Approach
An accurate history is essential to help differentiate between infectious and non-infectious causes of urethritis. A sexually active person presenting with urethral discharge or irritation should be evaluated for gonococcal urethritis (GU) and non-gonococcal urethritis (NGU). The criteria for clinical diagnosis usually include documenting urethral discharge, along with ≥2 polymorphonuclear leukocytes (PMNs) per high power field in the discharge or ≥10 in sediment from a first-void urine. Urine culture will be negative for enteric pathogens. Because of significant overlap in symptoms, GU and NGU should not be differentiated clinically.[2][25]
History and general physical exam
A comprehensive history should rule out trauma and other non-infectious causes of urethritis. If infection is suspected, an accurate sexual history is essential. Important elements include number of partners, any new partners, the onset of symptoms after the last sexual contact, type of sexual exposure, use of condoms and other contraceptive methods, and history of prior sexually transmitted infections (STIs; including HIV infection) in self or partner. Use of spermicides can cause a chemical urethritis, mimicking infection. Additional key risk factors include age between 15 and 24 years, low socio-economic class, multiple sex partners, and prior or current STI. The review of systems may reveal urethral discharge; dysuria without frequency or urgency; irritation or itching; or orchialgia (a feeling of heaviness in the male genitals).[2][26] The onset of symptoms usually occurs between 4 days and 2 weeks after contact with an infected partner.
Systemic symptoms are absent in uncomplicated urethritis. Women may have concurrent cervicitis (diagnostic approach and treatment remain the same). The presence of fever, urinary frequency or urgency, genital pain, arthritis, pneumonia, back or flank pain, and pustular or petechial rash (disseminated gonorrhoea) suggest alternative diagnoses or complications.[2][26]
The patient should be examined either in the morning or at least 2 hours after the last micturition. Urination temporarily washes away discharge and potentially culturable pathogens. When the patient undresses, the underwear should be examined for dried discharge. For the purposes of examination, men may be standing or supine; women should be in the lithotomy position.
Evidence for other STIs should be sought because they are common in patients with urethritis. The entire external urogenital system should be visualised for lesions, ulcers, and nits/lice. The region should be palpated for lymphadenopathy, masses, and tenderness. If a foreskin is present, it should be retracted for adequate evaluation of the meatus for discharge, crusting, and redness. If no discharge is seen, the urethra should be gently milked. In men, the prostate should be checked for bogginess and tenderness to determine the possibility of prostatitis.[2][26] Infants born to mothers with urethritis and/or cervicitis may present with conjunctivitis and ophthalmia neonatorum. Uveitis in conjunction with reactive arthritis has also been described.[Figure caption and citation for the preceding image starts]: Gonorrhoea with cervicitis and vaginal dischargeCDC Image Library [Citation ends].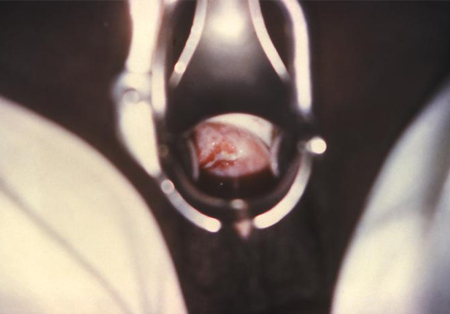
Urethral discharge
Discharge may range from clear and mucoid to frankly purulent. If discharge is present, it should be sent for Gram stain to check for PMNs and gram-negative intracellular diplococci. Gram stain is both sensitive and specific for establishing the presence or absence of urethritis and gonorrhoeal infection in symptomatic patients. Swabs should also be sent for culture and nucleic acid amplification testing (NAAT) for Neisseria gonorrhoeae and Chlamydia trachomatis (and Mycoplasma genitalium if available).
If no discharge is obvious, the urethra may be gently stripped (compressed) and samples sent as above. In men, with a gloved thumb placed on the ventral surface of the penis and the forefinger on the dorsum, a gentle pressure should be applied while moving the hand forward toward the meatus. In women, with the patient in the lithotomy position and a gloved finger inserted in the vaginal vault, a gentle pressure should be applied forward along the urethra. If no sample can be expressed, then a small swab should be inserted 2 cm into the urethra to obtain a specimen.[2][Figure caption and citation for the preceding image starts]: Gonorrhoea with penile meatal dischargeCDC Image Library / Susan Lindsley [Citation ends].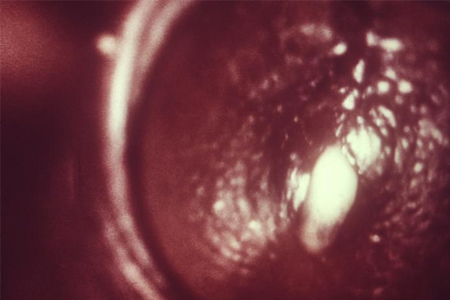 [Figure caption and citation for the preceding image starts]: Collection of a specimen from a male suspected of having gonorrhoea: the urethra is stripped towards the orifice to express some pus; a thin sterile swab is then inserted into the urethra and rotated before being withdrawnCDC Image Library / Renelle Woodall [Citation ends].
[Figure caption and citation for the preceding image starts]: Collection of a specimen from a male suspected of having gonorrhoea: the urethra is stripped towards the orifice to express some pus; a thin sterile swab is then inserted into the urethra and rotated before being withdrawnCDC Image Library / Renelle Woodall [Citation ends].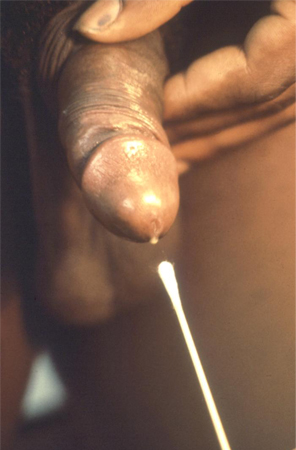
Tests
Gram stain of the urethral discharge is a rapid, sensitive, and specific test for establishing the presence or absence of gonorrhoeal infection. A positive staining or a result suggestive of gonococcal disease indicates that the patient should be treated for gonorrhoea and C trachomatis pending confirmatory test results, such as NAAT or culture.
Treatment for NGU is indicated whenever the result is negative for the presence of gonococci, but PMNs are present by microscopy (≥2 PMNs per field) or by urine leukocyte esterase. Testing with NAAT for N gonorrhoea, C trachomatis, and M genitalium should be done in people who meet the criteria for urethritis, even if initial Gram stain tests are negative for evidence of gonococci.[27][28] If the patient has been refractory to treatment, additional testing for Trichomonas vaginalis should be considered.[29][30]
A negative staining result for both gram-negative diplococci and PMNs indicates that a test for C trachomatis should be performed and/or Gram stain should be repeated before voiding. A first-void urine sample containing ≥10 PMNs per high power field suggests urethritis. Urine testing may be more sensitive than Gram stain in patients with very mild symptoms.[2]
Newer tests (known as non-culture tests), such as nucleic acid hybridisation tests and NAATs, are now available and are recommended as first-line methods of testing.[1][31][32] NAAT of urine specimens is preferable to culture in most settings because it has excellent sensitivity and is more convenient.
Culture of urethral discharge is used for sensitivity testing and genotyping, showing specificity close to 100% for diagnosing gonorrhoea, but sensitivity can vary between 85% and 95% (under optimal conditions).[33] While specificity of culture is very high for C trachomatis, culture methods are technically demanding and relatively insensitive, such that NAATs have replaced culture as the definitive diagnostic test for chlamydia.[34] Culture is not a reliable test for Mycoplasma species, as it is a slow-growing organism.[35]
Tests for T vaginalis are done if the patient is refractory to treatment. A NAAT for Trichomonas is available for diagnosis but may only be used at laboratories that have this test validated. Wet mount of urethral discharge is still considered as another method for of T vaginalis in women, but it is difficult to obtain in men. If wet mount is negative in women, a specimen should be sent for NAAT. In men, NAAT and culture of urine or urethral swab can be done (sensitivity 80%).[2] For women, vaginal swabs for NAAT or wet mounts can also be done. Potassium hydroxide prep can be useful to rule out candidal infection when candidal hyphae are present initially in the Gram stain, which may or may not indicate disease. Urinalysis (leukocyte esterase-positive in urethritis versus nitrite and leukocyte esterase-positive in urinary tract infection [UTI]) and culture (urine culture will be negative for enteric pathogens in urethritis) may rule out UTI if clinically unable to differentiate between urethritis and UTI.
NAATs for other organisms, such as Mycoplasma hominis, Ureaplasma urealyticum, and Ureaplasma parvum,are available but not all laboratories have them. These organisms may be suspected after initial treatment failure, if typical causative agents (N gonorrhoea, C trachomatis, M genitalium, T vaginalis) have been excluded.[36]
Patients should also routinely be tested for HIV and syphilis. [Figure caption and citation for the preceding image starts]: Gram stain of urethral exudate showing gram-negative diplococci and polymorphonuclear leukocytesAdapted from Public Health Image Library, CDC (Jacobs N, 1974) [Citation ends]. [Figure caption and citation for the preceding image starts]: McCoy cell monolayers with Chlamydia trachomatis inclusion bodiesAdapted from Public Health Image Library, CDC (Arum E and Jacobs N, 1975) [Citation ends].
[Figure caption and citation for the preceding image starts]: McCoy cell monolayers with Chlamydia trachomatis inclusion bodiesAdapted from Public Health Image Library, CDC (Arum E and Jacobs N, 1975) [Citation ends].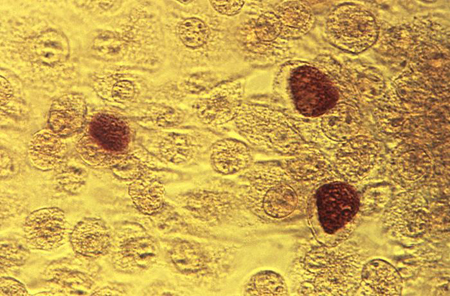
Use of this content is subject to our disclaimer