantly; association with high achievers at school/sports; severe debilitating pain; often minor trauma; incongruence between reported pain, distress and physical signs; often non-weight-bearing, limp, or wheelchair use; common sites are foot, ankle, and occasionally knee
Exam
diffuse swelling; mottling and allodynia with dysaesthesia and hyper-sensitivity; foot and ankle may be held flexed and abnormal posturing may be evident (especially with hand or foot involvement); site may be cold, sweaty, and cyanosed, with muscle wasting and contracture if chronic; gait may be bizarre and inconsistent
1st investigation
- none:
diagnosis is usually clinical
Use of this content is subject to our disclaimer