The primary goal of treatment is to suppress and normalise prolactin levels, thus restoring ovulation in women and normalising testosterone and sexual function in men.
In addition, patients with macroprolactinomas are treated to achieve tumour size reduction and decrease mass effects, particularly visual defects. Intolerable galactorrhoea also requires active treatment.
Women with microprolactinomas, mild galactorrhoea, and normal menstrual cycles may be monitored and not treated.
Treatment with dopamine agonists
Medical treatment with dopamine agonists is the primary treatment in men and women for both microprolactinomas and macroprolactinomas.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
[13]Samperi I, Lithgow K, Karavitaki N. Hyperprolactinaemia. J Clin Med. 2019 Dec 13;8(12):2203.
https://www.mdpi.com/2077-0383/8/12/2203/htm
http://www.ncbi.nlm.nih.gov/pubmed/31847209?tool=bestpractice.com
Dopamine agonists are potent inhibitors of prolactin secretion and synthesis. These agents reduce the volume of the lactotroph cells, thus decreasing the size of both micro- and macroprolactinomas. This continuous treatment will normalise prolactin in about 90% of patients; restore gonadal function, libido, and fertility; and shrink the tumour.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
Galactorrhoea should disappear.
Cabergoline is the recommended first-line dopamine agonist due to superior efficacy in normalising serum prolactin and reducing tumour size, better tolerability, and a more convenient dosing regimen.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
[13]Samperi I, Lithgow K, Karavitaki N. Hyperprolactinaemia. J Clin Med. 2019 Dec 13;8(12):2203.
https://www.mdpi.com/2077-0383/8/12/2203/htm
http://www.ncbi.nlm.nih.gov/pubmed/31847209?tool=bestpractice.com
Treatment usually starts at low doses to avoid adverse effects, with a gradual dose escalation during the first months upon achieving control of the hyperprolactinaemia and tumour shrinkage. After these are achieved, and prolactin is stably controlled for 1-2 years, the dopamine agonist dose can be gradually decreased, provided it maintains normal prolactin levels and controls tumour size.
Women with microprolactinomas and amenorrhoea or menstrual irregularities, who do not desire pregnancy, may be offered oestrogen/progesterone treatment instead of a dopamine agonist.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
Besides providing contraception, this treatment will achieve menstrual regularity. Oral oestrogen/progesterone treatment does not appear to promote growth of microprolactinomas.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
Because the dopamine agonists bromocriptine and cabergoline decrease prolactin levels and promote the return of a regular menstrual cycle and ovulation, pregnancy may occur whilst women are taking these medications. They are usually discontinued as soon as pregnancy is confirmed.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
In those patients with large macroprolactinomas, particularly those abutting the optic chiasm, dopamine agonists may be continued throughout pregnancy.[14]Vilar L, Abucham J, Albuquerque JL, et al. Controversial issues in the management of hyperprolactinemia and prolactinomas - an overview by the Neuroendocrinology Department of the Brazilian Society of Endocrinology and Metabolism. Arch Endocrinol Metab. 2018 Mar-Apr;62(2):236-63.
https://www.scielo.br/j/aem/a/YYhNDhks3xZndj8xG99bM3F/?lang=en
http://www.ncbi.nlm.nih.gov/pubmed/29768629?tool=bestpractice.com
[15]Maiter D. Prolactinoma and pregnancy: from the wish of conception to lactation. Ann Endocrinol (Paris). 2016 Jun;77(2):128-34.
http://www.ncbi.nlm.nih.gov/pubmed/27130071?tool=bestpractice.com
Due to its more widespread use, women are more likely to be receiving cabergoline rather than bromocriptine for treatment of their prolactinoma at the time of conception. Cabergoline has been introduced more recently than bromocriptine, and therefore, there are fewer safety data relating to maternal and fetal exposure to cabergoline compared with bromocriptine. Nevertheless, observational research has been unable to find an increase in miscarriage or fetal malformations in association with exposure to cabergoline in early pregnancy.[16]O'Sullivan SM, Farrant MT, Ogilvie CM, et al. An observational study of pregnancy and post-partum outcomes in women with prolactinoma treated with dopamine agonists. Aust N Z J Obstet Gynaecol. 2020 Jun;60(3):405-11.
http://www.ncbi.nlm.nih.gov/pubmed/31583693?tool=bestpractice.com
Bromocriptine is an alternative dopamine agonist that can be used for this indication.
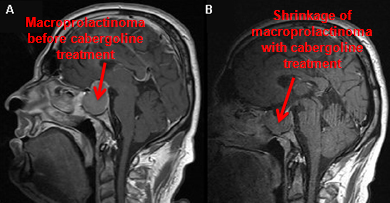
Post-menopausal women with microadenoma or undetectable pituitary mass do not usually require any treatment. Galactorrhoea usually improves when endogenous oestrogen decreases post-menopausally.[Figure caption and citation for the preceding image starts]: Gadolinium-enhanced magnetic resonance imaging (coronal view) showing a 40 mm pituitary macroprolactinoma in a 41-year-old man before (A) and after (B) 2-month treatment with cabergolineFrom the collection of Dr Ilan Shimon [Citation ends].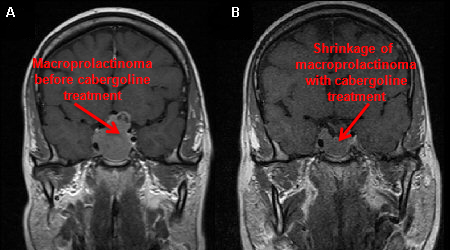 [Figure caption and citation for the preceding image starts]: Gadolinium-enhanced magnetic resonance imaging (sagittal view) showing a 40 mm pituitary macroprolactinoma in a 41-year-old man before (A) and after (B) 2-month treatment with cabergolineFrom the collection of Dr Ilan Shimon [Citation ends].
[Figure caption and citation for the preceding image starts]: Gadolinium-enhanced magnetic resonance imaging (sagittal view) showing a 40 mm pituitary macroprolactinoma in a 41-year-old man before (A) and after (B) 2-month treatment with cabergolineFrom the collection of Dr Ilan Shimon [Citation ends].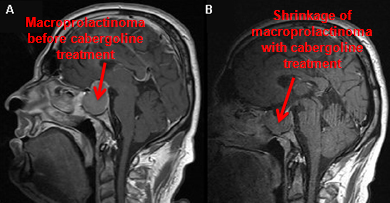
Dopamine agonist resistance and intolerance
Patients in whom prolactin does not normalise on maximally tolerated doses of dopamine agonists, or tumour size is not reduced by 50%, are considered to be dopamine agonist resistant.[13]Samperi I, Lithgow K, Karavitaki N. Hyperprolactinaemia. J Clin Med. 2019 Dec 13;8(12):2203.
https://www.mdpi.com/2077-0383/8/12/2203/htm
http://www.ncbi.nlm.nih.gov/pubmed/31847209?tool=bestpractice.com
Resistance to cabergoline occurs in approximately 10% of patients with a microprolactinoma compared with 15% to 20% with a macroprolactinoma.[17]Maiter D. Management of dopamine agonist-resistant prolactinoma. Neuroendocrinology. 2019;109(1):42-50.
https://www.karger.com/Article/FullText/495775
http://www.ncbi.nlm.nih.gov/pubmed/30481756?tool=bestpractice.com
Patients resistant or intolerant to dopamine agonists should be referred for trans-sphenoidal surgery, in centres with experienced neurosurgeons, for prolactinoma resection.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
[18]Donoho DA, Laws ER Jr. The role of surgery in the management of prolactinomas. Neurosurg Clin N Am. 2019 Oct;30(4):509-14.
http://www.ncbi.nlm.nih.gov/pubmed/31471058?tool=bestpractice.com
Surgery will immediately improve visual function in most cases of macroprolactinomas compressing the optic tract. Trans-sphenoidal surgery may be complicated, particularly in cases of large and invasive macroadenomas, and can result in anterior pituitary dysfunction and/or diabetes insipidus requiring permanent hormonal replacement.
Malignant prolactinomas exhibiting metastatic spread within or outside the central nervous system are rare. Radiotherapy is rarely used and is reserved for dopamine agonist-resistant or malignant prolactinomas.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
Dopamine agonists and valvular heart disease
Reported associations between high doses of cabergoline used in the treatment of Parkinson's disease and cardiac valvulopathy has led to concerns about the safety of cabergoline treatment in patients with prolactinomas.[19]De Vecchis R, Esposito C, Ariano C. Cabergoline use and risk of fibrosis and insufficiency of cardiac valves: meta-analysis of observational studies. Herz. 2013 Dec;38(8):868-80.
http://www.ncbi.nlm.nih.gov/pubmed/23743769?tool=bestpractice.com
However, patients receiving cabergoline for hyperprolactinaemia are typically younger, female, and taking much lower doses than those used in Parkinson's disease. Evidence does not support a clinically significant association between cabergoline treatment for prolactinomas and valvular heart disease.[20]Stiles CE, Lloyd G, Bhattacharyya S, et al. Incidence of cabergoline-associated valvulopathy in primary care patients with prolactinoma using hard cardiac endpoints. J Clin Endocrinol Metab. 2021 Jan 23;106(2):e711-20.
https://academic.oup.com/jcem/article/106/2/e711/6009022
http://www.ncbi.nlm.nih.gov/pubmed/33247916?tool=bestpractice.com
Recommendations on the timing and frequency of screening for cardiac valve disease in patients receiving cabergoline for hyperprolactinaemia vary.[21]Caputo C, Prior D, Inder WJ. The need for annual echocardiography to detect cabergoline-associated valvulopathy in patients with prolactinoma: a systematic review and additional clinical data. Lancet Diabetes Endocrinol. 2015 Nov;3(11):906-13.
http://www.ncbi.nlm.nih.gov/pubmed/25466526?tool=bestpractice.com
[22]Steeds RP, Stiles CE, Sharma V, et al. Echocardiography and monitoring patients receiving dopamine agonist therapy for hyperprolactinaemia: a joint position statement of the British Society of Echocardiography, the British Heart Valve Society and the Society for Endocrinology. Echo Res Pract. 2019 Mar 1;6(1):G1-8.
https://echo.biomedcentral.com/track/pdf/10.1530/ERP-18-0069.pdf
http://www.ncbi.nlm.nih.gov/pubmed/30825409?tool=bestpractice.com
Patients should receive the lowest effective dose of cabergoline for the shortest possible duration. Echocardiographic surveillance may be performed on patients likely to receive moderate or high doses of cabergoline for a considerable duration.[22]Steeds RP, Stiles CE, Sharma V, et al. Echocardiography and monitoring patients receiving dopamine agonist therapy for hyperprolactinaemia: a joint position statement of the British Society of Echocardiography, the British Heart Valve Society and the Society for Endocrinology. Echo Res Pract. 2019 Mar 1;6(1):G1-8.
https://echo.biomedcentral.com/track/pdf/10.1530/ERP-18-0069.pdf
http://www.ncbi.nlm.nih.gov/pubmed/30825409?tool=bestpractice.com
[23]Gamble D, Fairley R, Harvey R, et al. Screening for valve disease in patients with hyperprolactinaemia disorders prescribed cabergoline: a service evaluation and literature review. Ther Adv Drug Saf. 2017 Jul;8(7):215-29.
https://journals.sagepub.com/doi/10.1177/2042098617703647
http://www.ncbi.nlm.nih.gov/pubmed/28845230?tool=bestpractice.com
Dopamine agonists and psychiatric adverse effects
Although dopamine agonists are well tolerated by the majority of patients for prolactinoma management, a small number of patients may develop psychiatric disturbances, including impulse control disorders.[14]Vilar L, Abucham J, Albuquerque JL, et al. Controversial issues in the management of hyperprolactinemia and prolactinomas - an overview by the Neuroendocrinology Department of the Brazilian Society of Endocrinology and Metabolism. Arch Endocrinol Metab. 2018 Mar-Apr;62(2):236-63.
https://www.scielo.br/j/aem/a/YYhNDhks3xZndj8xG99bM3F/?lang=en
http://www.ncbi.nlm.nih.gov/pubmed/29768629?tool=bestpractice.com
Further studies are needed to elucidate specific risk factors for the development of psychiatric disturbance with dopamine agonists, but currently, clinicians are advised to monitor carefully for mood disturbance and the development of impulse control disorders. For those patients with pre-existing psychiatric disorders, dopamine agonists should be used with caution in the management of prolactinoma, and alternative treatment options, such as trans-sphenoidal surgery, should be considered.
Dopamine agonist withdrawal
In view of concerns about the association of the long-term use of dopamine agonists with valvular heart disease, there has been emphasis on a trial of drug withdrawal in certain patients with prolactinoma to minimise exposure.[24]Dekkers OM, Lagro J, Burman P, et al. Recurrence of hyperprolactinemia after withdrawal of dopamine agonists: systematic review and meta-analysis. J Clin Endocrinol Metab. 2010 Jan;95(1):43-51.
https://academic.oup.com/jcem/article/95/1/43/2835124
http://www.ncbi.nlm.nih.gov/pubmed/19880787?tool=bestpractice.com
A trial of dopamine agonist withdrawal is most likely to be successful if attempted in patients in whom there has been restoration of normal serum prolactin, significant reduction in tumour size on magnetic resonance imaging, low maintenance doses of dopamine agonists, and a treatment duration of at least 2 years.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
[25]Xia MY, Lou XH, Lin SJ, et al. Optimal timing of dopamine agonist withdrawal in patients with hyperprolactinemia: a systematic review and meta-analysis. Endocrine. 2018 Jan;59(1):50-61.
http://www.ncbi.nlm.nih.gov/pubmed/29043560?tool=bestpractice.com
Remission of hyperprolactinaemia in patients with prolactinoma following dopamine agonist withdrawal varies between studies, with greater success in microprolactinomas (approximately 40%) compared to macroprolactinomas (approximately 30%).[25]Xia MY, Lou XH, Lin SJ, et al. Optimal timing of dopamine agonist withdrawal in patients with hyperprolactinemia: a systematic review and meta-analysis. Endocrine. 2018 Jan;59(1):50-61.
http://www.ncbi.nlm.nih.gov/pubmed/29043560?tool=bestpractice.com
Because approximately one third of patients may develop secondary hypogonadism following recurrence of hyperprolactinaemia, regular monitoring of serum prolactin for the first year after drug withdrawal is recommended, with pituitary magnetic resonance imaging if hyperprolactinaemia recurs.[11]Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.
https://academic.oup.com/jcem/article/96/2/273/2709487
http://www.ncbi.nlm.nih.gov/pubmed/21296991?tool=bestpractice.com
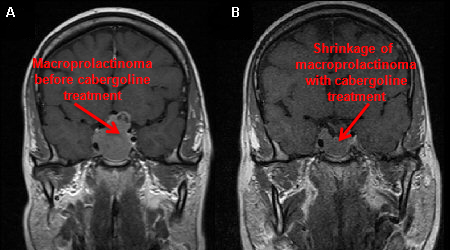 [Figure caption and citation for the preceding image starts]: Gadolinium-enhanced magnetic resonance imaging (sagittal view) showing a 40 mm pituitary macroprolactinoma in a 41-year-old man before (A) and after (B) 2-month treatment with cabergolineFrom the collection of Dr Ilan Shimon [Citation ends].
[Figure caption and citation for the preceding image starts]: Gadolinium-enhanced magnetic resonance imaging (sagittal view) showing a 40 mm pituitary macroprolactinoma in a 41-year-old man before (A) and after (B) 2-month treatment with cabergolineFrom the collection of Dr Ilan Shimon [Citation ends].