Approach
Patients with diabetic retinopathy usually have diabetes diagnosed before their retinopathy is identified. It is believed that diabetes may have been present for some time before retinopathy develops.
History
Clinicians should identify risk factors for incidence and progression of retinopathy, including:[62][70]
Duration and type of diabetes
Glycaemic control
Hypertension
Dyslipidaemia
Pregnancy
Renal disease
Cardiovascular disease
Previous laser, injection, or ocular surgery
Medication history
Most patients are asymptomatic or have symptoms unrelated to retinopathy, such as fluctuation in vision with blood glucose levels. Visual disturbances may occur later in disease (e.g., floaters due to vitreous haemorrhage). Symptomatic patients may have either gradual vision loss (caused by macular oedema) or acute vision loss (caused by vitreous haemorrhage).
Clinical examination
Best corrected visual acuity should be measured. The anterior segment of the eye should be examined to exclude iris neovascularisation and cataract. Intraocular pressure should be measured. The pupil should be dilated, following which the fundus and peripheral retina should be examined by stereoscopic biomicroscopy using Volk or similar lenses.[62][70]
Clinical signs of non-proliferative diabetic retinopathy (NPDR) include:[62][70]
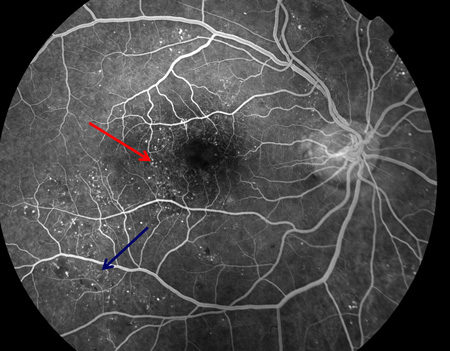
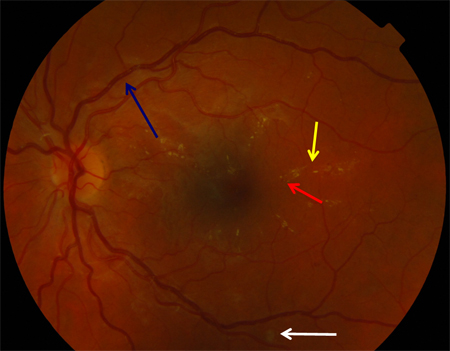
Microaneurysms[Figure caption and citation for the preceding image starts]: Fluorescein angiogram of non-proliferative diabetic retinopathy: microaneurysms (red arrow), intraretinal microvascular abnormalities (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
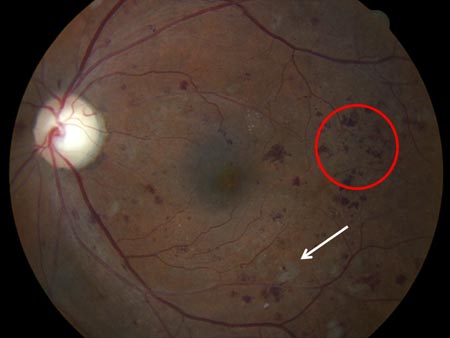
Cotton wool spots[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: cluster haemorrhages (red circle), cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
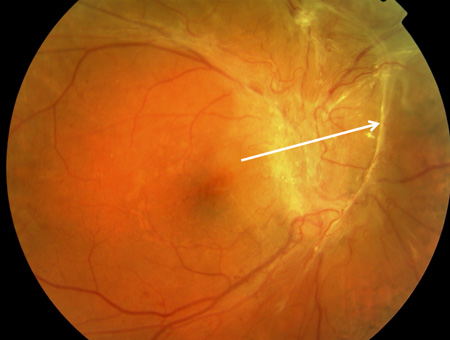
 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].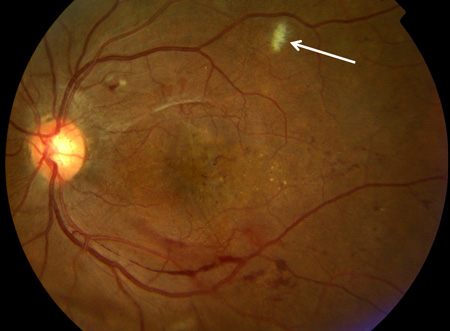
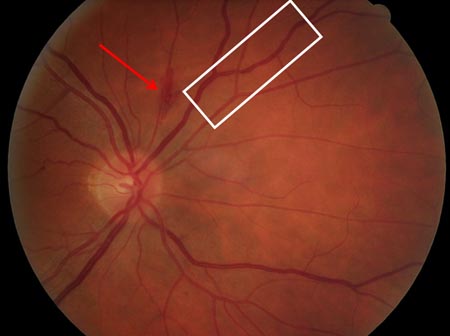
Intraretinal haemorrhage (presence of more than 20 in all 4 quadrants implies more severe retinopathy)[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: flame haemorrhage (red arrow), venous beading (white rectangle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
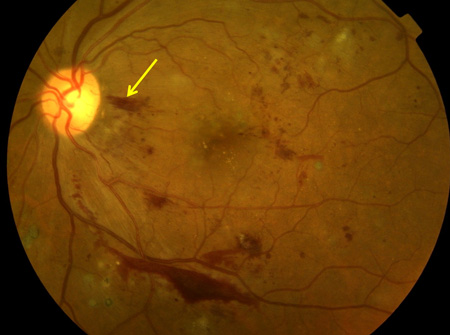
 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].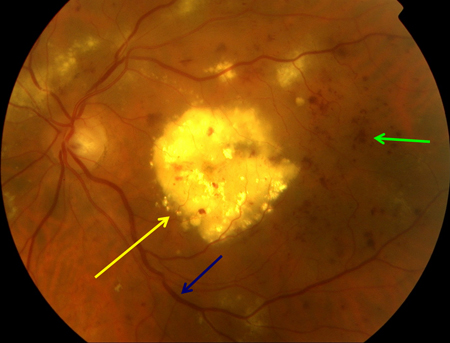 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: blot haemorrhage (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: blot haemorrhage (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
Venous beading (presence in 2 or more quadrants indicates more severe retinopathy)[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate (yellow arrow), microaneurysms (red arrow), venous dilatation (blue arrow), cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
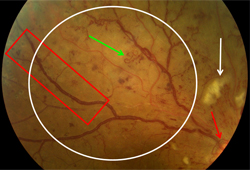
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].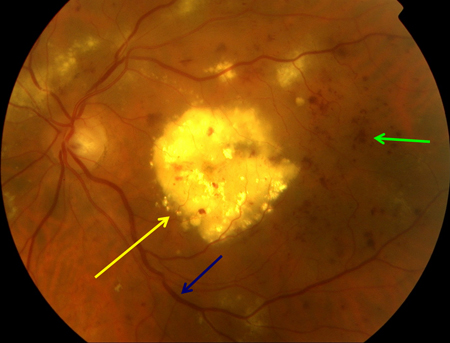 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].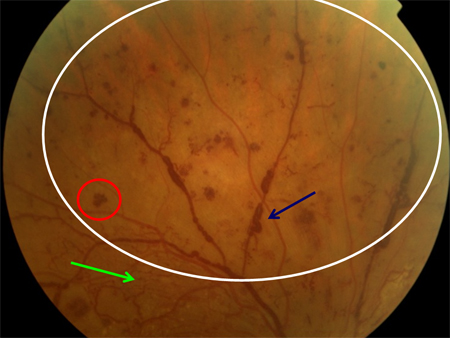 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].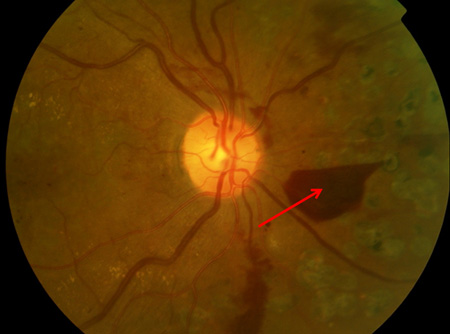
Intraretinal microvascular abnormalities (presence of any intraretinal microvascular abnormalities indicates more severe retinopathy).[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: optic disc new vessels (red arrow), intraretinal microvascular abnormality (IRMA; green arrow), cotton wool spot (white arrow), venous beading and segmentation (red rectangle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].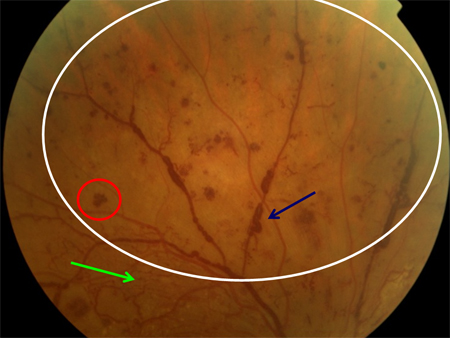
The 4-2-1 rule for severe non-proliferative diabetic retinopathy states:
4: more than 20 intraretinal haemorrhages in 4 quadrants
2: venous beading in 2 or more quadrants
1: intraretinal microvascular abnormalities in 1 or more quadrants.
Non-proliferative retinopathy may progress to proliferative diabetic retinopathy (PDR), characterised by:
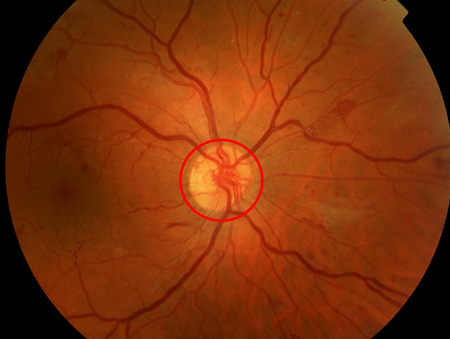
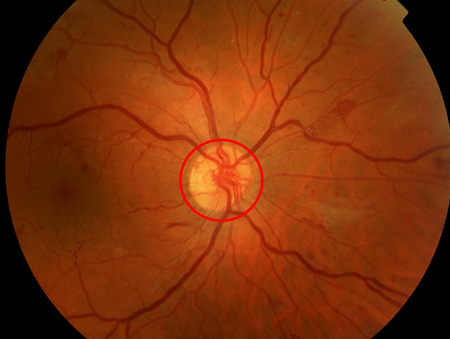
Optic disc neovascularisation[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle), retrohyaloid haemorrhage (red arrow), new vessels elsewhere with fibrosis (white arrow), dot and blot haemorrhage (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle), retrohyaloid haemorrhage (red arrow), new vessels elsewhere with fibrosis (white arrow), dot and blot haemorrhage (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].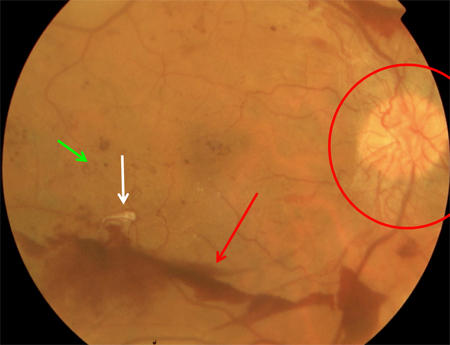 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: macular laser burns (black arrow), misty vitreous haemorrhage (blue arrow), clot within vitreous haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: macular laser burns (black arrow), misty vitreous haemorrhage (blue arrow), clot within vitreous haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].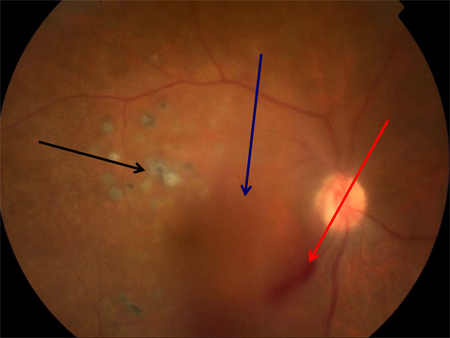 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: optic disc new vessels (red arrow), intraretinal microvascular abnormality (IRMA; green arrow), cotton wool spot (white arrow), venous beading and segmentation (red rectangle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: optic disc new vessels (red arrow), intraretinal microvascular abnormality (IRMA; green arrow), cotton wool spot (white arrow), venous beading and segmentation (red rectangle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].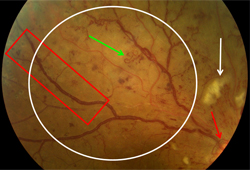 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].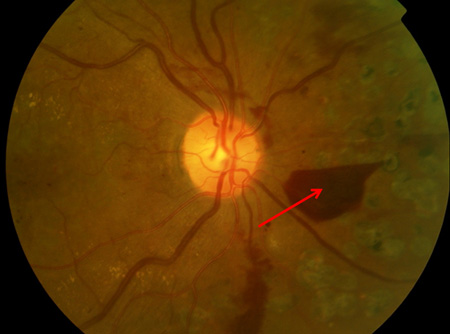
Retinal neovascularisation [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (red arrow), venous beading (blue arrow), intraretinal microvascular abnormality (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (red arrow), venous beading (blue arrow), intraretinal microvascular abnormality (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].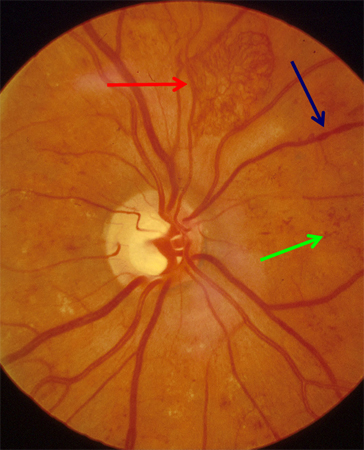 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].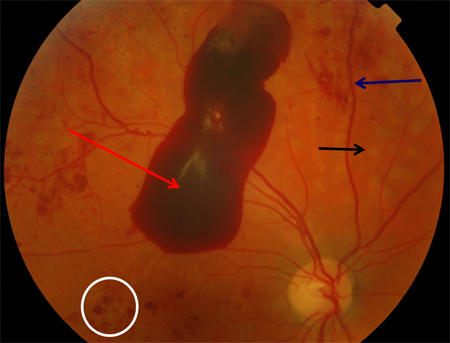 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction towards optic disc and consequent total retinal detachment (white block arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction towards optic disc and consequent total retinal detachment (white block arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].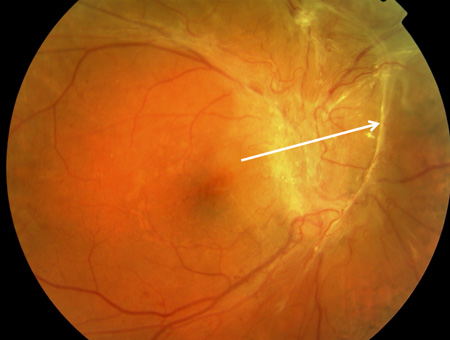
Preretinal or vitreous haemorrhage [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: nerve fibre layer haemorrhage (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].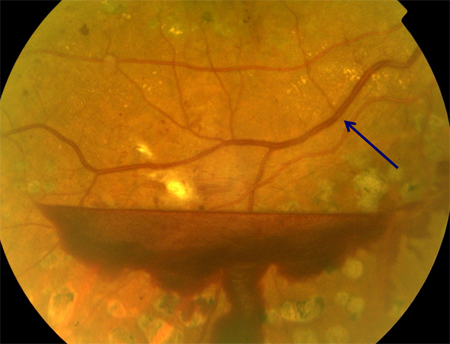 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: extensive vitreous haemorrhage obscuring most of fundus (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: extensive vitreous haemorrhage obscuring most of fundus (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].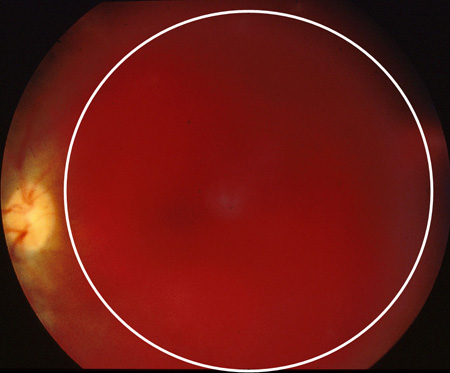 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].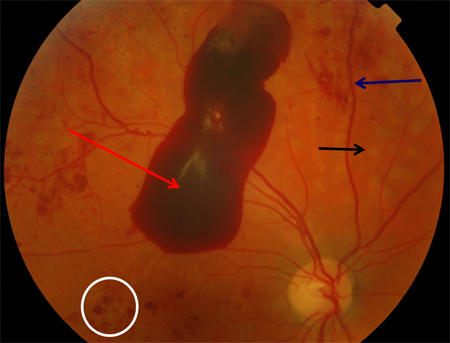 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (white arrow), vitreous (intra-gel) haemorrhage (green arrow), retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (white arrow), vitreous (intra-gel) haemorrhage (green arrow), retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].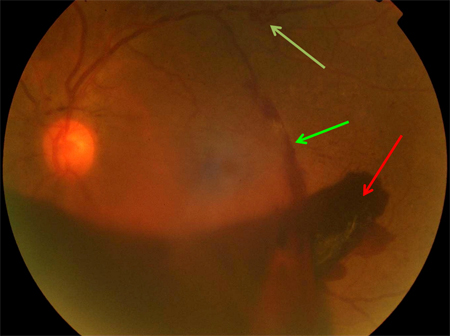
Retinal detachment. [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction towards optic disc and consequent total retinal detachment (white block arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction tear (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction tear (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].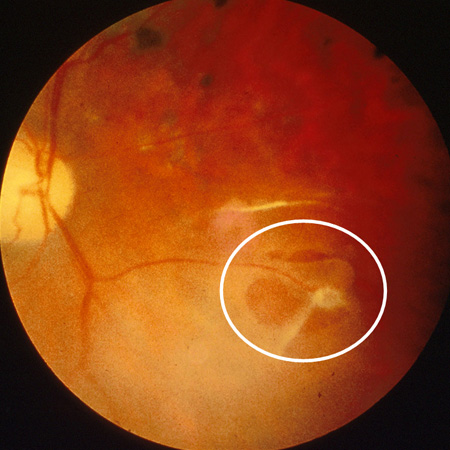
Eyes with untreated or inadequately treated proliferative retinopathy may progress to severe proliferative diabetic retinopathy with features such as traction retinal detachment and traction-rhegmatogenous retinal detachment.
Intraretinal oedema may involve the central retina, causing macular oedema, which appears as elevation or thickening of the central macula on stereoscopic evaluation. Macular oedema may occur in NPDR or PDR.[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate (yellow arrow), microaneurysms (red arrow), thickened retina (white circle), cystic change at macula (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].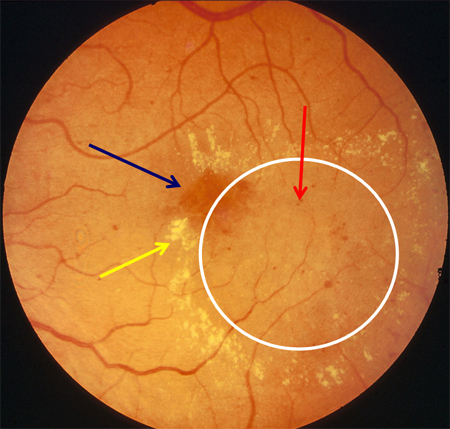 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: cotton wool spot (white arrow), thickened retina (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
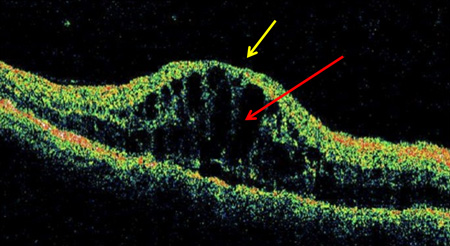
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: cotton wool spot (white arrow), thickened retina (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].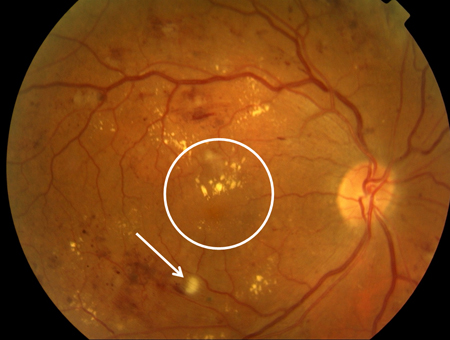 [Figure caption and citation for the preceding image starts]: Optical coherence tomography in macular oedema: loss of central foveal depression (yellow arrow), accumulation of fluid within cystoid spaces at fovea (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomography in macular oedema: loss of central foveal depression (yellow arrow), accumulation of fluid within cystoid spaces at fovea (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].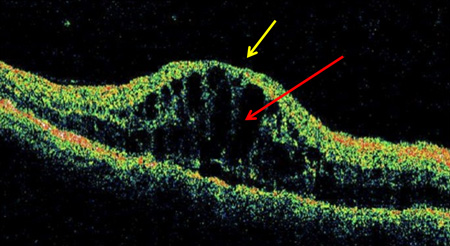 Both lipid exudates and/or microaneurysms may also indicate macular oedema.[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: thickened retina (white ellipse), exudate (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
Both lipid exudates and/or microaneurysms may also indicate macular oedema.[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: thickened retina (white ellipse), exudate (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].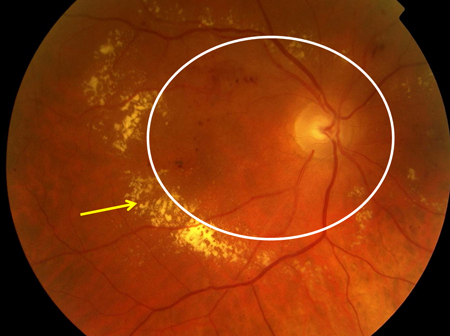
None of these signs is diagnostic for diabetic retinopathy, and all may occur in other conditions. However, diffuse bilateral posterior pole involvement with such signs in a patient with diabetes usually suggests diabetic retinopathy.
Ancillary tests
Other tests that may be used to confirm diagnosis include:[62][70]
Optical coherence tomography: should be ordered for all patients at baseline; for patients with exudation, haemorrhages, or microaneurysms in the macular area; and for patients with unexplained visual loss.[Figure caption and citation for the preceding image starts]: Optical coherence tomography in macular oedema: loss of central foveal depression (yellow arrow), accumulation of fluid within cystoid spaces at fovea (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Optical coherence tomogram of normal eye: normal foveal depression at centre of macula (yellow arrow), inner retina (towards centre of eye; red arrow), outer retina (further from centre of eye; blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomogram of normal eye: normal foveal depression at centre of macula (yellow arrow), inner retina (towards centre of eye; red arrow), outer retina (further from centre of eye; blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].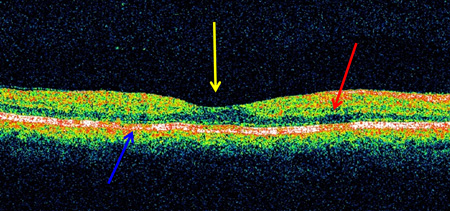 [Figure caption and citation for the preceding image starts]: Optical coherence tomography in vitreomacular traction: loss of foveal depression with traction on fovea (in direction of yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomography in vitreomacular traction: loss of foveal depression with traction on fovea (in direction of yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].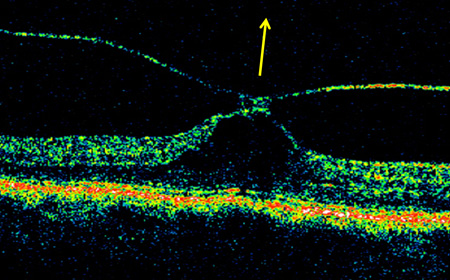
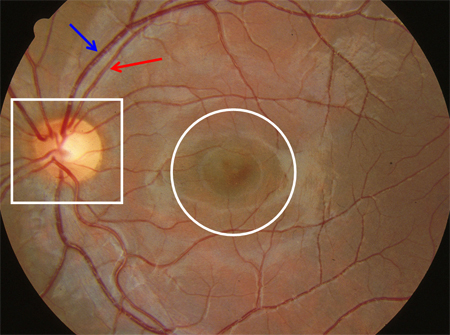
Digital photographs of the fundus: these should be ordered at baseline evaluation and when significant change is perceived in the fundus findings.[Figure caption and citation for the preceding image starts]: Normal retina left eye: optic disc (white square), macula (white circle), arteriole (red arrow), venule (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
Fluorescein angiography: this is indicated in some patients with diabetic maculopathy, and some patients with severe non-proliferative/proliferative retinopathy.[16][Figure caption and citation for the preceding image starts]: Fluorescein angiogram in mid-venous phase in diabetic retinopathy with microaneurysms only: microaneurysm (red arrow), optic disc (yellow arrow), macula (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
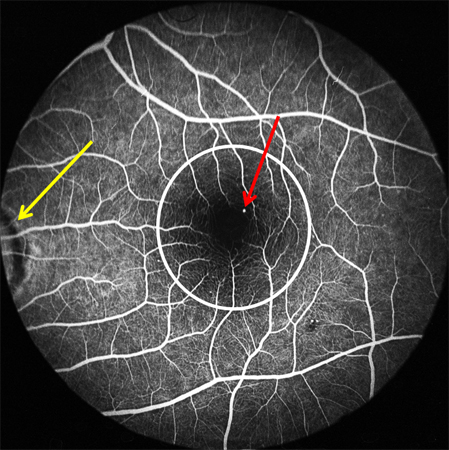 [Figure caption and citation for the preceding image starts]: Fluorescein angiogram of non-proliferative diabetic retinopathy: microaneurysms (red arrow), intraretinal microvascular abnormalities (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiogram of non-proliferative diabetic retinopathy: microaneurysms (red arrow), intraretinal microvascular abnormalities (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].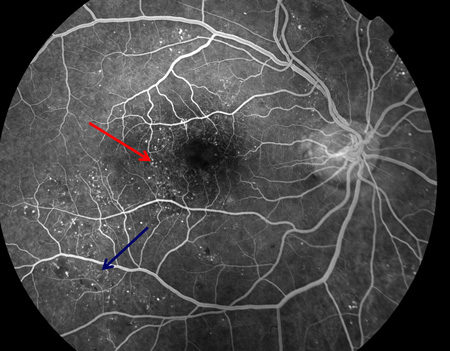 [Figure caption and citation for the preceding image starts]: Fluorescein angiogram in proliferative diabetic retinopathy with macular ischaemia: macular ischaemia (green circle), capillary non-perfusion (white arrow), optic disc new vessels (red arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiogram in proliferative diabetic retinopathy with macular ischaemia: macular ischaemia (green circle), capillary non-perfusion (white arrow), optic disc new vessels (red arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].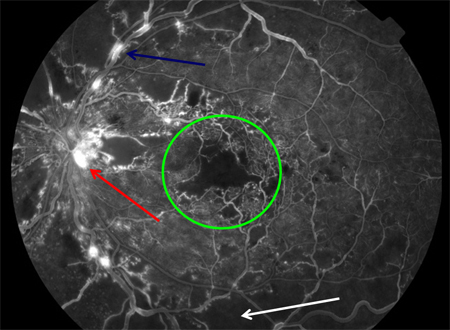 [Figure caption and citation for the preceding image starts]: Fluorescein angiography in proliferative diabetic retinopathy. Vascular component of fibrovascular proliferation (red arrows), capillary non-perfusion (yellow arrow), laser burns (green circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiography in proliferative diabetic retinopathy. Vascular component of fibrovascular proliferation (red arrows), capillary non-perfusion (yellow arrow), laser burns (green circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].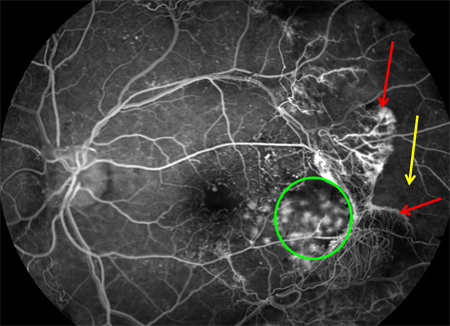 [Figure caption and citation for the preceding image starts]: Fluorescein angiogram in proliferative diabetic retinopathy: new vessels on the optic disc (red arrow), capillary non-perfusion (red rectangle), microaneurysms (green circle), venous beading (blue arrow), intraretinal microvascular abnormalities (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiogram in proliferative diabetic retinopathy: new vessels on the optic disc (red arrow), capillary non-perfusion (red rectangle), microaneurysms (green circle), venous beading (blue arrow), intraretinal microvascular abnormalities (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].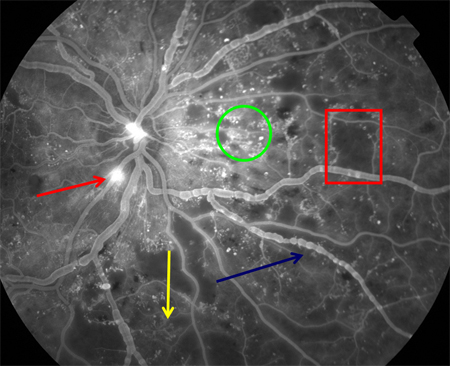 [Figure caption and citation for the preceding image starts]: Fluorescein angiography in proliferative diabetic retinopathy: new vessels elsewhere (red circle), capillary non-perfusion (white arrow), pan-retinal laser burns (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiography in proliferative diabetic retinopathy: new vessels elsewhere (red circle), capillary non-perfusion (white arrow), pan-retinal laser burns (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].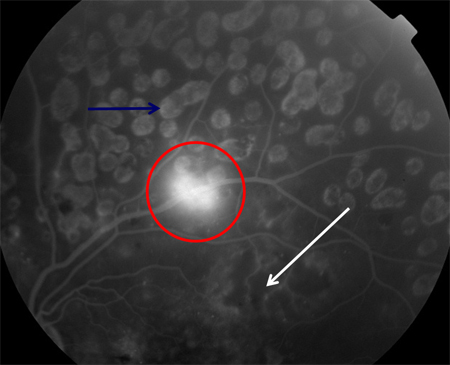
Optical coherence tomography angiography: this may be helpful in diagnosing macular ischaemia.[71][Figure caption and citation for the preceding image starts]: Optical coherence tomography in macular oedema: loss of central foveal depression (yellow arrow), accumulation of fluid within cystoid spaces at fovea (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
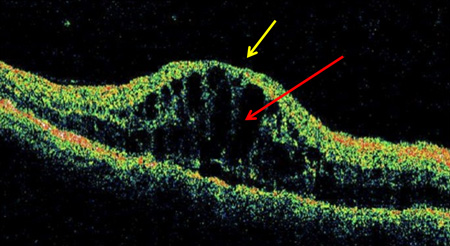 [Figure caption and citation for the preceding image starts]: Optical coherence tomogram of normal eye: normal foveal depression at centre of macula (yellow arrow), inner retina (towards centre of eye; red arrow), outer retina (further from centre of eye; blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomogram of normal eye: normal foveal depression at centre of macula (yellow arrow), inner retina (towards centre of eye; red arrow), outer retina (further from centre of eye; blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].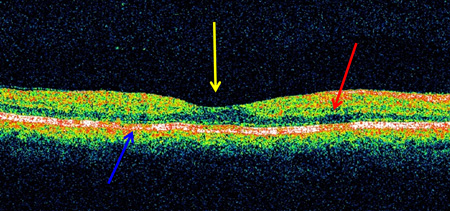 [Figure caption and citation for the preceding image starts]: Optical coherence tomography in vitreomacular traction: loss of foveal depression with traction on fovea (in direction of yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomography in vitreomacular traction: loss of foveal depression with traction on fovea (in direction of yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].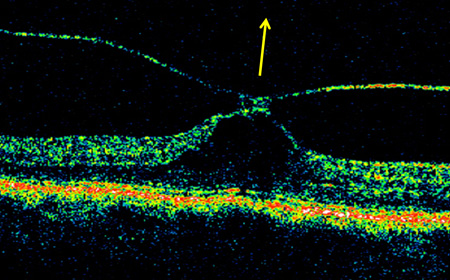
B-scan ultrasonography: this should be ordered in patients in whom media opacity (e.g., vitreous haemorrhage), prevents visualisation of the fundus.
Defining the severity of retinopathy and macular oedema
Using the retinal findings above and optical coherence tomography, the clinician can determine retinopathy severity and the presence or absence of macular oedema, and define the combined severity using the scales detailed in the Classification section under Aetiology.
Use of this content is subject to our disclaimer