Aetiology
Scabies is caused by infection with the ectoparasite Sarcoptes scabiei, variety hominis. This 0.3- to 0.5-mm mite burrows into the epidermis and tunnels through the stratum corneum, laying 2 to 4 eggs per day. The eggs produce larvae that hatch in 2 to 4 days and develop into adult mites approximately 2 weeks later. The average parasite burden of an infested individual is 10 to 12 mites. Transmission is primarily via direct and prolonged skin-to-skin contact, although transmission via shared clothing and bedding can occur. Mites can live away from their host for an average of 24 to 36 hours. Survival is prolonged at lower ambient temperature and higher humidity. However, mites lose infestation capability the longer they are away from their host. In young adults transmission is often sexual. Patients with higher parasitic burden are more infective. Patients who are immunosuppressed (e.g., due to HIV, human T-cell leukaemia virus type 1 [HTLV-1] infection, malignancy, iatrogenic suppression, or leprosy) may develop Norwegian or crusted scabies. The skin of these patients may contain thousands to millions of mites, and they are highly contagious.[6][Figure caption and citation for the preceding image starts]: Scabies mite under 10× powerFrom the collection of Laura Ferris, MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Histological section showing an adult Sarcoptes scabiei in its burrow in the stratum corneumFrom the collection of Pooja Khera, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Histological section showing an adult Sarcoptes scabiei in its burrow in the stratum corneumFrom the collection of Pooja Khera, MD [Citation ends].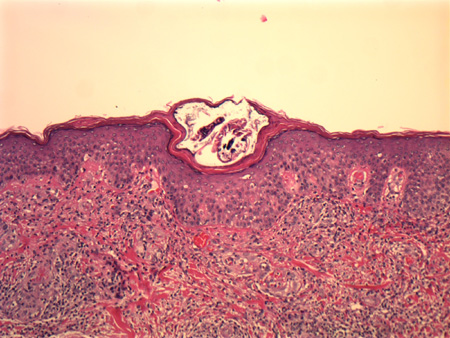
Pathophysiology
The linear burrows seen in the skin of patients with scabies are caused directly by the tunnelling mite, although they are generally visible only once they become erythematous. The pruritus, erythema, papules, and nodules seen in affected individuals are due to the host immune response to the mite, explaining why signs and symptoms appear 3 to 4 weeks after initial infestation but within a day upon re-infestation. The immune response is of the Th2 type characterised by increased interleukin-4 and immunoglobulin E production. Immunity seems to offer some protection from scabies as re-infestation of the sensitised patient can be difficult in experimental settings.[6]
Classification
Clinical variants
Crusted scabies (scabies crustosa, Norwegian scabies) is a distinctive and highly contagious form of scabies that typically occurs in patients with a history of immunosuppression, neurological disorders, or institutionalisation. Clinically, patients have erythematous scaly plaques on the torso and extremities with hyperkeratotic plaques on the palms and soles with associated nail dystrophy.[2]
Use of this content is subject to our disclaimer