Approach
Clinical evaluation
AS is often diagnosed during the decades-long subclinical phase while a murmur, noted on physical examination, is being investigated. Even patients with severe AS may be truly asymptomatic, although early symptoms may be subtle. A careful history is important to determine if the patient has altered his or her habits in response to slowly worsening stenosis.
Decreased exercise tolerance, shortness of breath on exertion, exertional chest pain (angina), exertional syncope or near syncope, and heart failure symptoms should prompt consideration of AS.[26] Patients have an increased risk of gastrointestinal bleeding due to arteriovenous malformations. They are also more likely to develop chronic gastrointestinal bleeding that is associated with angiodysplasia. This may be due to turbulent flow across the stenotic valve producing an acquired von Willebrand deficiency (Heyde syndrome), which resolves with aortic valve replacement.
The physical examination is the most important screening tool for valvular heart disease. A complete cardiac examination including precordial palpation, auscultation with attention to murmurs and the aortic closure sound, and evaluation of arterial and venous pulsation is essential in the diagnostic workup for AS.
Murmurs are generally graded on a scale of 1 to 6:
Grade 1: murmur is faint and heard only with effort
Grade 2: murmur is faint but easily detected
Grade 3: murmur is loud
Grade 4: murmur is very loud and associated with a palpable thrill
Grade 5: murmur is so loud that it can be heard with only the edge of the stethoscope
Grade 6: murmur is extremely loud and heard even when the stethoscope is no longer in contact with the patient.
The typical murmur of AS is a systolic murmur ≥3/6, with a diamond-shaped crescendo-decrescendo pattern that peaks in mid-systole and radiates to the carotid arteries. The murmur is generally loudest at the right upper sternal border and terminates with S2 and the end of systole. As the severity of stenosis worsens, the murmur peaks later in systole and may be accompanied by a palpable thrill. The aortic heart sound (A2) is delayed as the systolic ejection period becomes prolonged. In severe stenosis, paradoxical splitting of the second heart sound may be noted such that in expiration, the pulmonic sound (P2) is heard before A2. The intensity of the second heart sound tends to be diminished as the severity of stenosis increases and leaflet mobility is reduced. [Figure caption and citation for the preceding image starts]: The systolic crescendo-decrescendo murmur of aortic stenosisFrom the collection of David Liff, MD, Emory University Hospital; used with permission [Citation ends].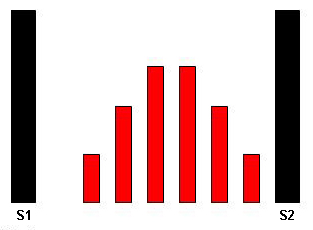
Auscultation sounds: Aortic stenosis (severe)
Uncommon findings include the presence of a holosystolic murmur at the apex (Gallavardin's phenomenon), mimicking the murmur of mitral regurgitation.
A delayed and diminished carotid upstroke (carotid parvus et tardus) may occur with severe AS, although this finding is often difficult to distinguish in older patients. In these patients, palpation of the brachial artery may reveal this finding.
ECG
An ECG is indicated in the initial work-up of all patients and is abnormal in >90% of patients with AS, with the most common abnormality being left ventricular hypertrophy (LVH) due to pressure overload.[27] Evidence of LVH and absent Q waves helps distinguish AS from other conditions such as aortic sclerosis with ischaemic heart disease. Patients with AS often have conduction disease manifesting as atrioventricular (AV) block, hemiblock, or bundle branch block.[Figure caption and citation for the preceding image starts]: ECG showing changes associated with left ventricular hypertrophyFrom the collection of Melanie Everitt MD, Heart Failure & Transplantation Program, Primary Children's Medical Center, Salt Lake City, UT; used with permission [Citation ends].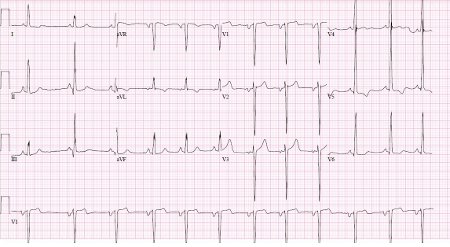
How to record an ECG. Demonstrates placement of chest and limb electrodes.
Transthoracic echocardiography (TTE)
TTE is the test of choice in the evaluation of suspected AS and for the evaluation of murmurs detected on physical examination. Doppler TTE can reliably and accurately detect the presence of a pressure gradient across the aortic valve. It can also assess left ventricle function and the presence of hypertrophy. It is essential for the diagnosis of AS and for serial evaluation once the diagnosis has been established.[26]
The American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommend TTE when there is:[26]
An unexplained systolic murmur
A single second heart sound
A history of a bicuspid aortic valve
Symptoms that might be due to AS.
The ACC/AHA also recommend that measurements taken during echocardiography examination should be used to grade the severity of AS.[26]
Although murmur intensity does not correlate well with the haemodynamic significance of the associated lesion, grade 3 murmurs are generally thought to reflect more significant lesions and thus warrant further evaluation with TTE. In practice, most patients with suspected cardiac disease and a murmur on examination should have an echocardiogram.
In the UK, the National Institute for Health and Care Excellence (NICE) recommends:[28]
To consider echocardiography if the patient has a murmur and no other signs or symptoms, but valve disease is suspected based on:
the nature of the murmur,
family history,
age (especially if >75 years), or
medical history (e.g., history of atrial fibrillation).
To arrange echocardiography for any patient with suspected valve disease and:
signs or symptoms of valve disease (such as peripheral oedema, angina, or breathlessness);
an abnormal ECG; or
an ejection systolic murmur with reduced second heart sound but no other signs or symptoms.
To refer for urgent (within 2 weeks) specialist assessment and echocardiography if valve disease is suspected, and the patient has:
A systolic murmur and exertional syncope. If the combination of specialist assessment and echocardiography is not available, urgent echocardiography alone should be performed.
A murmur and severe symptoms (such as angina or breathlessness on minimal exertion or at rest) which are thought to be due to valvular heart disease.
Chest x-ray
In patients with known or suspected valvular heart disease, a chest x-ray is indicated as part of the initial assessment to assess the presence or absence of pulmonary congestion or other lung pathology.[26]
Further testing
If there are discrepancies between the physical examination and initial non-invasive testing (ECG, TTE, and chest x-ray), further non-invasive (cardiac computed tomography [CT], cardiac magnetic resonance imaging [MRI], CT angiography, magnetic resonance angiography [MRA], ECG exercise stress testing, and dobutamine stress echo) or invasive (transoesophageal echocardiography, cardiac catheterisation) testing should be considered, to determine optimal treatment strategy.[26]
Cardiac CT
Cardiac CT allows both qualitative and quantitative evaluation of the calcium burden on the aortic valve.
The ACC/AHA guidelines recommend use of the Agaston aortic valve calcium score, which can be calculated and used to make the diagnosis of severe AS when echocardiography or invasive measurements are inconclusive. This is particularly helpful in the evaluation of low-flow low-gradient AS.[29][30]
NICE in the UK recommends to consider using cardiac CT to measure aortic valve calcium score if the severity of symptomatic AS is uncertain.[28]
Cardiac MRI
Cardiac MRI (cMRI) provides detailed, dynamic images of the heart. It allows for analysis of cardiac function and haemodynamics. cMRI may be useful when trying to distinguish between true valvular stenosis and subvalvular stenosis related to a subvalvular membrane.
Owing to the complexity of cMRI, the ACC/AHA recommend transthoracic echocardiography as the preferred test for evaluating AS, but state that cMRI may be a good option if echocardiography fails to yield quality images.[26]
If cMRI shows mid-wall fibrosis in adults with severe AS, NICE in the UK recommends enhanced follow up (e.g., more frequent reviews) and further assessment (e.g., stress echocardiography) to monitor the need for intervention.[28]
Late gadolinium enhancement in particular has shown potential for use to be used in AS risk stratification.[31]
CT angiography (CTA)
CTA uses a thin-section CT acquisition that is timed to coincide with peak arterial or venous enhancement. The resulting 3-dimensional image allows characterisation and reporting of aortic valve morphology.[29] CTA can also be used to screen for coronary artery disease before valular surgery.[32]
MRA
MRA has been found to produce good reproducibility of aortic annulus dimensions and calcifications in comparison with cardiac CTA, even in the presence of arrhythmias.[33] MRA may not be suitable; however, when there is a high-susceptibility artifact, magnetic field incompatible devices, and severe arrhythmia.[29] MRA examination is also technically more complex, with longer study time and a higher required degree of patient cooperation, which some patients may find problematic.[29][34]
ECG exercise stress testing
Symptomatic patients should not have exercise testing and should be referred for valve replacement.[26] For those without symptoms, symptom-limited exercise testing may provide clinically important information.[26][35] A positive stress test shows either decreased exercise tolerance (compared with normal for age and sex) or a drop in systolic blood pressure of 10mmHg with exercise.[26] Nearly 40% of patients with asymptomatic AS will develop symptoms with exercise testing.[36] Exercise echocardiography may add additional diagnostic and prognostic information.[26][37][38] In a group of patients with asymptomatic severe AS, a positive exercise stress test was highly predictive of the onset of symptoms or the need for surgery. At 24 months, only 19% with a positive exercise test remained symptom-free or without valve replacement compared with 85% of those with a negative test.[39] Subsequent work found that the development of symptoms on exercise testing was the strongest predictor for the onset of spontaneous symptoms, especially among patients <70 years old in whom symptoms of fatigue and breathlessness are more specific than in older patients.[40]
How to record an ECG. Demonstrates placement of chest and limb electrodes.
Dobutamine stress echo
The ACC/AHA recommend this test for patients with a low transvalvular gradient and left ventricular systolic dysfunction (low ejection fraction), in order to identify pseudostenosis and the presence of contractile reserve (≥20% increase in stroke volume with dobutamine).[26] Patients with pseudostenosis do not have severe AS and should not be referred for aortic valve replacement. The presence of contractile reserve suggests a better prognosis and lower perioperative risk with surgical aortic valve replacement; however, it does not predict outcomes after transcatheter aortic valve implantation.
NICE in the UK recommends that stress echocardiography be used as part of further assessment to monitor need for intervention if cardiac MRI shows mid-wall fibrosis in adults with severe AS.[28]
Transoesophageal echocardiography (TOE)
TOE provides alternate detailed views of the aortic valve apparatus, and is frequently used in patients undergoing valve surgery or transcatheter aortic valve replacement.[29][Figure caption and citation for the preceding image starts]: Transoesophageal echocardiogram showing the left ventricle outflow tract (LVOT), the aorta (Ao), and nearly immobile leaflets (arrows) of a severely stenotic aortic valveFrom the collection of David Liff, MD, Emory University Hospital; used with permission [Citation ends].
Cardiac catheterisation
Cardiac catheterisation is no longer a first-line test for diagnosis of AS. As a diagnostic tool it is used when echo-Doppler examination is inconclusive or there is a discrepancy between non-invasive findings and the history and physical examination.[26] In addition, cardiac catheterisation can be very helpful when the diagnosis of low-flow low-gradient aortic valve stenosis is being considered, as it allows measurement of the cardiac output and hence accurate determination of the aortic valve area and stroke volume. Furthermore, catheterisation remains essential prior to aortic valve replacement for the evaluation of coronary artery anatomy.
Use of this content is subject to our disclaimer