Approach
Diagnosis is made following the presence of key clinical factors together with microscopy of skin scrapings.
History
Patients with scabies almost invariably complain of pruritus, particularly at night. Although the classic symptom is intense pruritus that is classically worse at night, this timing is not specific to scabies. This is true of many pruritic conditions given that patients are typically more distracted during the daytime.
A history of close contact with an individual known to have scabies or of pruritus in other family members should prompt suspicion of scabies. Other factors in the history may include immunosuppression, age less than 15 years or over 65 years, overcrowded living conditions, institutionalisation, neurological disorders, and sexual contact with new or multiple partners.[1]
Physical examination
Patients may have linear lesions, papules, or nodules. Nodules are particularly common on the penis. Linear burrows are often seen in the interdigital web spaces.[1]
Thick, crusted lesions occurring on elbows, knees, hands, and feet with dystrophic nails are features of crusted or Norwegian scabies, which is more commonly seen in the immunocompromised patient.
The ink burrow test can also be useful in making a diagnosis.[14] A suspected lesion is marked with a purple surgical marking pen. The ink is then wiped away with isopropyl alcohol and reveals a linear burrow in cases of scabies.[Figure caption and citation for the preceding image starts]: Penile nodules, characteristic of scabiesPhotograph courtesy of Joseph C. English, III, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Characteristic linear burrows in skinFrom the collection of Laura Ferris, MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Characteristic linear burrows in skinFrom the collection of Laura Ferris, MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Hyperkeratotic palms in a patient with Norwegian scabiesPhotograph courtesy of Joseph C. English, III, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Hyperkeratotic palms in a patient with Norwegian scabiesPhotograph courtesy of Joseph C. English, III, MD [Citation ends].
Microscopy
Ectoparasite preparation of skin scrapings from papules or burrows of infested patients may show mites, their eggs, or faecal matter. Papules or linear lesions should be scraped with a number 15 scalpel blade that has first been dipped in liquid paraffin. Multiple (4 or more) lesions should be scraped from each patient. Scraping should be sufficient to cause bleeding. Liquid paraffin, rather than potassium hydroxide, should be used because the latter can actually dissolve the mite faecal matter. Although these findings are diagnostic of scabies and this is a recommended procedure for all patients suspected to have scabies, they are not necessary for the initiation of treatment in cases where the clinical suspicion is high.[5]
Epiluminescence light microscopy, or dermatoscopy, is an emerging investigation, which has the advantage of being inexpensive and non-invasive.[15] Dermatoscopy has been shown to be an accurate method for diagnosis when performed by a properly trained practitioner.[14] It employs a hand-held device that magnifies the skin in such a way that colour and structure in the epidermis, dermo-epidermal junction, and papillary dermis become more visible. Under the dermatoscope, the scabies mite appears as a characteristic triangular or circumflex shape located at one end of the linear burrow.[16][Figure caption and citation for the preceding image starts]: Scabies mite under 10× powerFrom the collection of Laura Ferris, MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Eggs and stool under 10× powerFrom the collection of Laura Ferris, MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Eggs and stool under 10× powerFrom the collection of Laura Ferris, MD, PhD [Citation ends].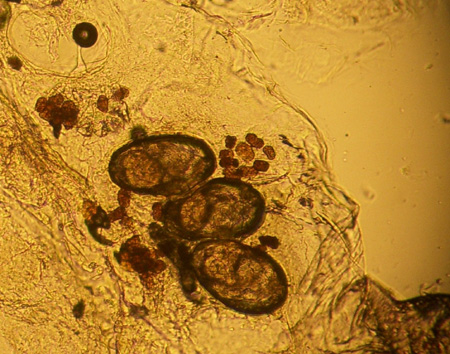 [Figure caption and citation for the preceding image starts]: Classic dermoscopic image of triangle or 'delta wing jet' sign of dense scabies head parts (long red arrow), relatively translucent scabies body (long black arrow), scabies eggs (short red arrows), and classic S-shaped burrowFox G. Diagnosis of scabies by dermoscopy. BMJ Case Rep. 2009;2009:bcr06.2008.0279. [Citation ends].
[Figure caption and citation for the preceding image starts]: Classic dermoscopic image of triangle or 'delta wing jet' sign of dense scabies head parts (long red arrow), relatively translucent scabies body (long black arrow), scabies eggs (short red arrows), and classic S-shaped burrowFox G. Diagnosis of scabies by dermoscopy. BMJ Case Rep. 2009;2009:bcr06.2008.0279. [Citation ends].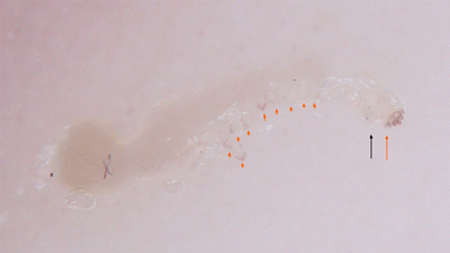
Skin biopsy
Skin biopsy may be done if the ectoparasite preparation is negative, in order to look for an alternative diagnosis. However, it is rare to see a mite in the biopsy specimen, and the eosinophilic infiltrate seen in most biopsies is non-specific and not sufficient for diagnosis.[17]
Use of this content is subject to our disclaimer