Investigations
1st investigations to order
chest x-ray
Test
Usually the first-line test, but rarely diagnostic. A normal chest radiograph does not rule out a small tumour.
Result
anterior mediastinal mass, wide mediastinum
chest CT with intravenous contrast medium
Test
The most useful imaging test.[24][32] Intravenous contrast is administered (if not contraindicated) to evaluate for invasion of blood vessels, which is crucial for preoperative staging and therapeutic planning.
With thymoma, CT usually shows a discrete mass in the thymus, often with well-defined borders and preservation of fat planes; local invasion may be present.[3][Figure caption and citation for the preceding image starts]: CT scan of the chest showing a typical Masaoka-Koga stage I thymomaFrom the collection of Cameron Wright, MD; used with permission [Citation ends].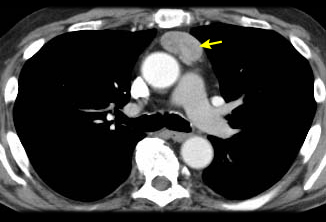 [Figure caption and citation for the preceding image starts]: CT scan of the chest showing thymoma with encasement and invasion of the superior vena cavaFrom the collection of Cameron Wright, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of the chest showing thymoma with encasement and invasion of the superior vena cavaFrom the collection of Cameron Wright, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan of the chest showing thymoma with encasement and invasion of the left innominate veinFrom the collection of Cameron Wright, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of the chest showing thymoma with encasement and invasion of the left innominate veinFrom the collection of Cameron Wright, MD; used with permission [Citation ends].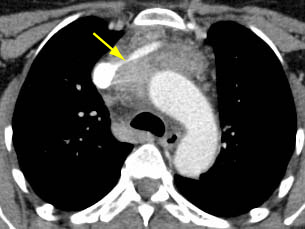
With thymic carcinoma, CT most commonly shows an invasive, poorly defined mediastinal mass with obliteration of mediastinal fat planes.
Aggressive, invasive thymoma and thymic carcinoma can appear virtually indistinguishable from anterior mediastinal lymphoma.
Vascular invasion, lymphadenopathy, and extrathymic metastases are common. May also contain calcification and necrosis.
Result
anterior mediastinal mass; superior vena cava obstruction, pleural or metastatic lung spread may be seen; there may be invasion of adjacent structures and organs
Investigations to consider
chest MRI
Test
Mainly used to confirm suspected cardiac invasion (with cardiac gating) based on CT results, or for staging when iodinated contrast medium is contraindicated. Chemical-shift MRI can be used to differentiate thymic hyperplasia from a thymic tumour.[25]
Result
anterior mediastinal mass; cardiac invasion may be seen
tissue biopsy
Test
Small, non-invasive lesions are usually resected for both diagnosis and treatment. Large, invasive, or unusual lesions, or those with metastatic spread, are usually first approached with a CT-guided core needle biopsy. Anterior mediastinotomy and video-assisted thoracoscopic surgery (VATS) to biopsy pleural implants are alternative approaches.
VATS is not recommended for biopsy of the primary tumour. [Figure caption and citation for the preceding image starts]: CT scan of the chest showing a typical Masaoka-Koga stage I thymomaFrom the collection of Cameron Wright, MD; used with permission [Citation ends].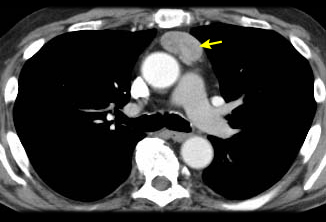 [Figure caption and citation for the preceding image starts]: CT scan of the chest showing Masaoka-Koga stage III thymoma with abutment of the anterior chest wall and invasion of the medial aspect of the left lungFrom the collection of Cameron Wright, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of the chest showing Masaoka-Koga stage III thymoma with abutment of the anterior chest wall and invasion of the medial aspect of the left lungFrom the collection of Cameron Wright, MD; used with permission [Citation ends].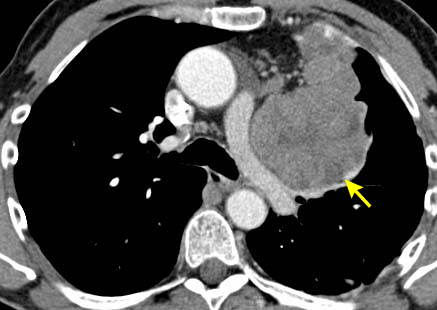 [Figure caption and citation for the preceding image starts]: CT scan of the chest showing Masaoka-Koga stage IVA thymoma with pleural effusion (red arrow) and extensive pleural metastases (yellow arrow) along posterior chest wallFrom the collection of Cameron Wright, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of the chest showing Masaoka-Koga stage IVA thymoma with pleural effusion (red arrow) and extensive pleural metastases (yellow arrow) along posterior chest wallFrom the collection of Cameron Wright, MD; used with permission [Citation ends].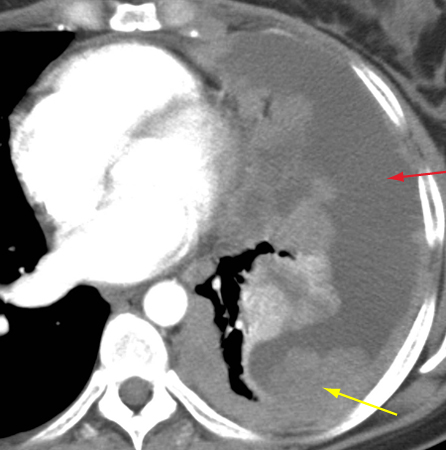
Result
specimen for pathological diagnosis
acetylcholine receptor antibodies
Test
Recommended in all patients with suspected or confirmed thymoma. Present in 80% to 90% of patients with myasthenia gravis.[30] May be elevated even without clinically evident myasthenia gravis.
Result
elevated titre (range varies with assay used)
FBC
Test
Anaemia may be a result of paraneoplastic pure-red-cell aplasia.
Result
normal or may show anaemia
PET/CT scan
Test
Helpful in avoiding biopsy for non-invasive tumours in young patients where lymphoma is a consideration (low maximum standardised uptake value [i.e., less than 7.5] renders lymphoma highly unlikely).
Can demonstrate unsuspected nodal or metastatic disease; of use when imaging or histological results suggest an aggressive thymic tumour or lymphoma.[29] In general, as WHO histology worsens, the intensity of the PET uptake (standardised uptake value) increases.
Result
may help identify nodal or metastatic disease; may help in differentiating between thymoma and lymphoma
serum alpha-fetoprotein (AFP)
Test
Younger patients who are outside the typical age group for thymoma (i.e., <40 years of age) should be evaluated for germ cell tumour with biochemical markers.
AFP is often elevated in germ cell tumours.
Result
>25 microgram/L (>25 nanogram/mL)
serum beta-human chorionic gonadotrophin (beta-hCG)
Test
Younger patients who are outside the typical age group for thymoma (i.e., <40 years of age) should be evaluated for germ cell tumour with biochemical markers.
Beta-HCG is often elevated in germ cell tumours.
Result
>0.7 IU/L
Use of this content is subject to our disclaimer