Evaluate patients for thyroid disorders when they have unexplained weight loss, palpitations, atrial fibrillation or other supraventricular tachycardias, tremor, generalised proximal muscle weakness, or unexplained protrusion of the eyes.[2]Smith TJ, Hegedüs L. Graves' disease. N Engl J Med. 2016 Oct 20;375(16):1552-65.
http://www.ncbi.nlm.nih.gov/pubmed/27797318?tool=bestpractice.com
[4]Boelaert K, Torlinska B, Holder RL, et al. Older subjects with hyperthyroidism present with a paucity of symptoms and signs – a large cross-sectional study. J Clin Endocrinol Metab. 2010 Jun;95(6):2715-26.
http://www.ncbi.nlm.nih.gov/pubmed/20392869?tool=bestpractice.com
[45]Chaker L, Cooper DS, Walsh JP, et al. Hyperthyroidism. Lancet. 2024 Feb 24;403(10428):768-80.
http://www.ncbi.nlm.nih.gov/pubmed/38278171?tool=bestpractice.com
Investigate diffuse enlargement of the thyroid, particularly if there is a bruit. Moist and velvety skin, hair loss, onycholysis, menstrual irregularities in women, and sexual dysfunction might also be associated with hyperthyroidism.[2]Smith TJ, Hegedüs L. Graves' disease. N Engl J Med. 2016 Oct 20;375(16):1552-65.
http://www.ncbi.nlm.nih.gov/pubmed/27797318?tool=bestpractice.com
[46]Kakuno Y, Amino N, Kanoh M, et al. Menstrual disturbances in various thyroid diseases. Endocr J. 2010;57(12):1017-22.
https://www.doi.org/10.1507/endocrj.k10e-216
http://www.ncbi.nlm.nih.gov/pubmed/20938101?tool=bestpractice.com
[47]Gabrielson AT, Sartor RA, Hellstrom WJG. The impact of thyroid disease on sexual dysfunction in men and women. Sex Med Rev. 2019 Jan;7(1):57-70.
https://www.doi.org/10.1016/j.sxmr.2018.05.002
http://www.ncbi.nlm.nih.gov/pubmed/30057137?tool=bestpractice.com
Symptoms such as unexplained weight loss and generalised weakness may cause a patient to be concerned about an underlying malignant cause. Order appropriate investigations and follow patient safety-netting procedures where any symptoms of malignancy are present that cannot be explained by another cause.
Diagnosis is mostly clinical. The combination of elevated thyroid-stimulating hormone (TSH) receptor antibodies (or elevated radioactive iodine/technetium-99 uptake by the thyroid if TSH receptor antibody testing is unavailable or diagnosis is uncertain); suppressed TSH; and elevated levels of circulating thyroid hormones (free T4 and total or free T3) is the standard for diagnosis of Graves' hyperthyroidism.
Subclinical hyperthyroidism
A number of otherwise asymptomatic individuals may be diagnosed with subclinical hyperthyroidism due to Graves’ disease on routine tests for other indications. Take a detailed clinical history (including family history of autoimmune diseases), carry out a physical examination, and repeat the thyroid function tests along with TSH receptor antibody after 8-12 weeks to determine if the biochemical abnormality is transient (such as due to non-thyroidal illness) or due to an autoimmune process.
Laboratory tests
Request a serum TSH assay as the initial laboratory screening test.[48]Kahaly GJ, Bartalena L, Hegedüs L, et al. 2018 European Thyroid Association guideline for the management of Graves' hyperthyroidism. Eur Thyroid J. 2018 Jul 25;7(4):167-86.
https://etj.bioscientifica.com/view/journals/etj/7/4/ETJ490384.xml
http://www.ncbi.nlm.nih.gov/pubmed/30283735?tool=bestpractice.com
Serum TSH and circulating thyroid hormones
Most symptomatic hyperthyroid Graves' disease patients have a serum TSH less than the detection limit of third-generation assays (e.g., <0.01 mIU/L).[49]Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016 Oct;26(10):1343-421.
http://online.liebertpub.com/doi/full/10.1089/thy.2016.0229
http://www.ncbi.nlm.nih.gov/pubmed/27521067?tool=bestpractice.com
The diagnosis of hyperthyroidism is confirmed by high serum levels of free T4 and total or free T3 in the presence of a low TSH.[2]Smith TJ, Hegedüs L. Graves' disease. N Engl J Med. 2016 Oct 20;375(16):1552-65.
http://www.ncbi.nlm.nih.gov/pubmed/27797318?tool=bestpractice.com
[45]Chaker L, Cooper DS, Walsh JP, et al. Hyperthyroidism. Lancet. 2024 Feb 24;403(10428):768-80.
http://www.ncbi.nlm.nih.gov/pubmed/38278171?tool=bestpractice.com
Total T4 and T3 measurements may give misleading results because they are affected by protein binding; measurement of the free fraction of T4 is preferred. Total T3 is commonly used because of limitations with free T3 assays.[45]Chaker L, Cooper DS, Walsh JP, et al. Hyperthyroidism. Lancet. 2024 Feb 24;403(10428):768-80.
http://www.ncbi.nlm.nih.gov/pubmed/38278171?tool=bestpractice.com
[49]Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016 Oct;26(10):1343-421.
http://online.liebertpub.com/doi/full/10.1089/thy.2016.0229
http://www.ncbi.nlm.nih.gov/pubmed/27521067?tool=bestpractice.com
In mild Graves' disease, free T4 levels may be normal, but T3 may be elevated ('T3 toxicosis').[45]Chaker L, Cooper DS, Walsh JP, et al. Hyperthyroidism. Lancet. 2024 Feb 24;403(10428):768-80.
http://www.ncbi.nlm.nih.gov/pubmed/38278171?tool=bestpractice.com
A high T3/T4 ratio is suggestive of Graves’ disease rather than thyroiditis.[50]Yoshimura Noh J, Momotani N, Fukada S, et al. Ratio of serum free triiodothyronine to free thyroxine in Graves' hyperthyroidism and thyrotoxicosis caused by painless thyroiditis. Endocr J. 2005 Oct;52(5):537-42.
https://www.jstage.jst.go.jp/article/endocrj/52/5/52_5_537/_article
http://www.ncbi.nlm.nih.gov/pubmed/16284430?tool=bestpractice.com
[51]Sriphrapradang C, Bhasipol A. Differentiating Graves' disease from subacute thyroiditis using ratio of serum free triiodothyronine to free thyroxine. Ann Med Surg (Lond). 2016 Aug 8;10:69-72.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4990637
http://www.ncbi.nlm.nih.gov/pubmed/27570620?tool=bestpractice.com
It may be helpful to calculate total T3/T4 or FT3/FT4 ratio to distinguish thyroiditis from Graves' disease, and from toxic nodular goitre (when radioiodine uptake is contraindicated e.g., in pregnancy or lactation).[52]Amino N, Yabu Y, Miki T, et al. Serum ratio of triiodothyronine to thyroxine, and thyroxine-binding globulin and calcitonin concentration in Graves' disease and destruction-induced thyrotoxicosis. J Clin Endocrinol Metab. 1981 Jul;53(1):113-6.
http://www.ncbi.nlm.nih.gov/pubmed/6165731?tool=bestpractice.com
Patients with subclinical disease have low serum TSH levels with peripheral thyroid hormone levels within the reference range.[7]Mitchell AL, Pearce SH. How should we treat patients with low serum thyrotropin concentrations? Clin Endocrinol (Oxf). 2010 Mar;72(3):292-6.
http://www.ncbi.nlm.nih.gov/pubmed/19744106?tool=bestpractice.com
[8]Col NF, Surks MI, Daniels GH. Subclinical thyroid disease: clinical applications. JAMA. 2004 Jan 14;291(2):239-43.
http://www.ncbi.nlm.nih.gov/pubmed/14722151?tool=bestpractice.com
[9]Biondi B, Palmieri EA, Klain M, et al. Subclinical hyperthyroidism: clinical features and treatment options. Eur J Endocrinol. 2005 Jan;152(1):1-9.
http://www.ncbi.nlm.nih.gov/pubmed/15762182?tool=bestpractice.com
TSH receptor antibodies
Measured by either immunoassay or bioassay, TSH receptor antibodies are typically elevated in >90% of patients with Graves’ disease. Reference range may differ between laboratories.
Older patients with Graves’ disease tend to have lower thyroid hormone elevation for the same level of circulating TSH receptor antibodies compared with younger patients.[53]Bano A, Gan E, Addison C, et al. Age may influence the impact of TRAbs on thyroid function and relapse-risk in patients with Graves disease. J Clin Endocrinol Metab. 2019 May 1;104(5):1378-85.
http://www.ncbi.nlm.nih.gov/pubmed/30517711?tool=bestpractice.com
Bioassays allow differentiation of TSH receptor-stimulating antibodies and TSH receptor-blocking antibodies, facilitating prediction of: extrathyroidal manifestations; and, fetal or neonatal hyperthyroidism among pregnant and postnatal women with Graves' disease.[48]Kahaly GJ, Bartalena L, Hegedüs L, et al. 2018 European Thyroid Association guideline for the management of Graves' hyperthyroidism. Eur Thyroid J. 2018 Jul 25;7(4):167-86.
https://etj.bioscientifica.com/view/journals/etj/7/4/ETJ490384.xml
http://www.ncbi.nlm.nih.gov/pubmed/30283735?tool=bestpractice.com
[49]Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016 Oct;26(10):1343-421.
http://online.liebertpub.com/doi/full/10.1089/thy.2016.0229
http://www.ncbi.nlm.nih.gov/pubmed/27521067?tool=bestpractice.com
Immunoassays measure inhibition of TSH receptor binding and are unable to distinguish between thyroid-stimulating and thyroid-blocking antibodies.
Thyroid peroxidase antibodies
Testing for thyroid peroxidase antibodies may be helpful if TSH receptor antibody testing is unavailable and/or isotope scans are contraindicated (e.g., in pregnant women). 70% of people with Graves’ disease will be positive.
Radiological tests
Do not request radiological tests in patients with thyrotoxic biochemistry and elevated TSH receptor antibodies.
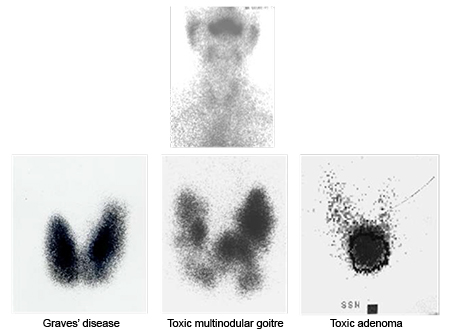
If TSH receptor antibody testing is negative and the cause of thyrotoxicosis is unknown, thyroid uptake of radioactive iodine-123 (I-123) or technetium-99 (Tc-99) may be considered.[54]Goichot B, Leenhardt L, Massart C, et al. Diagnostic procedure in suspected Graves' disease. Ann Endocrinol (Paris). 2018 Dec;79(6):608-17.
http://www.ncbi.nlm.nih.gov/pubmed/30220410?tool=bestpractice.com
I-123 or Tc-99 uptake provides a quantitative measure of the accumulation and retention of radioactive tracer by the thyroid. Radioactive tracer uptake can inform the diagnosis, and is useful in excluding low-uptake hyperthyroid syndromes such as painless thyroiditis. Additionally, results from the radioactive iodine uptake test can be used in treatment planning.
Thyroid scan (scintigraphy) using I-123 or Tc-99 allows the evaluation of thyroid tissue by showing the distribution pattern of the radioactive tracer (via two-dimensional images). Thyroid scan can differentiate Graves’ disease (diffuse uptake) from toxic multinodular goitre (patchy with focal areas of increased uptake).[2]Smith TJ, Hegedüs L. Graves' disease. N Engl J Med. 2016 Oct 20;375(16):1552-65.
http://www.ncbi.nlm.nih.gov/pubmed/27797318?tool=bestpractice.com
[45]Chaker L, Cooper DS, Walsh JP, et al. Hyperthyroidism. Lancet. 2024 Feb 24;403(10428):768-80.
http://www.ncbi.nlm.nih.gov/pubmed/38278171?tool=bestpractice.com
Thyroid uptake and scan is used less since TSH receptor antibody measurement became more widely available.
Thyroid ultrasound
Order a thyroid ultrasound when nodules are suspected on examination or present on thyroid scan. Colour-flow Doppler may help to distinguish Graves' disease (increased flow) from painless thyroiditis and amiodarone-induced hyperthyroidism (reduced flow).[2]Smith TJ, Hegedüs L. Graves' disease. N Engl J Med. 2016 Oct 20;375(16):1552-65.
http://www.ncbi.nlm.nih.gov/pubmed/27797318?tool=bestpractice.com
[45]Chaker L, Cooper DS, Walsh JP, et al. Hyperthyroidism. Lancet. 2024 Feb 24;403(10428):768-80.
http://www.ncbi.nlm.nih.gov/pubmed/38278171?tool=bestpractice.com
[55]Bogazzi F, Vitti P. Could improved ultrasound and power Doppler replace thyroidal radioiodine uptake to assess thyroid disease? Nat Clin Pract Endocrinol Metab. 2008 Feb;4(2):70-1.
http://www.ncbi.nlm.nih.gov/pubmed/17984981?tool=bestpractice.com
Thyroid ultrasound should not routinely be ordered if there is no palpable abnormality of the thyroid gland.[56]The Journal of Healthcare Contracting. Choosing wisely: Endocrine Society and American Association of Clinical Endocrinologists. 2024 [internet publication].
https://www.jhconline.com/choosing-wiselyendocrine-society-and-american-association-of-clinical-endocrinologists.html
[57]Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules - 2016 update. Endocr Pract. 2016 May;22(5):622-39.
https://www.endocrinepractice.org/article/S1530-891X(20)42954-4/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/27167915?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Iodine uptake scans. Typical appearances of absent uptake in thyroiditis (top panel). Diffuse increased uptake in Graves' disease (lower left panel). Areas of increased and decreased uptake in toxic multinodular goitre (lower middle panel). Single area of increased uptake in a toxic adenoma (lower right panel)Courtesy of Dr Petros Perros [Citation ends].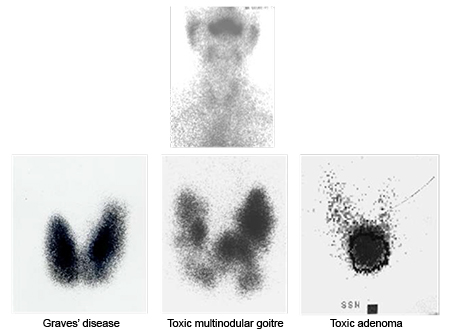
Orbitopathy/dermopathy
Examine patients carefully for bilateral proptosis and lid retraction. In the presence of hyperthyroidism, these clinical features are sufficient for the diagnosis of Graves' orbitopathy.
Request cross-sectional imaging of the orbit (i.e., CT or MRI scan) in patients with euthyroid unilateral orbitopathy, or other atypical presentations (e.g., no previous or present evidence of thyroid dysfunction, absence of upper eyelid retraction, divergent strabismus, diplopia sole manifestation, history of diplopia worsening towards the end of the day); demonstration of typical muscle thickening is needed in order to rule out other diagnoses.[34]Perros P, Neoh C, Dickinson J. Thyroid eye disease. BMJ. 2009 Mar 6;338:b560.
http://www.ncbi.nlm.nih.gov/pubmed/19270020?tool=bestpractice.com
Elevated TSH receptor antibodies increase the probability of the diagnosis being Graves' orbitopathy, but this measure is no substitute for orbital imaging if there is suspicion of an alternative diagnosis.[3]Davies TF, Andersen S, Latif R, et al. Graves' disease. Nat Rev Dis Primers. 2020 Jul 2;6(1):52.
https://www.doi.org/10.1038/s41572-020-0184-y
http://www.ncbi.nlm.nih.gov/pubmed/32616746?tool=bestpractice.com
[34]Perros P, Neoh C, Dickinson J. Thyroid eye disease. BMJ. 2009 Mar 6;338:b560.
http://www.ncbi.nlm.nih.gov/pubmed/19270020?tool=bestpractice.com
[58]Bartalena L, Kahaly GJ, Baldeschi L, et al. The 2021 European Group on Graves' orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves' orbitopathy. Eur J Endocrinol. 2021 Aug 27;185(4):G43-G67.
https://www.doi.org/10.1530/EJE-21-0479
http://www.ncbi.nlm.nih.gov/pubmed/34297684?tool=bestpractice.com
Examine the patient for thyroid dermopathy (pretibial myxoedema), which may present as non-pitting oedema, plaque, nodule(s), or elephantiasis.[19]Fatourechi V, Pajouhi M, Fransway AF. Dermopathy of Graves disease (pretibial myxedema): review of 150 cases. Medicine. 1994 Jan;73(1):1-7.
http://www.ncbi.nlm.nih.gov/pubmed/8309359?tool=bestpractice.com
In the presence of Graves' orbitopathy, this is diagnostic of Graves' disease. Dermopathy and/or acropachy without orbitopathy are exceptionally rare and should raise suspicion of alternative causes for the skin and nail changes. In questionable cases, request a skin biopsy.[59]Schwartz KM, Fatourechi V, Ahmed DD, et al. Dermopathy of Graves' disease (pretibial myxedema): long-term outcome. J Clin Endocrinol Metab. 2002 Feb;87(2):438-46.
http://www.ncbi.nlm.nih.gov/pubmed/11836263?tool=bestpractice.com
[60]Fatourechi V, Ahmed DDF, Schwartz KM. Thyroid acropachy: report of 40 patients treated at a single institution in a 26-year period. J Clin Endocrinol Metab. 2002 Dec;87(12):5435-41.
http://www.ncbi.nlm.nih.gov/pubmed/12466333?tool=bestpractice.com
Be aware that Graves' orbitopathy is often diagnosed late or misdiagnosed as allergy or conjunctivitis, especially when the eye symptoms precede the diagnosis of Graves' disease.
It is currently unclear whether mild Graves' orbitopathy is a chronic relapsing and remitting process or whether it is a transient event in the course of illness.[61]Anagnostis P, Boboridis K, Adamidou F, et al. Natural course of mild Graves' orbitopathy: is it a chronic remitting or a transient disease? J Endocrinol Invest. 2017 Mar;40(3):257-61.
http://www.ncbi.nlm.nih.gov/pubmed/27664101?tool=bestpractice.com
The DiaGO (diagnosis of Graves' orbitopathy) test is a 20-point assessment tool that can be used by clinicians (including non-ophthalmic specialists) to help identify patients with Graves' orbitopathy; however, confirmatory studies are required before this can be used in clinical practice.[62]Mitchell AL, Goss L, Mathiopoulou L, et al. Diagnosis of Graves' orbitopathy (DiaGO): results of a pilot study to assess the utility of an office tool for practicing endocrinologists. J Clin Endocrinol Metab. 2015 Mar;100(3):E458-62.
http://www.ncbi.nlm.nih.gov/pubmed/25485725?tool=bestpractice.com
Guidelines on early detection and management of Graves' orbitopathy have been published.[58]Bartalena L, Kahaly GJ, Baldeschi L, et al. The 2021 European Group on Graves' orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves' orbitopathy. Eur J Endocrinol. 2021 Aug 27;185(4):G43-G67.
https://www.doi.org/10.1530/EJE-21-0479
http://www.ncbi.nlm.nih.gov/pubmed/34297684?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Lid retraction, mild proptosis, and mild chemosisCourtesy of Dr Vahab Fatourechi [Citation ends]. [Figure caption and citation for the preceding image starts]: Pretibial myxoedema (non-pitting oedema)Courtesy of Dr Vahab Fatourechi [Citation ends].
[Figure caption and citation for the preceding image starts]: Pretibial myxoedema (non-pitting oedema)Courtesy of Dr Vahab Fatourechi [Citation ends]. [Figure caption and citation for the preceding image starts]: Orbitopathy and elephantiasisCourtesy of Dr Vahab Fatourechi [Citation ends].
[Figure caption and citation for the preceding image starts]: Orbitopathy and elephantiasisCourtesy of Dr Vahab Fatourechi [Citation ends]. [Figure caption and citation for the preceding image starts]: Axial CT scan through the orbits of a patient with Graves' orbitopathy showing increased thickness of medial rectiCourtesy of Dr Petros Perros [Citation ends].
[Figure caption and citation for the preceding image starts]: Axial CT scan through the orbits of a patient with Graves' orbitopathy showing increased thickness of medial rectiCourtesy of Dr Petros Perros [Citation ends].
 [Figure caption and citation for the preceding image starts]: Pretibial myxoedema (non-pitting oedema)Courtesy of Dr Vahab Fatourechi [Citation ends].
[Figure caption and citation for the preceding image starts]: Pretibial myxoedema (non-pitting oedema)Courtesy of Dr Vahab Fatourechi [Citation ends]. [Figure caption and citation for the preceding image starts]: Orbitopathy and elephantiasisCourtesy of Dr Vahab Fatourechi [Citation ends].
[Figure caption and citation for the preceding image starts]: Orbitopathy and elephantiasisCourtesy of Dr Vahab Fatourechi [Citation ends]. [Figure caption and citation for the preceding image starts]: Axial CT scan through the orbits of a patient with Graves' orbitopathy showing increased thickness of medial rectiCourtesy of Dr Petros Perros [Citation ends].
[Figure caption and citation for the preceding image starts]: Axial CT scan through the orbits of a patient with Graves' orbitopathy showing increased thickness of medial rectiCourtesy of Dr Petros Perros [Citation ends].