Investigations
1st investigations to order
thyroid-stimulating hormone (TSH)
Test
Initial laboratory screening test.[48]
Reference range may differ among assays, but typically serum TSH is 0.4 to 4.0 mIU/L. A value below the reference range suggests hyperthyroidism.[48]
Most symptomatic hyperthyroid Graves' disease patients have a serum TSH less than the detection limit of third-generation assays (e.g., <0.01 mIU/L).[49]
Patients with subclinical disease have low serum TSH levels with peripheral thyroid hormone levels within the reference range.[7][8][9]
Low levels of serum TSH are also seen in non-thyroidal illness, in pituitary hypothalamic disease, and with use of some medicines.
Order the test initially and also for follow-up and monitoring of therapy.
Result
suppressed
serum free or total T4
Test
The diagnosis of hyperthyroidism is confirmed by high serum levels of free T4 and total or free T3 in the presence of a low TSH.[2][45] Total T4 measurements may give misleading results because they are affected by protein binding; measurement of the free fraction of T4 is preferred.
In mild Graves’ disease, free T4 levels may be normal, but T3 may be elevated ('T3 toxicosis').[45]
Reference range may differ between assays, but typically free T4 is 10.3 to 23.2 pmol/L (0.8 to 1.8 ng/dL).
Order free T4 and serum TSH together for diagnosis, and for monitoring therapy.
Result
elevated, except in T3 toxicosis or subclinical disease
serum free or total T3
Test
The diagnosis of hyperthyroidism is confirmed by high serum levels of free T4 and total or free T3 in the presence of a low TSH.[2][45] Total T3 measurements may give misleading results because they are affected by protein binding. Total T3 is, however, commonly used because of limitations with free T3 assays.[45][49]
In mild Graves’ disease, free T4 levels may be normal, but T3 may be elevated ('T3 toxicosis').[45]
Reference range may differ between assays, but typically free T3 is 3.5 to 6.5 pmol/L (2.3 to 4.2 picograms/mL or 230-420 picograms/dL) and total T3 is 1.2 to 2.8 pmol/L (80-180 ng/dL).
Order if TSH suggests hyperthyroidism but free T4 is normal, to differentiate clinical hyperthyroidism (T3 toxicosis) from subclinical hyperthyroidism.
Result
elevated, except in subclinical disease
TSH receptor antibodies (TRAb)
Test
Measured by either immunoassay or bioassay, TSH receptor antibodies are typically elevated in >90% of patients with Graves’ disease. Reference range may differ between laboratories.
Older patients with Graves’ disease tend to have lower thyroid hormone elevation for the same level of circulating TSH receptor antibodies compared with younger patients.[53]
Bioassays allow differentiation of TSH receptor-stimulating antibodies and TSH receptor-blocking antibodies, facilitating prediction of: extrathyroidal manifestations; and, fetal or neonatal hyperthyroidism among pregnant and postnatal women with Graves' disease.[48][49]
Immunoassays measure inhibition of TSH receptor binding and are unable to distinguish between thyroid-stimulating and thyroid-blocking antibodies.
Result
positive
Investigations to consider
calculation of total T3/T4 or FT3/FT4 ratio
Test
It may be helpful to calculate total T3/T4 or FT3/FT4 ratio to distinguish thyroiditis from Graves' disease, and from toxic nodular goitre (when radioiodine uptake is contraindicated e.g., in pregnancy or lactation).[52]
A high T3/T4 ratio is suggestive of Graves’ disease rather than thyroiditis.[50][51]
Result
likely to be high compared with thyroiditis
radioactive iodine or technetium-99 uptake
Test
If TSH receptor antibody testing is negative and the cause of thyrotoxicosis is unknown, thyroid uptake of radioactive iodine-123 (I-123) or technetium-99 (Tc-99) may be considered.[54]
I-123 or Tc-99 uptake provides a quantitative measure of the accumulation and retention of radioactive tracer by the thyroid.
Radioactive tracer uptake can inform the diagnosis, and is useful in excluding low-uptake hyperthyroid syndromes such as painless thyroiditis. Additionally, results from the radioactive iodine uptake test can be used in treatment planning.
Normal 24-hour uptake is 14% to 24%. Upper limit of normal increases with iodine deficiency.
Thyroid uptake is used less since TSH receptor antibody measurement became more widely available.
Result
elevated
thyroid scan (scintigraphy)
Test
Thyroid scan using I-123 or Tc-99 allows the evaluation of thyroid tissue by showing the distribution pattern of the radioactive tracer (via two-dimensional images).
Thyroid scan can differentiate Graves’ disease (diffuse uptake) from toxic multinodular goitre (patchy with focal areas of increased uptake).[2][45]
Thyroid scan is used less since TSH receptor antibody measurement became more widely available.
Result
diffuse uptake
thyroid peroxidase antibodies (TPOAb)
Test
May be helpful if TSH receptor antibody testing is unavailable and/or isotope scans are contraindicated (e.g., in pregnancy or lactation).
70% of patients with Graves’ disease will be positive.
Result
positive
thyroid ultrasound
Test
Highly sensitive for detection of thyroid nodules.
Order a thyroid ultrasound when nodules are suspected on examination or present on thyroid scan. Colour-flow Doppler may help to distinguish Graves' disease (increased flow) from painless thyroiditis and amiodarone-induced hyperthyroidism (reduced flow).[2][45][55]
May also be used for thyroid volume estimation for calculation of dose of radioactive iodine.
Thyroid ultrasound should not routinely be ordered if there is no palpable abnormality of the thyroid gland.[56][57]
[Figure caption and citation for the preceding image starts]: Iodine uptake scans. Typical appearances of absent uptake in thyroiditis (top panel). Diffuse increased uptake in Graves' disease (lower left panel). Areas of increased and decreased uptake in toxic multinodular goitre (lower middle panel). Single area of increased uptake in a toxic adenoma (lower right panel)Courtesy of Dr Petros Perros [Citation ends].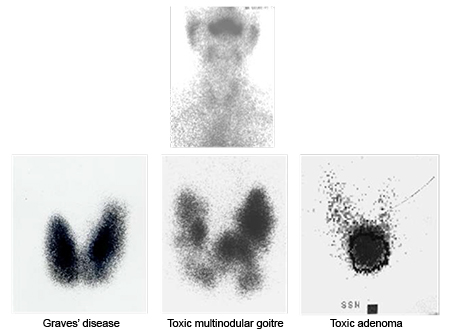
Result
highly vascular; diffuse; enlarged
CT or MRI scan of orbit
Test
May be needed to confirm euthyroid orbitopathy, or exclude other processes when proptosis is asymmetrical or if presentation is atypical (e.g., no previous or present evidence of thyroid dysfunction, absence of upper eyelid retraction, divergent strabismus, diplopia sole manifestation, history of diplopia worsening towards the end of the day).[34]
Result
may show muscle thickening
Use of this content is subject to our disclaimer