Investigations
1st investigations to order
Gram stain of urethral discharge and/or urine sediment
Test
Gram stain is rapid, sensitive, and specific for establishing the presence or absence of gonorrhoeal infection. Confirms presence of urethritis. Presence of gram-negative diplococci strongly suggests Neisseria gonorrhoeae, but does not exclude other causes of urethritis. Lack of gram-negative diplococci does not rule out gonorrhoea. Gram stain may fail to identify up to 5% of gonorrhoea cases.[2][37][Figure caption and citation for the preceding image starts]: Gram stain of urethral exudate showing gram-negative diplococci and polymorphonuclear leukocytesAdapted from Public Health Image Library, CDC (Jacobs N, 1974) [Citation ends].
Result
≥2 polymorphonuclear leukocytes per high power field plus documented urethral discharge diagnostic for urethritis; presence of gram-negative diplococci diagnostic for gonorrhoeal infection
nucleic acid amplification tests (NAAT)
Test
Non-culture tests, such as nucleic acid hybridisation tests and NAATs, are now available and are recommended as first-line methods of testing.[1][31][32]
Useful for urine and urethral specimens.
Most sensitive method to detect gonorrhoea in urine specimens.
Testing with NAAT for N gonorrhea, C trachomatis, and M genitalium should be done in people who meet the criteria for urethritis, even if initial Gram stain tests are negative for evidence of gonococci.[27][28]
Result
may diagnose Neisseria gonorrhoeae, Chlamydia trachomatis, or M genitalium
culture of urethral discharge
Test
Specificity is close to 100%, but sensitivity ranges between 85% and 95% (under optimal conditions) for gonorrhoea.[33] Culture is required as a test of cure to evaluate suspected cases of gonorrhoea treatment failure and to monitor developing resistance to current treatment regimens.
While specificity is very high for Chlamydia trachomatis, culture methods are technically demanding and relatively insensitive, such that NAATs have replaced culture as the definitive diagnostic test for chlamydia.[34]
Culture is not recommended as a reliable indicator for Mycoplasma species, as it is a slow-growing organism.[35]
[Figure caption and citation for the preceding image starts]: McCoy cell monolayers with Chlamydia trachomatis inclusion bodiesAdapted from Public Health Image Library, CDC (Arum E and Jacobs N, 1975) [Citation ends].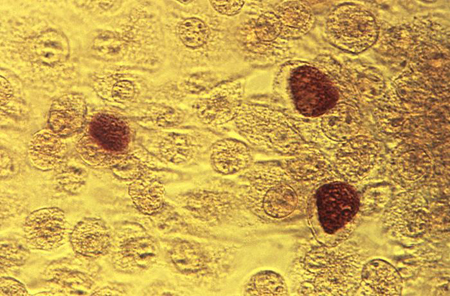
Result
chocolate agar positive for Neisseria gonorrhoeae; inoculate cell monolayers such as McCoy or Buffalo green monkey kidney for C trachomatis
potassium hydroxide prep of urethral discharge
Test
Useful to rule out candidal infection if the Gram stain, done initially to rule out gonococcal urethritis, shows candidal hyphae.
Result
may detect fungal hyphae
HIV test
Result
may be positive
syphilis test
Result
may be positive
Investigations to consider
urinalysis and culture
Test
Presence of ≥10 polymorphonuclear leukocytes (PMNs) per high power field is consistent with either urinary tract infection (UTI) or urethritis. Urine culture is useful to rule out other bacterial infections causing UTI if otherwise unable to differentiate between urethritis and UTI.
Result
detection of leukocyte esterase (≥10 PMNs per high power field)
wet mount of urethral discharge (women)
Test
Diagnostic tool available for diagnosis of T vaginalis in women, but difficult to obtain in men. If negative, a specimen should be sent for NAAT. In men, NAAT and culture of urine or urethral swab can be done (sensitivity 80%).[2]
Result
may detect Trichomonas vaginalis
NAAT and culture of urine or urethral/vaginal swab for Trichomonas vaginalis
Test
NAAT may be done on urine or urethral/vaginal swab, if symptoms persist after treatment for Neisseria gonorrhoeae and Chlamydia trachomatis.[30][38]
In men, NAAT and culture of urine or urethral swab has sensitivity of 80%.[2][30] In men, wet mount is difficult to perform so urine or urethral swab is preferred. For women, vaginal swabs for NAAT or wet mounts can be done.
Result
may detect T vaginalis
NAAT for other organisms
Test
NAATs for other organisms, such as Mycoplasma hominis, Ureaplasma urealyticum, and Ureaplasma parvum,are available but not all laboratories have them. These organisms may be suspected after initial treatment failure, if typical causative agents (Neisseria gonorrhoea, Chlamydia trachomatis, Mycoplasma genitalium, Trichomonas vaginalis) have been excluded.[36]
Result
rapid detection of M hominis, U urealyticum, and U parvum
Use of this content is subject to our disclaimer