Differentials
Ocular ischaemic syndrome
SIGNS / SYMPTOMS
Commonly presents with amaurosis fugax and gradual or sudden visual loss.
Vision may be poor, intraocular pressure may be abnormally high or low, and anterior segment neovascularisation is a common feature.[75]
Commonly unilateral, predominantly haemorrhagic, and often involves equatorial and anterior retina rather than the posterior pole.[Figure caption and citation for the preceding image starts]: Ocular ischaemic syndrome: scattered posterior-pole and equatorial cluster haemorrhages (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
INVESTIGATIONS
Fluorescein angiography shows delayed arterial filling in affected eyes.
Doppler imaging may show carotid stenosis and ophthalmic artery flow reversal.
Radiation retinopathy
SIGNS / SYMPTOMS
Typically occurs in people with a history of radiation exposure and without diabetes.
Signs of an irregular pattern of capillary leakage and non-perfusion are present. [Figure caption and citation for the preceding image starts]: Radiation retinopathy: cotton wool spots (white arrow), optic disc oedema (white circle), venous beading (blue arrow), nerve fibre layer haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].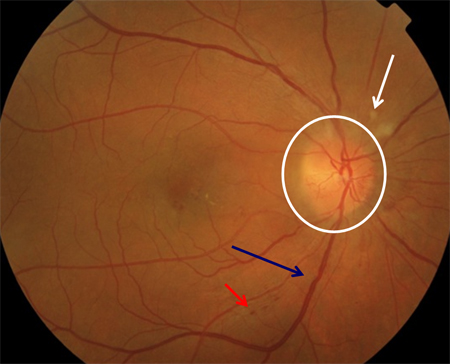
INVESTIGATIONS
No differentiating tests; exposure to radiation can usually be elicited from the history.
Retinal venous occlusion
SIGNS / SYMPTOMS
Typically produces acute visual loss in one eye, and retinal signs (i.e., haemorrhage, cotton wool spots, macular oedema, neovascularisation) are limited to the eye and to the territory of the occlusion.
Central retinal vein occlusion typically involves the posterior pole, but if a branch vein is occluded, signs are limited to the segment of retina drained by the vein, and it is usually possible to identify the point of occlusion where an artery crosses anterior to a vein. [Figure caption and citation for the preceding image starts]: Central retinal vein occlusion: optic disc swelling (white circle), macular oedema (yellow circle), exudate (yellow arrow), nerve fibre layer haemorrhage (blue arrow), venous engorgement and tortuosity (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].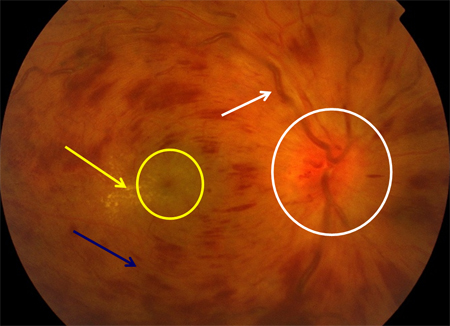 [Figure caption and citation for the preceding image starts]: Branch retinal vein occlusion: site of occlusion (white circle), cotton wool spot (white arrow), nerve fibre layer haemorrhage (red arrow), cluster haemorrhage (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Branch retinal vein occlusion: site of occlusion (white circle), cotton wool spot (white arrow), nerve fibre layer haemorrhage (red arrow), cluster haemorrhage (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].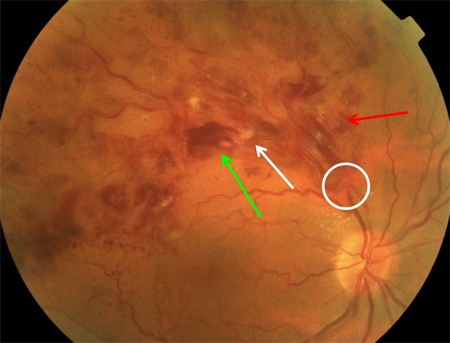
INVESTIGATIONS
No differentiating tests; typically monocular signs are the best indicator.
Fluorescein angiography is effective in characterising the distinctly localised nature of vascular abnormality in retinal venous occlusion.
Hypertensive retinopathy
SIGNS / SYMPTOMS
Systolic and diastolic pressures are markedly elevated.
Associated with acute visual disturbance, with optic disc swelling (which is uncommon in diabetic retinopathy) and macular oedema often in the form of a macular exudate star.
It may involve the posterior pole of both eyes, but signs of axoplasmic hold-up (i.e., cotton wool spots and optic disc oedema) tend to dominate the fundus appearance.
INVESTIGATIONS
Fluorescein angiography reveals arteriolar non-perfusion, rather than capillary non-perfusion as in diabetic retinopathy.
Proliferative sickle cell retinopathy
SIGNS / SYMPTOMS
Chronic infarction in sickle cell anaemia may be accompanied by vitreous haemorrhages and blindness due to neovascularisation.
Patients with sickle cell anaemia presenting with acute onset of floaters or acute loss of vision require an immediate evaluation by an ophthalmologist to check for signs of retinal haemorrhage or retinal artery occlusion.[76]
On examination, there may be severe vision loss, no afferent pupillary defect, possible cells in the anterior chamber, and blood in the vitreous humour with a poor view of the fundus.
Patients with sickle cell anaemia require yearly retinal examinations to screen for proliferative retinopathy. Around 45% of patients have maculopathy detectable with optical coherence tomography angiography; prevalence increases with age.[77]
INVESTIGATIONS
A sickle cell screen may detect the disease. However, it is unusual for a person with sickle cell disease to reach adulthood without being aware of their diagnosis. The diagnosis should be suspected in a patient who presents with unexplained haemolysis, with or without intermittent episodes of pain (vaso-occlusive crises). Patients may also present with avascular necrosis, retinal haemorrhage, or leg ulcers.
B-scan ultrasound may demonstrate the site of bleeding, and tractional retinal detachment.
Use of this content is subject to our disclaimer