Differentials
Common
Adhesions
History
history of abdominal or pelvic surgery; intermittent, cramp-like abdominal pain; nausea and/or vomiting, feculent vomiting, constipation, absence of flatus, history of intra-abdominal malignancy, including ovarian or colon cancer
Exam
high-pitched (hyperactive) bowel sounds with rushes, or absent bowel sounds; distended abdomen, tenderness to abdominal palpation, involuntary guarding; pyrexia; tachycardia; tympany on percussion; presence of abdominal scars
1st investigation
- CT of abdomen and pelvis with oral and intravenous contrast:
may see dilated loops of proximal bowel with collapsed loops posterior to site of obstruction
- plain abdominal x-rays:
may see dilated loops of bowel
More - chest x-ray:
may see free air under the diaphragm
More - ABG:
may be normal; metabolic acidosis; elevated lactate
More - FBC:
elevated WBC count; may be normal in early obstruction
More - serum electrolytes:
may not see any abnormalities with early obstruction; may confirm hypochloraemia and hypokalaemia; urea and creatinine may be elevated
More - CRP:
may be elevated
- serum lipase or amylase:
normal
More
Incarcerated/strangulated hernia
History
history of hernia, intermittent, cramp-like abdominal pain; painful bulge; nausea, vomiting, decreased or absent bowel function; absence of flatus; distended abdomen
Exam
high-pitched (hyperactive) bowel sounds with rushes, or absent bowel sounds; distended abdomen, tenderness to abdominal palpation; tender bulge in abdominal wall or inguinal/femoral region; involuntary guarding; or indirect hernia (more common on right than left)
1st investigation
- ABG:
may be normal; metabolic acidosis; elevated lactate
More - FBC:
may be normal in early obstruction; elevated WBC count as bowel infarction develops
More - serum electrolytes:
may be normal in early obstruction; may confirm hypochloraemia and hypokalaemia
More - CRP:
may be elevated
- serum lipase or amylase:
normal
More
Other investigations
Cholecystitis
History
history of cholelithiasis and biliary colic; intense right upper quadrant pain, lasting more than 30 minutes, exacerbated by eating (especially fatty foods); right shoulder pain (referred pain from the gallbladder may be felt in the right shoulder or interscapular region); fever, nausea, and/or vomiting; more common in women than men; risk factors include obesity, age over 50, pregnancy, use of oestrogen, history of liver disease, cirrhosis, and pancreatitis
Exam
fever, tachycardia, right upper quadrant tenderness, Murphy's sign (right upper quadrant tenderness with arrest of inhalation during palpation), palpable gallbladder, local guarding, and jaundice
1st investigation
Other investigations
- cholescintigraphy (hepatobiliary iminodiacetic acid [HIDA] scan):
no contrast filling in gallbladder; may see patent cystic duct
More - pregnancy test:
negative
More - CT or MRI of abdomen and pelvis:
may show irregular thickening of the gallbladder wall, poor contrast enhancement of the gallbladder wall (interrupted rim sign), increased density of fatty tissue around the gallbladder, gas in the gallbladder lumen or wall, membranous structures within the lumen (intraluminal flap or intraluminal membrane), peri‐gallbladder abscess
More
Perforated gastric ulcer
History
background of recurrent upper abdominal pain (dyspepsia); with nausea, vomiting, loss of appetite, and pain made worse by food; weight loss; use of non-steroidal anti-inflammatory drugs; sudden-onset severe upper abdominal pain with fever, nausea, vomiting, and peritoneal signs; referred pain to shoulders secondary to diaphragmatic irritation
Exam
often points to site of pain ('pointing sign'); develops into spreading upper abdominal pain; fever, peritoneal signs with guarding and rebound
1st investigation
- ABG:
may be normal; metabolic acidosis; elevated lactate
More - blood cultures:
may detect bacteraemia
More - FBC:
microcytic anaemia; elevated WBC count
More - serum electrolytes:
may show elevated creatinine and urea
More - CRP:
usually elevated
- serum lipase or amylase:
normal
More - CT of abdomen and pelvis:
pneumoperitoneum
More - plain abdominal x-rays:
abdominal free air on erect abdominal film
More - chest x-ray:
may see free air under the diaphragm
More - Helicobacter pylori testing:
positive result if H pyloripresent
More
Other investigations
- upper gastrointestinal series with water-soluble contrast:
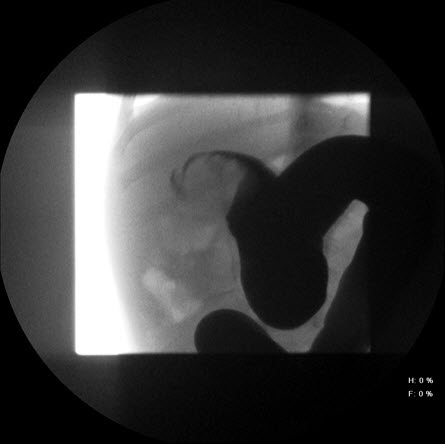
extravasation of contrast from stomach
- oesophagogastroduodenoscopy with biopsy:
may show Helicobacter pylori on culture and/or malignancy on histology
More - fasting serum gastrin level:
hypergastrinaemia in Zollinger-Ellison syndrome
- pregnancy test:
negative
More
Appendicitis
History
sudden-onset, constant, severe abdominal pain often periumbilical with migration to right lower quadrant, usually worse on movement; nausea, vomiting, anorexia, fever, diarrhoea, more common in children and young adults; pain may improve after appendix rupture
Exam
fever, tachycardia, patient may be lying in right lateral decubitus position with hips flexed; no or decreased bowel sounds; pain commonly originates near the umbilicus or the epigastrium; right lower quadrant (McBurney's point) tenderness with rigid abdomen; guarding and rebound tenderness; Rovsing's sign (palpation of left lower quadrant elicits pain in the right lower quadrant), psoas sign (right lower quadrant pain with right thigh extension), pain reproduced by coughing or hopping
1st investigation
Other investigations
- pregnancy test:
negative
More - right lower quadrant ultrasound:
non-compressible appendix of ≥7 mm in anteroposterior diameter appendicolith; interruption of the continuity of the echogenic submucosa; peri-appendiceal fluid or mass
More - MRI abdomen:
findings may include diffuse or segmental enlargement of the pancreas with irregular contour and obliteration of the peri-pancreatic fat, necrosis, or pseudocysts
More
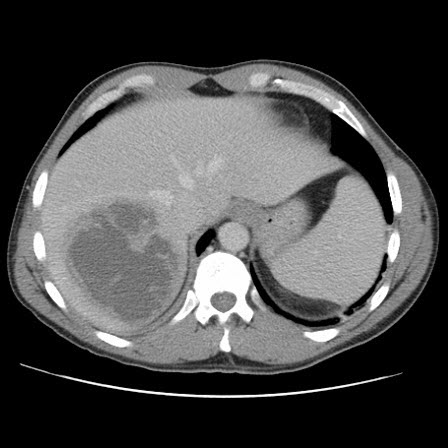
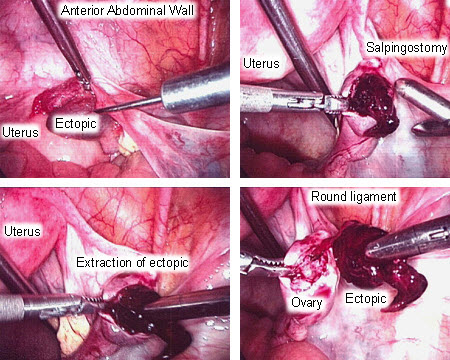
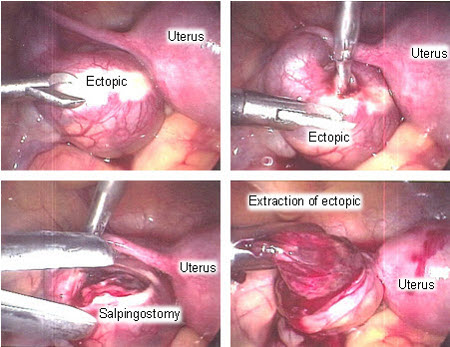
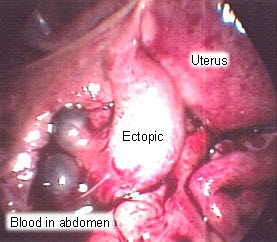
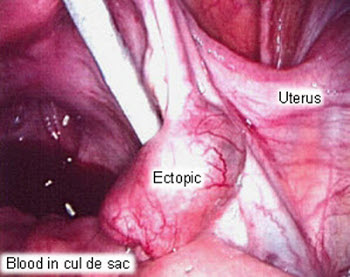
Ectopic pregnancy
History
vaginal bleeding with severe, usually unilateral pelvic pain; amenorrhoea or painless vaginal bleeding; history of recent early pregnancy or missed last menstrual period; risk factors include history of ectopic pregnancy, tubal surgery, pelvic inflammatory disease, infertility treatment and pregnancy with an intrauterine device in situ
Exam
may have palpable adnexal mass with or without tenderness; rigid abdomen, guarding, and rebound tenderness with ruptured ectopic leading to haemoperitoneum, tachycardia, and hypotension; vaginal bleeding on speculum examination
1st investigation
Other investigations
- diagnostic laparoscopy:
ectopic pregnancy or complex mass seen
More
Pelvic inflammatory disease
History
sexually active, young age at onset of sexual activity, unprotected sexual intercourse with multiple sexual partners; prior infection with chlamydia or gonorrhoea; history of pelvic inflammatory disease; use of intrauterine device; lower abdominal or pelvic pain of recent onset or relatively short duration that may have begun after intercourse; abnormal vaginal discharge; fever (non-specific, but suggestive)
Exam
abdominal tenderness; abnormal vaginal discharge; cervical motion tenderness and adnexal tenderness will be present; bimanual examination may reveal a tubo-ovarian abscess
1st investigation
Other investigations
- ultrasound:
tubal wall thickness >5 mm, incomplete septae within the tube, fluid in the cul-de-sac, and a cog-wheel appearance on the cross-section of the tubal view; may see complex adnexal mass, which could be indicative of a tubo-ovarian abscess
More
Acute pancreatitis
History
acute-onset, constant, severe mid-abdominal/epigastric pain that often radiates to the back; nausea, vomiting; anorexia; history of biliary colic, alcohol misuse, use of specific medicines (e.g., sulphonamides, tetracycline, oestrogens, corticosteroids), trauma, or surgery
Exam
varying degrees of abdominal tenderness, usually worse in the epigastric region; guarding, abdominal distension, and reduced or absent bowel sounds; ecchymoses in the skin of one or both flanks (Grey-Turner's sign) and/or the periumbilical area (Cullen's sign)
1st investigation
Other investigations
- serum calcium:
may be elevated
More - serum triglycerides:
may be elevated
More - abdominal ultrasound:
may see ascites, gallstones, dilated common bile duct, and enlarged pancreas
More - CT scan of abdomen with oral and intravenous contrast:
may show pancreatic inflammation, peri-pancreatic stranding, calcifications, or fluid collections; confirms or excludes gallstones
More - magnetic resonance cholangiopancreatography (MRCP):
findings may include stones, diffuse or segmental enlargement of the pancreas with irregular contour and obliteration of the peri-pancreatic fat, necrosis, or pseudocysts
More - pregnancy test:
negative
More
Acute diverticulitis
History
persistent left lower quadrant pain; fever, anorexia, nausea, vomiting, and abdominal distension (with ileus), patient may have a known history of diverticulosis
Exam
fever; left lower quadrant tenderness; frank blood in stool; diffuse tenderness with peritoneal signs (guarding, rebound tenderness, rigid abdomen) with perforation or ruptured abscess
1st investigation
- FBC:
elevated WBC count
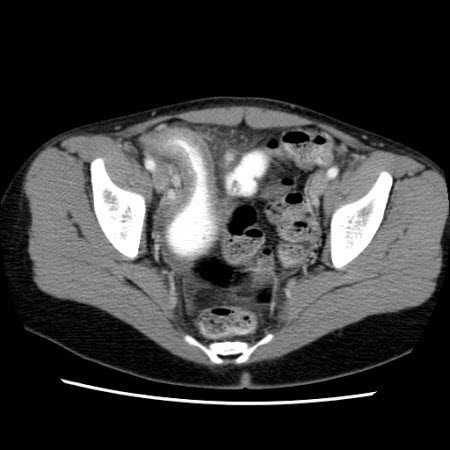
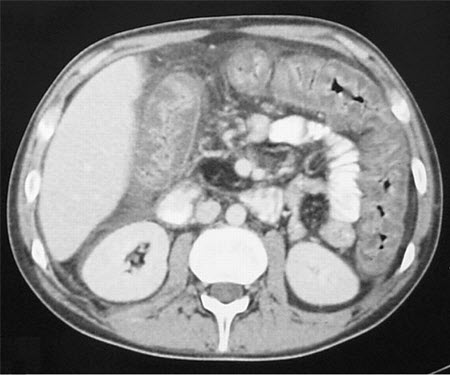
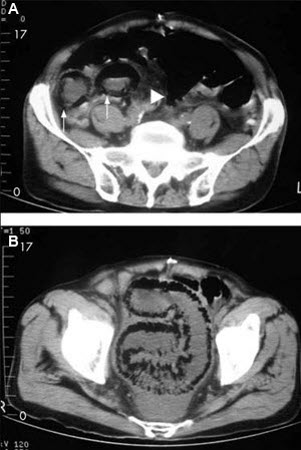
- CT abdomen/pelvis with intravenous, oral, and rectal contrast:
may see diverticula, inflammation of pericolonic fat, thickening of the bowel wall, free abdominal air, and an abscess
More
Other investigations
- water-soluble contrast enema:
may see diverticula along with extravasation of contrast material into an abscess cavity or into the peritoneum
More - abdominal ultrasound:
may see fluid collections around the colon or a thickened hypoechoic bowel wall
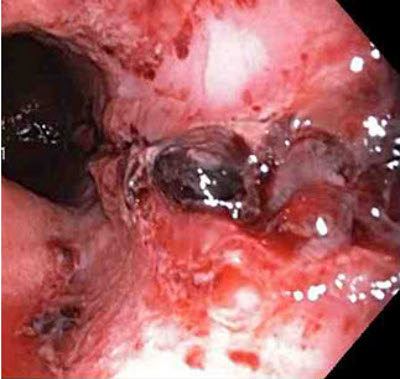
More - endoscopy:
may see inflamed diverticulum, abscess and perforation
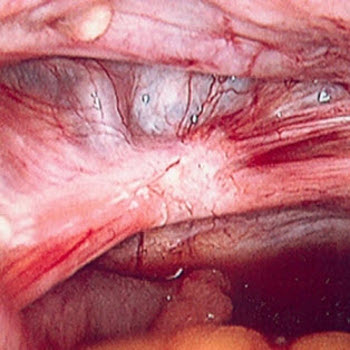
More - laparoscopy:
allows direct visualisation of bowel if diagnosis is unclear
- pregnancy test:
negative
More
Ulcerative colitis
History
bloody mucous diarrhoea and/or frank blood; fever, abdominal pain, weight loss, and growth retardation; back and joint pain and stiffness
Exam
abdominal tenderness; fevers; skin rash; episcleritis; pallor; guaiac-positive stools or frank blood on rectal examination
1st investigation
- FBC:
variable degree of anaemia, leukocytosis, or thrombocytosis
- comprehensive metabolic panel (including LFTs):
hypokalaemic metabolic acidosis; elevated sodium and urea; elevated alkaline phosphatase, bilirubin, aspartate aminotransferase, and alanine aminotransferase; hypoalbuminaemia
- CRP and erythrocyte sedimentation rate:
elevated
- stool studies:
negative culture, Clostridium difficile toxins A and B negative; WBCs present; elevated faecal calprotectin
- plain abdominal radiograph:
dilated loops with air-fluid level secondary to ileus; free air is consistent with perforation; in toxic megacolon, the transverse colon is dilated to ≥6 cm in diameter
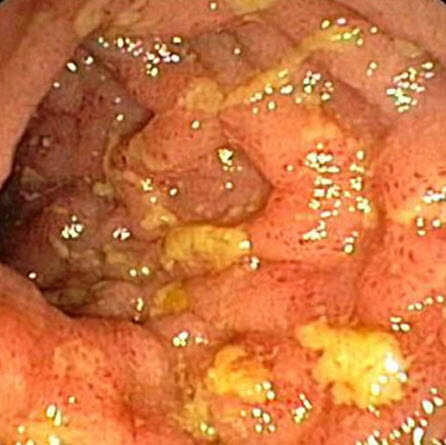
- colonoscopy/sigmoidoscopy:
rectal involvement, continuous uniform involvement, loss of vascular marking, diffuse erythema, mucosal granularity, fistulas (rarely seen), normal terminal ileum (or mild 'backwash' ileitis in pancolitis)
- biopsies:
continuous distal disease, mucin depletion, basal plasmacytosis, diffuse mucosal atrophy, absence of granulomata, and anal sparing; only mucosal/submucosal involvement
Other investigations
- double-contrast barium enema:
results range from a fine granular appearance of the bowel wall to diffuse ulceration, thumbprinting (due to mucosal oedema), and narrowing and shortening of the bowel, depending on the severity of the disease
- serological markers: perinuclear antineutrophil cytoplasmic antibody (pANCA):
may be positive
More - CT abdomen/pelvis with oral and intravenous contrast:
may show thickening, inflammation, abscess, fistulisation, obstruction of the bowel; biliary dilation suggests primary sclerosing cholangitis
More - radionuclide studies:
positive areas of inflammation
- pregnancy test:
negative
More
Crohn's disease
History
family history of Crohn's disease; typical age range 15-40 or 60-80 years; fevers, abdominal pain, prolonged intermittent bloody or non-bloody diarrhoea; fatigue; anal discharge and abscess; weight loss; faltering growth in children
Exam
abdominal tenderness often periumbilical or right lower quadrant if terminal ileum inflamed, mimicking appendicitis; peri-anal disease with fissures, skin tags fistulae, sinuses, and abscesses; aphthous ulcers; blood on rectal examination
1st investigation
- FBC:
anaemia; leukocytosis; may be thrombocytosis
- comprehensive metabolic panel:
hypoalbuminaemia, hypocholesterolaemia, hypocalcaemia
- CRP and erythrocyte sedimentation rate:
elevated
- iron studies:
normal, or may demonstrate changes consistent with iron deficiency
More - serum vitamin B12:
may be normal or low
- serum folate:
may be normal or low
- stool testing:
absence of infectious elements seen on microscopy or culture; faecal calprotectin may be elevated
- plain abdominal films:
small bowel or colonic dilation; calcification; sacroiliitis; intra-abdominal abscesses
- CT abdomen:
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulae
More - Yersinia enterocolitica serology:
negative
More
Other investigations
- MRI abdomen/pelvis:
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulae
More - abdominal and pelvic ultrasonography:
bowel wall thickening, surrounding inflammation, abscess; tubo-ovarian abscess
- colonoscopy:
aphthous ulcers, hyperaemia, oedema, cobblestoning, skip lesions
More - tissue biopsy:
mucosal bowel biopsies demonstrate transmural involvement with non-caseating granulomas
- technetium-99 labelled WBC scanning:
increased uptake in the inflamed segments
More - oesophagogastroduodenoscopy:
aphthous ulcers; mucosal inflammation
- wireless capsule endoscopy:
aphthous ulcers; hyperaemia; oedema; cobblestoning; skip lesions
More - anti-glycan antibodies:
positive anti-Saccharomyces cerevisiae mannan antibodies (ASCA) and negative perinuclear neutrophil cytoplasmic antibodies
More - pregnancy test:
negative
More
Cholelithiasis
History
right upper quadrant or epigastric pain (lasting more than 30 minutes) sometimes associated with food
Exam
right upper quadrant or epigastric tenderness; jaundice
1st investigation
Other investigations
- endoscopic retrograde cholangiopancreatography (ERCP):
ERCP demonstrates stones in the gallbladder or bile duct
More - magnetic resonance cholangiopancreatography (MRCP):
MRCP demonstrates stones in the gallbladder or bile duct
More - endoscopic ultrasound (EUS):
stones in gallbladder or bile duct
More - pregnancy test:
negative
More
Gastrointestinal malignancy
History
nausea, vomiting, abdominal pain and distension (especially with distal obstruction); little or no flatus or bowel function; weight loss; black stools
Exam
may have palpable mass, pallor, or cachexia; if obstruction present, distended abdomen, high-pitched (hyperactive) bowel sounds with rushes, or absent bowel sounds; tenderness to abdominal palpation, involuntary guarding; tachycardia
1st investigation
- FBC:
variable level of anaemia
- quantitative faecal immunochemical testing:
positive
More - renal function:
normal, except if advanced pelvic disease is compressing ureters
- LFTs:
normal, except if liver metastases present
- chest x-ray:
normal or evidence of metastatic disease
- oesophagogastroduodenoscopy with biopsy:
may show upper gastrointestinal ulcer, mass, or mucosal changes and provide histological confirmation
- colonoscopy with biopsy:
ulcerating exophytic mucosal lesion that may narrow the bowel lumen; histological confirmation
- CT thorax/abdomen/pelvis with oral and intravenous contrast:
hypodense lesions around tumour site or at distant metastatic sites (e.g. liver); colonic wall thickening, enlarged lymph nodes, liver metastases, ascites, lung secondaries; invasion of mesorectal fascia
- CT colonography:
appearances similar to conventional colonoscopy, with an ulcerating exophytic mucosal lesion that may narrow the bowel lumen
Other investigations
- upper gastrointestinal endoscopic ultrasound:
determines clinical tumour (T) and node (N) stage of upper gastrointestinal tumours
- transrectal endoscopic ultrasound:
determines clinical tumour (T) and node (N) stage of rectal tumours
- carcinoembryonic antigen:
elevated in colorectal cancer
- pregnancy test:
negative
More
Mallory-Weiss tear
History
vomiting or coughing with subsequent haematemesis; retrosternal, epigastric, or back pain; melena; presyncope/syncope; dysphagia, odynophagia
Exam
postural/orthostatic hypotension; pallor, tachycardia
1st investigation
- erect chest x-ray:
may show free air
- oesophagogastroduodenoscopy:
bleeding, adherent clot, or fibrous rind over an area of mucosal split at or near the gastro-oesophageal junction
More
Other investigations
Diabetic ketoacidosis
History
inadequate or inappropriate insulin therapy, infection (pneumonia and urinary tract infections are the most common), myocardial infarction; anorexia, nausea, vomiting, polyuria, thirst; abdominal pain; fever; dizziness, weakness, mental status change
Exam
acetone breath; deep, laboured, gasping breathing (Kussmaul's breathing); signs of hypovolaemia (tachycardia, hypotension, poor capillary refill, sunken eyes); abdominal tenderness; altered mental status
1st investigation
- plasma glucose:
elevated
- serum electrolytes and urea:
usually sodium low, potassium elevated, chloride low, magnesium low, calcium low, phosphate normal or elevated, urea elevated, creatinine elevated
- arterial blood gases:
pH varies from 7.00 to 7.30 in diabetic ketoacidosis (DKA); arterial bicarbonate ranges from <10 mmol/L (<10 mEq/L) in severe DKA to >15 mmol/L (>15 mEq/L) in mild DKA
- urinalysis:
positive for glucose and ketones; positive for leukocytes and nitrites in the presence of infection
- serum ketones:
elevated
- FBC:
elevated WBC count
More
Other investigations
Opioid withdrawal
History
history of drug use/misuse; fever, chills, nausea, vomiting; crampy abdominal pain; change of bowel habit; sweating, tremors, confusion, agitation, anxiety, muscular aches, increased salivation, dilated pupils
Exam
diffuse abdominal pain and tenderness; abdomen usually not distended; dilated pupils, confusion, sweating, copious salivation
Other investigations
- CT abdomen/pelvis:
may indicate intra-abdominal source
- pregnancy test:
negative
More
Gastroenteritis
History
nausea, vomiting, diarrhoea, crampy abdominal pain; history of sick contacts with similar symptoms; ingestion of questionable food or water; recent travel to places with insanitary conditions
Exam
dehydration; tachycardia; soft, non-distended abdomen; diffuse abdominal tenderness
1st investigation
- FBC:
elevated WBC count
- serum electrolytes and urea:
variable, may show dehydration
- stool for culture, ova and parasites:
may identify infectious agent
More
Infectious colitis
History
fever, chills, nausea, vomiting, diarrhoea (may be bloody), abdominal pain; abdominal distention, malaise, and anorexia; may have been recent travel, community outbreak or close contact with people with similar symptoms, recent use of antibiotics or hospitalisation; immunocompromise
Exam
pyrexia, abdominal pain and tenderness; variable signs from mild dehydration to hypovolaemic shock/septic shock (hypotension, tachycardia); peritonitis; possible abdominal distention
1st investigation
- FBC:
elevated WBC count and/or anaemia
- serum electrolytes and urea:
variable, may show dehydration
- stool culture:
may identify infectious agent
Other investigations
- stool immunoassay for Clostridioides difficile toxins A and B:
may be positive
More - stool culture for ova/parasites:
may be positive
More - cytomegalovirus antigen/shell assay:
may be positive
More - abdominal x-ray:
may show distended colon
- CT abdomen/pelvis with contrast:
may show thickened and inflamed segments of colon or all of colon affected; may show pneumatosis or localised perforation or perforation with phlegmon/abscess in severe cases
More - pregnancy test:
negative
More
Sickle cell crisis
History
history of sickle cell anaemia; diffuse bodily pain which can include abdominal pain, bone pain, chest pain; may also have fatigue, fever, jaundice, tachycardia, delayed growth and puberty; skin ulcers
Exam
diffuse acute abdominal pain and tenderness on palpation; patient is uncomfortable in any position; abdomen is usually not distended; fever
1st investigation
- FBC with reticulocyte count:
some degree of anaemia occurs in most patients with sickle cell disease; leukocytosis common in acute pain crises
- peripheral blood smear:
presence of nucleated red blood cells, sickle-shaped cells, and Howell-Jolly bodies
- urea and creatinine:
normal or elevated
More - LFTs:
variable
More - bacterial cultures:
pathogen detected
More - abdominal ultrasound:
may show enlarged spleen or presence of gallstones; hepatomegaly
More - CT abdomen/pelvis:
may show enlarged spleen or presence of gallstones; hepatic or renal infarction
More
Endometriosis
History
dysmenorrhoea; cyclical lower abdominal/pelvic/back pain, often 1-2 weeks before menstruation and during menstruation; pain during bowel movements; dyspareunia; sub-fertility; urinary or bowel obstruction; depression
Exam
discomfort and uterosacral ligament nodularity during bimanual/rectovaginal examination; tenderness on palpation in lower abdomen; fixed retroverted uterus in late stages; pelvic mass (ovarian endometriomas)
1st investigation
- transvaginal ultrasound:
may show ovarian endometrioma (homogeneous, low-level echoes) or evidence of deep pelvic endometriosis such as uterosacral ligament involvement (hypoechoic linear thickening)
More
Other investigations
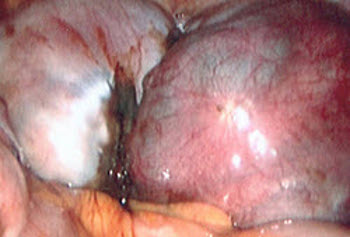
- diagnostic laparoscopy:
direct visualisation of endometrial implants and histological confirmation of biopsies
More - rectal endoscopic ultrasound:
hypoechoic nodule or mass
More - MRI pelvis:
hypointense, irregular thickening or mass of uterosacral ligament; replacement of fat tissue plane between uterus and rectum/sigmoid with tissue mass
More - pregnancy test:
negative
More
Testicular torsion
History
history of previous on-off testicular pain; sudden-onset testicular pain with nausea and vomiting; scrotal oedema/swelling/erythema; abdominal pain also often present
Exam
severe testicular pain and tenderness on affected side; may be swollen; affected testicle is located higher than the non-affected testicle, often in horizontal position; reduced or absent cremasteric reflex
1st investigation
Other investigations
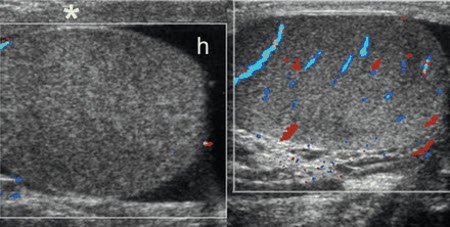
- power Doppler ultrasound:
absent or decreased blood flow in the affected testicle; decreased flow velocity in the intratesticular arteries, increased resistive indices in the intratesticular arteries
- colour Doppler ultrasound:
absent or decreased blood flow in the affected testicle; decreased flow velocity in the intratesticular arteries, increased resistive indices in the intratesticular arteries
More - spectral Doppler:
non-homogeneous and/or asymmetric vascular perfusion compared with the unaffected testis
- scintigraphy:
decreased uptake of radioactive technetium-99m to the affected testicle in patients with testicular torsion
More
Kidney stones
History
previous history of kidney stones; may be asymptomatic to severe abdominal flank pain radiating to the groin; other symptoms include nausea, vomiting, diaphoresis, haematuria; urinary frequency/urgency; occupations in hot conditions (e.g., chefs, steel workers); family history of stones
Exam
often obese; abdomen soft; when in pain, may be severe, unable to find comfortable position; tender to palpation/percussion of costovertebral angle/flank; if urosepsis also present may be tachycardic, hypotensive, pyrexial
1st investigation
- urinalysis:
dipstick positive for leukocytes, nitrates, blood; microscopic analysis positive for WBCs, red blood cells, or bacteria; may be normal
More - FBC:
normal or raised WBC count
More - serum electrolytes, urea, and creatinine:
normal or deranged
More - uric acid level:
normal or elevated
More - non-contrast helical CT abdomen/pelvis (stone protocol):
calcification seen in renal collecting system or ureter
Other investigations
- renal ultrasound:
calcification seen within urinary tract
- retrograde urethrogram:
calcification seen within urinary tract or a filling defect seen
- intravenous pyelogram:
calcification seen within urinary tract or a filling defect seen when dye is passing through the kidney and down the ureter
More - pregnancy test:
negative
More
Pyelonephritis
History
family history of kidney stones; history of urinary tract infection, stress incontinence, or frequent sexual intercourse; fever with chills; dysuria, frequency, urgency; flank pain; nausea, vomiting, diaphoresis, haematuria
Exam
pyrexia; flushed looking; flank pain and/or costovertebral angle tenderness on palpation/percussion
1st investigation
- urinalysis:
pyuria (>10 WBCs per high-power field [HPF]), red blood cells ≥5/HPF, leukocyte esterase, nitrites, WBC casts, proteinuria up to 20 g/L (2 g/dL)
- Gram stain:
typically gram-negative rods; less typically gram-positive cocci
- urine culture:
positive
- FBC:
leukocytosis
- CRP:
elevated
More
Other investigations
- blood cultures:
may be positive
More - CT abdomen/pelvis with intravenous contrast:
altered renal parenchymal perfusion; altered excretion of contrast; perinephric fluid; non-renal disease; may show abscess formation
More - renal ultrasound:
gross structural abnormalities; hydronephrosis; stones; perirenal fluid collections
More - 99mTc-dimercaptosuccinic acid scintigraphy:
inflammation or scarring of the renal cortex; unequal distribution of renal function between the kidneys
More - MRI:
structural anomalies of the genitourinary system (prenatal); renal inflammation or masses; abnormal renal vasculature; urinary obstruction
More - pregnancy test:
negative
More
Uncommon
Volvulus
History
steady abdominal pain that may have colicky characteristics varying from vague discomfort to excruciating (severe unremitting pain suggests gangrenous bowel); history of abdominal surgery, abdominal or inguinal hernia; nausea, vomiting, emesis may be absent in patients with sigmoid volvulus (more common in older or debilitated patients); periumbilical or hypogastric pain, diarrhoea or constipation (depending on the degree and location of the obstruction)
Exam
often diffuse abdominal distension and tenderness; faint or no bowel sounds, rigid abdomen, guarding, rebound tenderness, fever, or haematochezia
1st investigation
- plain abdominal x-rays:
partial or complete obstruction; dilated bowel loops; air-fluid levels; abdominal free air with perforation
More - ABG:
may be normal; metabolic acidosis; elevated lactate
More - chest x-ray:
may see free air under the diaphragm
More - FBC:
elevated WBC count
More - serum electrolytes:
may be normal in early obstruction; may confirm hypochloraemia and hypokalaemia; urea and creatinine may be elevated
More - CRP:
may be elevated
Retroperitoneal haemorrhage
History
symptoms may be vague; groin, lower abdominal or back pain; history of risk factors (e.g., recent anticoagulation use, recent history of transfemoral catheterisation, recent obstetric procedure in women of childbearing age, malignancy, pelvic or spine fractures)
Exam
non-specific findings including unexplained tachycardia; diffuse abdominal, back, or lower quadrant abdominal pain, abdominal distension; may be bruising of flank; flank mass on palpation; diaphoresis if severe; profound hypotension with decreasing levels of consciousness if shock present
1st investigation
- basic test panel (FBC, serum electrolytes, blood glucose, serum LFTs, coagulation profile, group and save):
low Hb; INR may be raised
- ECG:
normal, or tachycardia
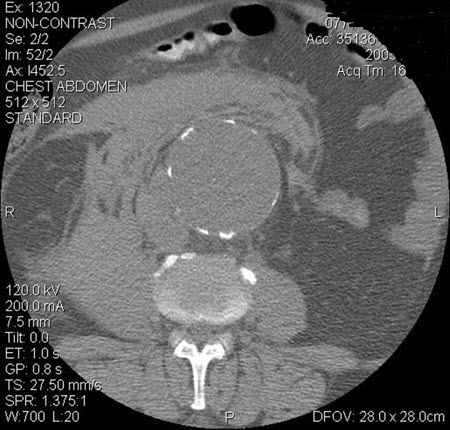
- CT abdomen and pelvis:
haematoma may be visualised
More - abdominal and pelvic CT angiography:
may demonstrate active bleeding site if bleeding is ongoing
More
Other investigations
Viral Hepatitis
History
perinatal exposure, family history of hepatitis B viral infection, blood transfusions, high-risk activities (e.g., multiple sexual partners, men who have sex with men, injection drug users, intravenous drug use); right upper quadrant pain; fever, chills, fatigue, myalgia/arthralgia; nausea, vomiting; jaundice
Exam
right upper quadrant tenderness; hepatosplenomegaly; jaundice; ascites; maculopapular or urticarial rash
1st investigation
Intussusception
History
more common in children than in adults; classic presentation of severe, colicky pain alternating with lethargy; may also present with vague abdominal complaints; severe, cramp-like abdominal pain; children may be inconsolable; vomiting
Exam
occult or frank blood mixed with mucus giving currant-jelly appearance, abdominal tenderness, and palpable mass
1st investigation
- ultrasound:
tubular mass in longitudinal view; target lesion in transverse view
More - air or water enema:
filling defect or cupping in the head of contrast as it advances to the site of the intussusception
More - FBC:
elevated WBC count
More - serum electrolytes:
may be normal in early obstruction; may confirm hypochloraemia and hypokalaemia; urea and creatinine may be elevated
More - CRP:
may be elevated
Other investigations
- CT of abdomen and pelvis:
target lesion: intraluminal soft-tissue density mass with an eccentrically placed fatty area; reniform mass: high attenuation peripherally and lower attenuation centrally; sausage-shaped mass: alternating areas of low and high attenuation representing closely spaced bowel wall, mesenteric fat, and/or intestinal fluid and gas
More
Perforated duodenal ulcer
History
acute onset of severe epigastric pain, nausea, vomiting, and loss of appetite; more common in men than women; history of melaena or bright red blood from rectum, episodic epigastric pain relieved by eating; use of non-steroidal anti-inflammatory drugs; may have latent period with symptom improvement that may last several hours, followed by peritonitis with fever, nausea, vomiting, and peritoneal signs; referred pain to shoulders secondary to diaphragmatic irritation
Exam
tachycardia, fever, epigastric tenderness, rigid abdomen, guarding, rebound tenderness, and occult or frank blood in stool
1st investigation
- ABG:
may be normal; metabolic acidosis; elevated lactate
More - blood cultures:
may detect bacteraemia
More - FBC:
elevated WBC count
More - serum electrolytes:
may show elevated creatinine and urea
More - CRP:
usually elevated
- serum lipase or amylase:
normal
More - CT of abdomen and pelvis:
pneumoperitoneum
More - plain abdominal x-rays:
abdominal free air on erect abdominal film
More - chest x-ray:
may see free air under the diaphragm
More - Helicobacter pylori testing:
positive result if H pylori present
More
Other investigations
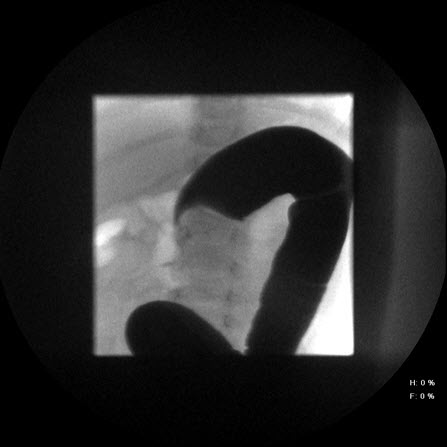
- upper gastrointestinal series with water-soluble contrast:
extravasation of contrast from stomach or duodenum
- esophagogastroduodenoscopy with biopsy:
visualisation of ulcer; histological confirmation
Ruptured ovarian cyst
History
often days 20 and 26 of a normal menstrual cycle; often follows intercourse, exercise, or pelvic examination; sudden-onset lower abdominal pain, may be lateralised to left or right; light vaginal bleeding; postural dizziness if marked haemorrhage (associated with rupture of corpus luteum cyst, specifically among patients on anticoagulants or with bleeding disorders)
Exam
light vaginal bleeding; vital signs usually normal, but may be low-grade fever; may have tachycardia/hypotension if severe bleeding in association with coagulopathy or anticoagulant use; signs of peritonitis if haemoperitoneum present
1st investigation
Other investigations
Ovarian torsion
History
sudden onset of unilateral pain, waxing and waning severe pelvic pain, and history of adnexal mass
Exam
severe, unilateral adnexal tenderness; adnexal mass that is often palpable and, in advanced cases, patient may develop rigid abdomen, guarding, and rebound tenderness
1st investigation
Other investigations
Abdominal aortic dissection
History
severe, sharp, or tearing pain in thorax or abdomen, pain radiates to neck or back, history of hypertension, increased risk in Marfan's syndrome and Ehlers-Danlos syndrome or other collagen vascular disorders, painless dissection is rare
Exam
hypertension in distal dissection; lower extremity pulse deficit, sensory or motor deficits (including numbness, tingling, or transient paraplegia); ischaemia and, if mesenteric arteries involved, bowel ischaemia with rigid abdomen, guarding and rebound tenderness
1st investigation
- serum urea and electrolytes:
elevated urea
More - plain abdominal x-rays:
aortic wall calcification consistent with abdominal aortic aneurysm; loss of psoas shadow in presence of rupture
More - CT angiography of chest and abdomen:
two aortic lumina separated by intimal flap or displaying different rates of contrast opacification
- magnetic resonance angiography of chest and abdomen:
two aortic lumina separated by intimal flap; branch vessel involvement; aortic regurgitation
More - chest x-ray:
widened aortic silhouette; widened mediastinum
More
Other investigations
- contrast aortography:
two aortic lumina separated by intimal flap; branch vessel involvement; aortic regurgitation
More
Ruptured aortic aneurysm
History
severe abdominal pain radiating to back, flank, groin, or legs; patient unaffected by position; history of aneurysm, possible discoloration and pain in lower extremities due to ischaemia
Exam
tachycardia, hypotension, pulsatile abdominal mass, nausea, vomiting, lower extremity pulse deficit, lower extremity or back pain, loss of consciousness or confusion, limb numbness or tingling, ischaemia and livedo reticularis
1st investigation
- abdominal ultrasound:
aortic aneurysm
More
Other investigations
- CT of chest and abdomen with intravenous contrast:
aortic aneurysm, extravasation of contrast
More
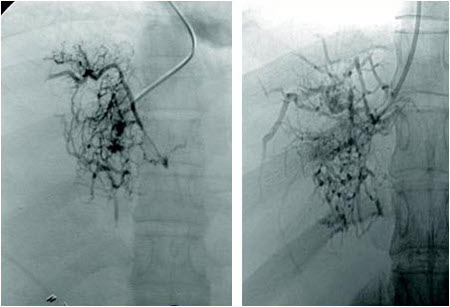
Acute mesenteric ischaemia (AMI) and infarction
History
age >50 years; constant periumbilical non-radiating abdominal pain; recent history of post-prandial abdominal pain; history of atrial fibrillation, coronary artery disease, myocardial infarction, and congestive heart failure; melaena or bright red blood from rectum, and patient taking vaso-active medicines; risk factors include smoking, hypertension, hyperlipidaemia, and diabetes
Exam
initially, pain out of proportion to examination findings with soft, non-tender abdomen despite severe abdominal pain, followed by rigid abdomen, guarding, and rebound tenderness with bowel necrosis and perforation, and, in advanced cases, fever, tachycardia, and hypotension will be present
1st investigation
- CT of abdomen:
vessel thrombosis; thickened bowel wall; abnormal bowel wall enhancement; pneumatosis; portal or mesenteric venous gas
More - plain abdominal x-rays:
may see dilated loops of bowel; air-fluid level; bowel wall thickening; formless loops of large or small bowel; pneumatosis; vascular gas
More - chest x-ray:
may see free air under the diaphragm
More - FBC:
elevated WBC count
More - serum lactate:
elevated
More - ABG:
metabolic acidosis
- serum electrolytes:
uraemia, elevated creatinine
Other investigations
- mesenteric angiography:
arterial or venous obstruction
More
Myocardial infarction
History
epigastric pain, diaphoresis, shortness of breath, nausea, vomiting; may be risk factors such as atherosclerosis, diabetes, smoking, hypertension, obesity, dyslipidaemia; atypical symptoms more common in women, older people, and those with diabetes
Exam
often normal; may be tachycardia, bradycardia, hypotension, third and fourth heart sound, paradoxical splitting of second heart sound
1st investigation
- ECG:
ST-T wave changes or ischaemic changes
- cardiac troponins:
>99th percentile of normal
Other investigations
Meckel's diverticulitis
History
sudden-onset severe abdominal pain, often starts periumbilical with migration to right lower quadrant; nausea, vomiting, anorexia, fever, diarrhoea
Exam
fever, tachycardia, patient may be lying in right lateral decubitus position with hips flexed; no or decreased bowel sounds; pain commonly originates near the umbilicus or the epigastrium; right lower quadrant (McBurney's point) tenderness with rigid abdomen; guarding and rebound tenderness; psoas sign (right lower quadrant pain with right thigh extension)
1st investigation
- FBC:
low haemoglobin and haematocrit; leukocytosis with left shift
- technetium-99m pertechnetate scan ('Meckel scan'):
ectopic focus or 'hot spot'; enhancement of diverticulum
Other investigations
- plain abdominal radiography:
dilated bowel loops with air-fluid levels and paucity of distal gas suggests bowel obstruction; free air on upright film suggests a perforation; a density in the right side of the abdomen suggests an intussusception
- CT scan of the abdomen and pelvis:
blind-ending fluid-filled and/or gas-filled structure in continuity with distal ileum
- ultrasound of the abdomen:
tubular mass in longitudinal views and a doughnut or target appearance in transverse views suggests intussusception
Hepatic abscess
History
biliary tract abnormalities; age >50 years; malignancy; diabetes mellitus; history of interventional biliary or hepatic procedures; travel to endemic area for amoebiasis; right upper quadrant pain, fever, chills, anorexia, and malaise; nausea and vomiting; cough, shortness of breath, may have had recent episode of gastrointestinal disease or biliary disease such as appendicitis, diverticulitis, or cholangitis
Exam
fever; hepatomegaly; weight loss; shortness of breath; jaundice; pleural effusion right lower zone; signs of shock with severe disease; rarely ascites
1st investigation
- FBC:
leukocytosis, elevated neutrophil count, anaemia
- LFTs:
elevated alkaline phosphatase, mildly elevated aminotransferases and bilirubin, hypoalbuminaemia
- blood culture:
pyogenic: may be positive for causative bacterial organism; fungal: may be positive for Candida species
- prothrombin time and activated partial thromboplastin time:
usually normal
- CRP:
may be elevated
- chest x-ray:
in presence of pleural effusion: blunting of the costophrenic angles
- liver ultrasound:
demonstrates a variably echoic lesion
- contrast-enhanced abdominal CT scan:
demonstrates hypodense liver lesions; gas within the lesion is highly suggestive of a pyogenic abscess
More - stool Entamoeba histolytica antigen detection test:
positive in amoebiasis
- Gram stain and culture of aspirated abscess fluid:
pyogenic: positive for causative bacterial organism; fungal: may be positive for Candida species
- polymerase chain reaction (PCR) or real-time quantitative PCR of aspirated abscess fluid:
amplification of amoebic DNA
Other investigations
- pregnancy test:
negative
More
Psoas abscess
History
fever, chills, nausea, vomiting, flank or low abdominal/groin pain, malaise; new-onset limp
Exam
mild pyrexia, rigors, flank or abdominal tenderness; hip flexion deformity; pain with active hip flexion and passive extension
1st investigation
- FBC:
elevated WBC count
- CRP:
elevated
- CT abdomen/pelvis with intravenous contrast:
visualisation of abscess
Other investigations
- ultrasound abdomen/pelvis:
visualisation of abscess
- MRI abdomen/pelvis:
visualisation of abscess
- aspiration of abscess, Gram stain and culture:
may culture causative organism
Tuberculosis
History
male, black or Hispanic ethnicity; diffuse abdominal pain, right lower quadrant pain
Exam
fever, cachexia, abdominal swelling, abdominal mass, hepatosplenomegaly, lymphadenopathy
1st investigation
- chest x-ray:
consolidation, pulmonary infiltrates, mediastinal or hilar lymphadenopathy, upper zone fibrosis
More - sputum acid-fast bacilli smear and culture:
presence of acid-fast bacilli (Ziehl-Neelsen stain) in specimen
More - acid-fast bacilli smear and culture of extrapulmonary biopsy specimen:
positive
More - nucleic acid amplification tests (NAAT):
positive for M tuberculosis
More
Other investigations
- lateral flow urine lipoarabinomannan (LF-LAM) assay:
positive
More
Oesophageal perforation (Boerhaave’s syndrome)
History
history of vomiting followed by chest pain; recent oesophagogastroduodenoscopy or chest/neck trauma; neck, chest, epigastric, or upper back pain; dysphagia; respiratory distress; fever, tachycardia
Exam
mediastinal crunching sound on auscultation; subcutaneous emphysema of neck or chest; decreased breath sounds (usually on left side); tachypnoea and respiratory distress
1st investigation
- FBC:
elevated WBC count
- erect chest x-ray:
may show pneumomediastinum, subcutaneous emphysema, pleural effusions typically located left side
Fitz-Hugh Curtis syndrome
History
female with history of pelvic inflammatory disease; severe right upper quadrant abdominal pain, possibly referred to right shoulder and worse on coughing, sneezing, or movement; fever, chills; headaches; malaise; hiccups; night sweats, nausea, and vomiting
Exam
right upper quadrant pain and tenderness on palpation; lower abdominal tenderness, cervical excitation pain, tender adnexa
1st investigation
- ultrasound right upper quadrant:
no gallstones
- CT abdomen/pelvis with oral and intravenous contrast:
may show enhancement of liver capsule
- nucleic acid amplification test or culture of vaginal secretions:
may culture Neisseria gonorrhoeae or Chlamydia trachomatis
Other investigations
- diagnostic laparoscopy with lysis of adhesions and peritoneal cultures:
may see peritonitis of liver surface and adjacent peritoneal surface; lysis of adhesions may provide relief of chronic symptoms; may culture N gonorrhoeae or C trachomatis
- pregnancy test:
negative
More
Ischaemic colitis
History
fever, vomiting, diarrhoea, abdominal pain, and bloody stools; history of vascular disease, recent abdominal aortic aneurysm repair, sepsis, myocardial infarct, or atrial fibrillation
Exam
diffuse abdominal pain or localised to area of colon affected with little or no distension
1st investigation
- FBC:
elevated WBC count
- serum lactate:
elevated if tissue hypoxia
- CT abdomen/pelvis with oral and intravenous contrast:
may show thickened and inflamed segments of colon; pneumatosis or gas in mesenteric veins suggestive of ischaemia
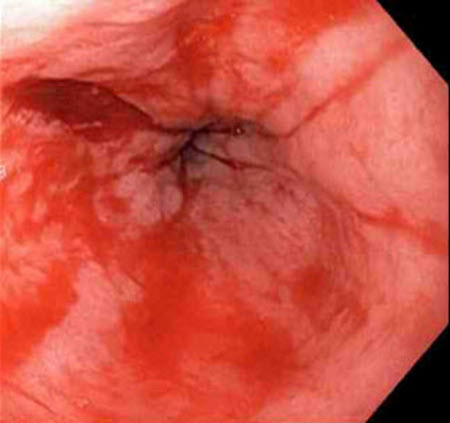
- colonoscopy:
pale or bluish mucosa with haemorrhagic lesions
Other investigations
- obstruction series:
pneumatosis or gas in mesenteric or portal vein but not specific to ischaemic colitis
- MRI abdomen with contrast:
may show thickened and inflamed segments of colon; pneumatosis or gas in mesenteric veins suggestive of ischaemia
- diagnostic laparoscopy:
full thickness ischaemia may be seen; ischaemia restricted to mucosa will not be seen
Ruptured splenic artery aneurysm
History
females and pregnant women; acute abdominal pain, may start in epigastrium or left upper quadrant and become diffuse; occasionally presents as gastrointestinal haemorrhage; dizziness, weakness, collapse
Exam
hypovolaemic shock; pallor; abdominal distension and tenderness
1st investigation
- CT abdomen/pelvis with intravenous contrast:
visualisation of aneurysm and haemorrhage
More
Other investigations
Budd-Chiari syndrome
History
female, age in third or fourth decade of life; use of oral contraceptive, pregnancy, and immediate postpartum period; history of myeloproliferative disorder and/or hypercoagulable states; right upper quadrant pain, history of liver failure/cirrhosis, variceal bleeding, ascites
Exam
right upper quadrant pain and tenderness; hepatosplenomegaly; jaundice; muscle wasting; ascites; leg oedema; truncal venous collaterals; disturbances of consciousness, intellectual function, behaviour, and neuromuscular function (hepatic encephalopathy)
1st investigation
- colour-flow Doppler ultrasound:
alterations in hepatic and/or caval veins in the form of thrombosis, stenosis, fibrotic cord, or insufficient recanalisation of the vessels
More
Other investigations
- MRI with pulsed sequencing:
thrombus, compression, and/or stenosis along the whole length of the inferior vena cava (IVC) or hepatic veins; necrosis and focal nodular hyperplasia in liver parenchyma; detect other lesions
More - CT abdomen/pelvis with triple-phase contrast:
occlusion of hepatic veins and/or IVC; areas with necrotic liver parenchyma; detect other lesions
- hepatic venography:
spider web pattern
More
Splenic infarct
History
ranges from asymptomatic to left upper quadrant pain, nausea, vomiting, fever, chills; may have pleuritic chest pain or left shoulder pain
Exam
tender left upper quadrant
1st investigation
- CT abdomen/pelvis with intravenous contrast:
visualisation of infarct
Other investigations
- MRI abdomen/pelvis intravenous gadolinium contrast:
visualisation of infarct
Abdominal wall haematoma
History
spontaneous or secondary to trauma, exercise, coughing, or procedure; acute abdominal pain with fever, nausea, vomiting; may report a mass or lump
Exam
signs of hypovolaemia with hypotension and tachycardia; localised abdominal pain and tenderness with non-pulsatile mass that is firm and painful; no mass may be palpable depending on location and depth of haematoma
1st investigation
- ultrasound abdominal wall:
haematoma visualised
More
Other investigations
- CT abdomen/pelvis with intravenous contrast:
haematoma visualised
More - FBC:
normal or low haemoglobin
- coagulation studies:
normal or deranged
Uraemia
History
confusion, depressed mental status; oliguria; tachycardia; pallor; fatigue; diffuse abdominal pain; thirst; excessive urination at night
Exam
diffuse abdominal pain, poor skin turgor, low blood pressure
1st investigation
- creatinine clearance:
reduced, usually <10 mL/min
- glomerular filtration rate:
reduced
- serum electrolytes:
abnormal
- urinalysis:
abnormal
Other investigations
- CT abdomen/pelvis with oral and intravenous contrast:
may reveal alternative cause for acute abdomen
Addisonian crisis
History
weight loss, nausea, vomiting, abdominal pain, anorexia, salt craving, fatigue, postural dizziness, syncope, confusion
Exam
cutaneous and mucosal hyperpigmentation, hypotension, pyrexia, and abdominal pain and/or guarding
1st investigation
- random cortisol level:
decreased
- rapid adrenocorticotropic hormone (ACTH) stimulation test:
limited increase in cortisol levels in response to ACTH stimulation
- CT abdomen/pelvis with oral and intravenous contrast:
may show bilateral enlargement of adrenal glands, adrenal haemorrhage, infiltrating diseases, or atrophic glands; may rule out other causes of abdominal pain and hypotension
- serum electrolytes:
often abnormal, typically with hypercalcaemia, hyponatremia, and hyperkalaemia
Other investigations
Hypercalcaemia
History
bone pain; depression; fatigue; confusion; nausea, anorexia; constipation; abdominal or flank pain; polyuria, polydipsia
Exam
non-specific findings; abdominal pain, hyperreflexia, tongue fasciculations, bony tenderness on palpation; hypertension and bradycardia
1st investigation
- corrected or ionised calcium:
elevated
- 12-lead ECG:
typically short QT interval and widened T waves
- serum parathyroid hormone:
elevated
Other investigations
- ultrasound neck:
may indicate hyperparathyroidism
- nuclear scan neck:
may indicate hyperparathyroidism
- MRI neck:
may indicate hyperparathyroidism
- CT abdomen/pelvis with oral and intravenous contrast:
may indicate alternative source of acute abdomen
Acute intermittent porphyria (AIP)
History
family history of acute porphyria, female sex predominates, nutritional alterations (e.g., fasting, dieting), intercurrent illness, and exposure to drugs or hormones known to provoke attacks of AIP; intermittent acute severe abdominal pain for days with symptoms out of proportion to the physical examination, often epigastric and colicky; nausea, vomiting; psychiatric symptoms (minor behavioural changes and insomnia to depression, agitation, and confusion); weakness in lower limbs; constipation; urinary hesitancy and dysuria
Exam
epigastric pain, tenderness, distension; fever, tachycardia, and hypertension; dark or red urine; central nervous system signs such as seizures, mental status changes, cortical blindness, and coma; weakness starting in lower limbs and ascending
1st investigation
- urinary porphobilinogen (PBG):
elevated; reddish colour
More
Other investigations
- obstruction series:
may show ileus
- CT abdomen/pelvis with oral and intravenous contrast:
may indicate alternative source of acute abdomen
Familial Mediterranean fever
History
mainly people of Mediterranean ancestry, especially from Arabian countries, Turkey, and Armenia; age <20 years; male sex; positive family history; episodic acute fever and pain in various places, the abdomen being the most common; pain can also occur in chest, joints, muscles, and skin; altered bowel habit (usually constipation)
Exam
fever, tachypnoea, acute abdominal pain with rigidity, rebound tenderness
1st investigation
- FBC:
leukocytosis ± thrombocytosis
- erythrocyte sedimentation rate:
elevated
- CRP:
elevated
- serum fibrinogen:
elevated
- LFTs:
rarely: elevated alanine aminotransferase and aspartate aminotransferase
- urinalysis:
proteinuria; haematuria suggests infection or vasculitis
- CT abdomen:
serositis; may show fluid and/or inflammation
Other investigations
- genetic testing:
positive for mutation
- pregnancy test:
negative
More
Typhlitis (neutropenic enterocolitis)
History
history of haematological malignancy and/or receiving chemotherapy or other immunosuppressive medicines; fever, abdominal pain, particularly right lower quadrant; nausea, vomiting, diarrhoea (sometimes bloody)
Exam
pyrexia; hypovolaemia from dehydration; marked abdominal pain and tenderness; may have septic shock; peritonitis
1st investigation
- CT abdomen/pelvis with oral and intravenous contrast:
dilated/distended caecum with thickening and inflammation; may show pneumatosis, localised perforation, phlegmon, or abscess formation
More - absolute neutrophil count:
neutropenia
- blood cultures:
may culture infective organism
- stool culture (including Clostridium difficile toxin):
may culture infective organism
Radiation enteritis
History
history of radiation treatment in recent or distant past; acute radiation enteritis produces nausea, vomiting, abdominal pain, diarrhoea, anorexia, diarrhoea/watery stools; chronic radiation enteritis produces obstructive symptoms (distention, nausea, vomiting, reduced flatus) if stricturing has occurred or malabsorptive symptoms (bloating, cramping, flatus, bulky stools, diarrhoea, weight loss) if mucosal integrity has been damaged; gastrointestinal bleeding if intestinal ulceration has occurred
Exam
abdominal pain and tenderness without distension in acute enteritis; passage of blood or mucus per rectum; obstructive findings include distension with tenderness and guarding, tympanism, tinkling bowel sounds, dehydration; abdominal bloating, mild abdominal tenderness; steatorrhoea, weight loss with malabsorption
1st investigation
- CT abdomen/pelvis with oral and intravenous contrast:
thickening and inflammation of bowel segments affected
Other investigations
- upper gastrointestinal series with small bowel follow-through:
shows extent of radiation injury; stricturing of bowel; fistula formation; thickening of bowel wall
- enteroclysis:
shows extent of radiation injury; stricturing of bowel; fistula formation; thickening of bowel wall
More - endoscopy:
shows mucosal integrity
More
Heavy metal poisoning
History
medical/environmental/occupational history consistent with exposure; nausea, persistent vomiting, diarrhoea, abdominal pain
Exam
anaemia, dehydration, neurological findings, abdominal pain and tenderness; encephalopathy, cardiomyopathy, dysrhythmias, acute tubular necrosis, and metabolic acidosis
1st investigation
- FBC with blood smear:
haematocrit and haemoglobin values reduced; smear either normochromic and normocytic or hypochromic and microcytic
- serum electrolytes and urea:
may be normal or deranged
- LFTs:
normal or elevated
- urinalysis:
presence of heavy metal at elevated levels
- venous blood lead level:
elevated in lead exposure
Other investigations
Spider bite
History
possible spider bite (e.g., black widow spider); fever, chills, nausea, vomiting, and severe, acute diffuse abdominal pain
Exam
diffuse abdominal pain and tenderness; abdominal muscle rigidity; profuse sweating; tachycardia
1st investigation
- clinical diagnosis:
diagnosis is based on history and examination
Other investigations
Use of this content is subject to our disclaimer






 ]
]