Initial history
History for mild TBI is centered on the injury event.
A typical history should begin with establishing how the injury occurred and whether the impact was directly to the head or transmitted to the head by the acceleration-deceleration of the body on impact, corroborated by an observer when possible.[5]Patricios JS, Schneider KJ, Dvorak J, et al. Consensus statement on concussion in sport: the 6th International Conference on concussion in sport-Amsterdam, October 2022. Br J Sports Med. 2023 Jun;57(11):695-711.
https://bjsm.bmj.com/content/57/11/695
http://www.ncbi.nlm.nih.gov/pubmed/37316210?tool=bestpractice.com
Somatic, cognitive, and affective symptoms should be enquired about, typically rated on a Likert scale to assess their severity. It is important to note the symptoms that occurred immediately after the injury was sustained, as well as those that are still present at the time of evaluation. A variety of symptom scales are available.[3]Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019 Feb;53(4):213-25.
https://bjsm.bmj.com/content/53/4/213.long
http://www.ncbi.nlm.nih.gov/pubmed/30705232?tool=bestpractice.com
It is common for symptoms to worsen the day after injury, especially in patients who have a positive history for mild TBI, including concussion.[51]Bruce JM, Echemendia RJ. Concussion history predicts self-reported symptoms before and following a concussive event. Neurology. 2004 Oct 26;63(8):1516-8.
http://www.ncbi.nlm.nih.gov/pubmed/15505180?tool=bestpractice.com
Previous brain traumas can lower the impact threshold, making mild TBI more likely regardless of the force of impact and, therefore, increasing the chances of future brain trauma.
Alcohol and substance misuse is associated with a significantly higher risk for all forms of TBI, but this is confounded by a higher overall risk for all forms of external injury.[34]Parry-Jones BL, Vaughan FL, Miles Cox W. Traumatic brain injury and substance misuse: a systematic review of prevalence and outcomes research (1994-2004). Neuropsychol Rehabil. 2006 Oct;16(5):537-60.
http://www.ncbi.nlm.nih.gov/pubmed/16952892?tool=bestpractice.com
[35]Taylor LA, Kreutzer JS, Demm SR, et al. Traumatic brain injury and substance abuse: a review and analysis of the literature. Neuropsychol Rehabil. 2003 Jan-Mar;13(1-2):165-88.
http://www.ncbi.nlm.nih.gov/pubmed/21854333?tool=bestpractice.com
Symptoms may fluctuate, but typically subside after a week to a month. Physicians should specifically enquire about the following symptoms:
Headache: the most commonly reported symptom.[52]Kraemer Y, Mäki K, Marinkovic I, et al. Post-traumatic headache after mild traumatic brain injury in a one-year follow up study - risk factors and return to work. J Headache Pain. 2022 Feb 19;23(1):27.
https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-022-01398-9
http://www.ncbi.nlm.nih.gov/pubmed/35183101?tool=bestpractice.com
[53]Hoem Nordhaug L, Vik A, Hagen K, et al. Headaches in patients with previous head injuries: a population-based historical cohort study (HUNT). Cephalalgia. 2016 Oct;36(11):1009-19.
https://journals.sagepub.com/doi/10.1177/0333102415618948
http://www.ncbi.nlm.nih.gov/pubmed/26634833?tool=bestpractice.com
Although often felt immediately, headache can worsen the day after the injury is sustained. 30% of patients with mild TBI continue to report headache at three months post-trauma.[54]Voormolen DC, Haagsma JA, Polinder S, et al. Post-concussion symptoms in complicated vs. uncomplicated mild traumatic brain injury patients at three and six months post-Injury: results from the CENTER-TBI study. J Clin Med. 2019 Nov 8;8(11):1921.
https://www.mdpi.com/2077-0383/8/11/1921
http://www.ncbi.nlm.nih.gov/pubmed/31717436?tool=bestpractice.com
Medication overuse, neck injuries, sleep disturbance and psychological comorbidity may all contribute to headache after mild TBI.[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
Disturbed gait/balance or dizziness: when occurring after a head injury, typically related to benign paroxysmal positional vertigo.[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
These symptoms may be alarming to patients if they do not settle quickly. Explaining that they are due to debris dislodged into the inner ear by the injury can help to alleviate patients’ concerns about "brain damage".[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
Vestibular migraine and depersonalization (a sense of disconnection from the body) are other causes of dizziness in this population. Central vestibular disorders can occur but are more typical after moderate or severe brain injury.[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
See Benign paroxysmal positional vertigo.
Mental slowing and fogginess: patients report these as a general feeling, often accompanied by difficulty sustaining attention, and general fatigue.[4]Mayer AR, Quinn DK, Master CL. The spectrum of mild traumatic brain injury: a review. Neurology. 2017 Aug 8;89(6):623-32.
http://www.ncbi.nlm.nih.gov/pubmed/28701496?tool=bestpractice.com
[6]Centers for Disease Control and Prevention. Report to Congress on traumatic brain injury in the United States: epidemiology and rehabilitation. 2015 [internet publication].
https://www.cdc.gov/traumaticbraininjury/pubs/congress_epi_rehab.html
Memory difficulties: these can be centered on the injury incident itself or generalized to include difficulty in day-to-day situations, and typically co-occur with other cognitive and/or physical symptoms, such as headaches. Memory lapses are common in the general population and are not specific to mild TBI.[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
Vomiting and nausea: less typical in adults, occurring much more frequently in adolescents and children. When vomiting is the only symptom of head injury in a child, TBI on CT is uncommon and clinically important TBI is very uncommon.[56]Dayan PS, Holmes JF, Atabaki S, et al. Association of traumatic brain injuries with vomiting in children with blunt head trauma. Ann Emerg Med. 2014 Jun;63(6):657-65.
https://www.annemergmed.com/article/S0196-0644(14)00021-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/24559605?tool=bestpractice.com
TBI is more frequent in children when vomiting is accompanied by other signs or symptoms suggestive of TBI.[56]Dayan PS, Holmes JF, Atabaki S, et al. Association of traumatic brain injuries with vomiting in children with blunt head trauma. Ann Emerg Med. 2014 Jun;63(6):657-65.
https://www.annemergmed.com/article/S0196-0644(14)00021-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/24559605?tool=bestpractice.com
Neck pain: more commonly associated with motor vehicle collisions than with other mechanisms of injury.[57]King JA, McCrea MA, Nelson LD. Frequency of primary neck pain in mild traumatic brain injury/concussion patients. Arch Phys Med Rehabil. 2020 Jan;101(1):89-94.
http://www.ncbi.nlm.nih.gov/pubmed/31493383?tool=bestpractice.com
If present, the patient should be assessed for a cervical spine injury. See Acute cervical spine trauma in adults.
Neuropsychological testing
Cognitive symptoms usually resolve quickly after mild TBI; a minority of patients have memory and concentration problems within three months of injury.[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
Neuropsychological testing involves paper-and-pencil or computerized tests assessing attention, memory, and executive functions, as well as reaction times. Routine referral for cognitive (psychometric) assessment is not recommended after mild TBI; careful assessment of the nature of the injury and symptoms, including bedside cognitive tests is more appropriate in the first instance.[55]van Gils A, Stone J, Welch K, et al. Management of mild traumatic brain injury. Pract Neurol. 2020 May;20(3):213-21.
http://www.ncbi.nlm.nih.gov/pubmed/32273394?tool=bestpractice.com
[68]Healthcare Improvement Scotland. Brain injury rehabilitation in adults: a national clinical guideline. Mar 2013 [internet publication].
https://www.sign.ac.uk/media/1068/sign130.pdf
[69]US Department of Veterans Affairs. VA/DoD clinical practice guidelines: management and rehabilitation of post-acute mild traumatic brain Injury (mTBI). 2021 [internet publication].
https://www.healthquality.va.gov/guidelines/rehab/mtbi/index.asp
Most guidelines support the use of formal sidelines or office-based cognitive testing for sports-related concussion.[3]Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019 Feb;53(4):213-25.
https://bjsm.bmj.com/content/53/4/213.long
http://www.ncbi.nlm.nih.gov/pubmed/30705232?tool=bestpractice.com
[5]Patricios JS, Schneider KJ, Dvorak J, et al. Consensus statement on concussion in sport: the 6th International Conference on concussion in sport-Amsterdam, October 2022. Br J Sports Med. 2023 Jun;57(11):695-711.
https://bjsm.bmj.com/content/57/11/695
http://www.ncbi.nlm.nih.gov/pubmed/37316210?tool=bestpractice.com
Cognitive performance can be affected by stress, fatigue, effort, and medications. Therefore, if testing is required, neuropsychological evaluations should be carried out by trained neuropsychologists who can disentangle the effects of these factors from the consequences of mild TBI. Guidelines on sport-related concussion support the use of neuropsychological testing to diagnose the effects of mild TBI, help make return-to-play decisions for athletes, and monitor recovery.[5]Patricios JS, Schneider KJ, Dvorak J, et al. Consensus statement on concussion in sport: the 6th International Conference on concussion in sport-Amsterdam, October 2022. Br J Sports Med. 2023 Jun;57(11):695-711.
https://bjsm.bmj.com/content/57/11/695
http://www.ncbi.nlm.nih.gov/pubmed/37316210?tool=bestpractice.com
It is important to ensure that an appropriate amount of time has passed between testing sessions to guard against practice effects and uphold test validity. Although neuropsychological tests are an important component of mild TBI assessment, they should not be the only benchmark in making decisions about recovery from a mild TBI.[70]Echemendia RJ, Iverson GL, McCrea M, et al. Advances in neuropsychological assessment of sport-related concussion. Br J Sports Med. 2013 Apr;47(5):294-8.
http://www.ncbi.nlm.nih.gov/pubmed/23479487?tool=bestpractice.com
Quick assessment tools
Quick assessment tools can be invaluable, particularly for sideline evaluations. They include:
Sport Concussion Assessment Tool (SCAT)
SCAT6: sport concussion assessment tool - 6th edition
Opens in new window[71]Echemendia RJ, Burma JS, Bruce JM, et al. Acute evaluation of sport-related concussion and implications for the Sport Concussion Assessment Tool (SCAT6) for adults, adolescents and children: a systematic review. Br J Sports Med. 2023 Jun;57(11):722-35.
https://bjsm.bmj.com/content/57/11/722
http://www.ncbi.nlm.nih.gov/pubmed/37316213?tool=bestpractice.com
The Child SCAT6 should be used in patients ages 8-12 years.
McGill Abbreviated Concussion Evaluation (ACE)[72]Johnston KM, Lassonde M, Ptito A. A contemporary neurosurgical approach to sport-related head injury: the McGill concussion protocol. J Am Coll Surg. 2001 Apr;192(4):515-24.
http://www.ncbi.nlm.nih.gov/pubmed/11294409?tool=bestpractice.com
various iterations of the ImPACT cognitive test for the assessment of signs and symptoms of head injury (e.g., ImPACT sideline card; ImPACT computerized concussion management tool; ImPACT pediatric computerized concussion management tool).
Regardless of the choice of assessment tool, an assessment of balance and postural stability is essential in the initial evaluation of the concussed athlete.
Brain imaging
In cases with loss of consciousness or impact seizure, patients should receive a comprehensive evaluation for serious brain or cervical spine injury.[4]Mayer AR, Quinn DK, Master CL. The spectrum of mild traumatic brain injury: a review. Neurology. 2017 Aug 8;89(6):623-32.
http://www.ncbi.nlm.nih.gov/pubmed/28701496?tool=bestpractice.com
CT is most commonly used because it rapidly rules out intracranial bleeding or bony injuries. The New Orleans Criteria or the Canadian CT head rule can be used as an assessment guide to imaging.[67]American College of Emergency Physicians. Mild Traumatic Brain Injury. May 2023 [internet publication].
https://www.acep.org/patient-care/clinical-policies/mild-traumatic-brain-injury2
[73]Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000 Jul 13;343(2):100-05.
http://www.nejm.org/doi/full/10.1056/NEJM200007133430204#t=article
http://www.ncbi.nlm.nih.gov/pubmed/10891517?tool=bestpractice.com
[74]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6.
http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com
Cases where there are positive imaging results may include prolonged alterations to consciousness, focal neurologic deficits, and worsening symptoms (typically uncontrollable headache, nausea, vomiting, and severe dizziness).[65]Davis GA, Iverson GL, Guskiewicz KM, et al. Contributions of neuroimaging, balance testing, electrophysiology and blood markers to the assessment of sport-related concussion. Br J Sports Med. 2009 May;43 Suppl 1:i36-45.
http://www.ncbi.nlm.nih.gov/pubmed/19433424?tool=bestpractice.com
[67]American College of Emergency Physicians. Mild Traumatic Brain Injury. May 2023 [internet publication].
https://www.acep.org/patient-care/clinical-policies/mild-traumatic-brain-injury2
[75]Stein SC, Spettell C. The head injury severity scale (HISS): a practical classification of closed-head injury. Brain Inj. 1995 Jul;9(5):437-44.
http://www.ncbi.nlm.nih.gov/pubmed/7550215?tool=bestpractice.com
[76]American College of Radiology. ACR appropriateness criteria: head trauma. 2015 [internet publication].
https://acsearch.acr.org/docs/69481/Narrative
Indications for admission to hospital should also be considered as strong indications to perform diagnostic imaging and include:
a Glasgow Coma Scale (GCS) score <15; or, after imaging, a GCS score that has not returned to 15 or the pre-injury baseline, regardless of the imaging results
post-traumatic seizure
signs of skull fracture or penetrating injury
loss of consciousness[66]Carroll LJ, Cassidy JD, Holm L, et al. Methodological issues and research recommendations for mild traumatic brain injury: the WHO Collaborating Centre Task Force on mild traumatic brain injury. J Rehabil Med. 2004 Feb;(43 suppl):113-25.
http://www.ncbi.nlm.nih.gov/pubmed/15083875?tool=bestpractice.com
severe persistent headache
persistent vomiting
meningism
cerebrospinal fluid leak
suspicion of ongoing post-traumatic anterograde or retrograde amnesia
a high-risk mechanism of injury (e.g., road traffic accident, significant fall)
suspected nonaccidental injury
a coagulopathy
receiving anticoagulant therapy[67]American College of Emergency Physicians. Mild Traumatic Brain Injury. May 2023 [internet publication].
https://www.acep.org/patient-care/clinical-policies/mild-traumatic-brain-injury2
previous brain surgery
current drug or alcohol intoxication
shock
focal neurologic deficit since the injury.
Do not routinely obtain head CT scans for patients with minor head injury who are at low risk based on validated decision rules.[67]American College of Emergency Physicians. Mild Traumatic Brain Injury. May 2023 [internet publication].
https://www.acep.org/patient-care/clinical-policies/mild-traumatic-brain-injury2
[77]American College of Emergency Physicians. Five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2013 [internet publication].
https://web.archive.org/web/20230326153926/https://www.choosingwisely.org/clinician-lists/american-college-emergency-physicians-ct-scans-of-head-for-emergency-department-patients-with-minor-head-injury
In children, use clinical observation/Pediatric Emergency Care Applied Research Network (PECARN) criteria to determine whether imaging is indicated.[78]American Academy of Pediatrics. Ten things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2022 [internet publication].
https://web.archive.org/web/20230325225612/https://www.choosingwisely.org/societies/american-academy-of-pediatrics
[79]American Association of Neurological Surgeons and Congress of Neurological Surgeons. Five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2022 [internet publication].
https://web.archive.org/web/20221205213858/https://www.choosingwisely.org/societies/american-association-of-neurological-surgeons-and-congress-of-neurological-surgeons
Several guidelines recommend, or suggest consideration of, CT head imaging for anticoagulated patients after minor head injury, regardless of symptoms.[67]American College of Emergency Physicians. Mild Traumatic Brain Injury. May 2023 [internet publication].
https://www.acep.org/patient-care/clinical-policies/mild-traumatic-brain-injury2
[80]Vos PE, Alekseenko Y, Battistin L, et al. Mild traumatic brain injury. Eur J Neurol. 2012 Feb;19(2):191-8.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1468-1331.2011.03581.x
http://www.ncbi.nlm.nih.gov/pubmed/22260187?tool=bestpractice.com
However, the supporting evidence base is limited.[80]Vos PE, Alekseenko Y, Battistin L, et al. Mild traumatic brain injury. Eur J Neurol. 2012 Feb;19(2):191-8.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1468-1331.2011.03581.x
http://www.ncbi.nlm.nih.gov/pubmed/22260187?tool=bestpractice.com
[81]Fuller GW, Evans R, Preston L, et al. Should adults with mild head injury who are receiving direct oral anticoagulants undergo computed tomography scanning? A Systematic Review. Ann Emerg Med. 2019 Jan;73(1):66-75.
https://www.annemergmed.com/article/S0196-0644(18)30652-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/30236417?tool=bestpractice.com
If initial CT shows no hemorrhage and no other criteria are met for extended monitoring, routine admission or observation is not indicated after a minor head injury for patients who are taking anticoagulants or antiplatelet medications.[67]American College of Emergency Physicians. Mild Traumatic Brain Injury. May 2023 [internet publication].
https://www.acep.org/patient-care/clinical-policies/mild-traumatic-brain-injury2
The absence of CT abnormalities does not exclude structural damage.[2]Maas AIR, Menon DK, Manley GT, et al. Traumatic brain injury: progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022 Nov;21(11):1004-60.
https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(22)00309-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36183712?tool=bestpractice.com
Avoid ordering a brain MRI to evaluate an acute concussion unless more severe brain injury is suspected.[82]American Medical Society for Sports Medicine. Ten things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2022 [internet publication].
https://web.archive.org/web/20230323081534/https://www.choosingwisely.org/societies/american-medical-society-for-sports-medicine
Brain MRI should be obtained if there is suspicion of an intracerebral structural lesion or hematoma, and CT scan is negative. Studies report structural traumatic abnormalities on MRI, (performed 2-3 weeks after injury) in approximately 30% of patients with mild TBI who had a normal CT on presentation.[2]Maas AIR, Menon DK, Manley GT, et al. Traumatic brain injury: progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022 Nov;21(11):1004-60.
https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(22)00309-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36183712?tool=bestpractice.com
[26]Yue JK, Yuh EL, Korley FK, et al. Association between plasma GFAP concentrations and MRI abnormalities in patients with CT-negative traumatic brain injury in the TRACK-TBI cohort: a prospective multicentre study. Lancet Neurol. 2019 Oct;18(10):953-61.
http://www.ncbi.nlm.nih.gov/pubmed/31451409?tool=bestpractice.com
[27]Steyerberg EW, Wiegers E, Sewalt C, et al. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: a European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019 Oct;18(10):923-34.
http://www.ncbi.nlm.nih.gov/pubmed/31526754?tool=bestpractice.com
Advanced MRI techniques, such as diffusion tensor imaging and susceptibility weighted imaging are more sensitive than standard MRI at detecting superficial contusions, traumatic axonal injury and traumatic vascular injury.[2]Maas AIR, Menon DK, Manley GT, et al. Traumatic brain injury: progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022 Nov;21(11):1004-60.
https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(22)00309-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36183712?tool=bestpractice.com
[83]Amyot F, Arciniegas DB, Brazaitis MP, et al. A review of the effectiveness of neuroimaging modalities for the detection of traumatic brain injury. J Neurotrauma. 2015 Nov 15;32(22):1693-721.
http://www.ncbi.nlm.nih.gov/pubmed/26176603?tool=bestpractice.com
[84]Sandsmark DK, Bashir A, Wellington CL, et al. Cerebral microvascular injury: a potentially treatable endophenotype of traumatic brain injury-induced neurodegeneration. Neuron. 2019 Aug 7;103(3):367-79.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6688649
http://www.ncbi.nlm.nih.gov/pubmed/31394062?tool=bestpractice.com
Fast MRI is feasible and accurate relative to CT in clinically stable children, in whom exposure to ionizing radiation may otherwise be a concern.[85]Lindberg DM, Stence NV, Grubenhoff JA, et al. Feasibility and accuracy of fast MRI versus CT for traumatic brain injury in young children. Pediatrics. 2019 Oct;144(4):e20190419.
https://pediatrics.aappublications.org/content/144/4/e20190419.long
http://www.ncbi.nlm.nih.gov/pubmed/31533974?tool=bestpractice.com
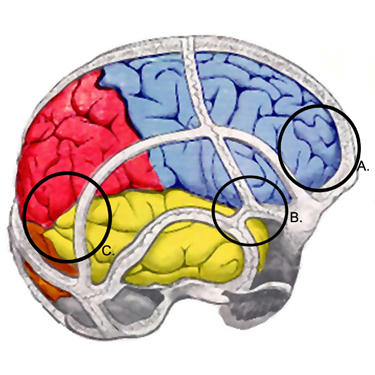
The most common structural changes observed are cerebral contusions; less common observations include epidural hematomas, subdural hematomas, and axonal injury.[Figure caption and citation for the preceding image starts]: Sites of contusions and epidural hematomas: (A) prefrontal cortex, (B) pterion, (C) temporal-parietal cortex (often during contre-coup)From the collection of L. Henry; used with permission [Citation ends].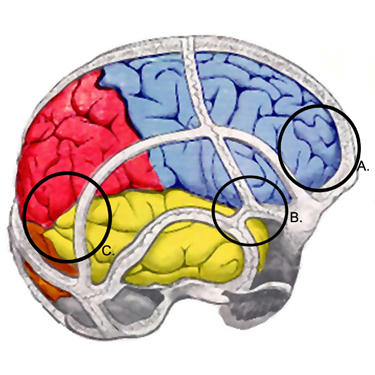
Alternative and emerging imaging modalities
Positron emission tomography (PET), single-photon emission CT [SPECT], magnetic resonance spectroscopy, and diffusion tensor imaging have yielded promising results that provide valuable insights into the pathophysiology of concussion, but are not yet recommended outside of a research setting.[86]Kutcher JS, McCrory P, Davis G, et al. What evidence exists for new strategies or technologies in the diagnosis of sports concussion and assessment of recovery? Br J Sports Med. 2013 Apr;47(5):299-303.
http://www.ncbi.nlm.nih.gov/pubmed/23479488?tool=bestpractice.com
It is noteworthy that both PET and SPECT have been used to demonstrate clinical changes in those patients with persistent symptomatology in the form of hypoperfused brain areas.[87]Umile EM, Sandel ME, Alavi A, et al. Dynamic imaging in mild traumatic brain injury: support for the theory of medial temporal vulnerability. Arch Phys Med Rehabil. 2002 Nov;83(11):1506-13.
http://www.ncbi.nlm.nih.gov/pubmed/12422317?tool=bestpractice.com
[88]Chen SH, Kareken DA, Fastenau PS, et al. A study of persistent post-concussion symptoms in mild head trauma using positron emission tomography. J Neurol Neurosurg Psychiatry. 2003 Mar;74(3):326-32.
http://www.ncbi.nlm.nih.gov/pubmed/12588917?tool=bestpractice.com
[89]Bonne O, Gilboa A, Louzoun Y, et al. Cerebral blood flow in chronic symptomatic mild traumatic brain injury. Psychiatry Res. 2003 Nov 30;124(3):141-52.
http://www.ncbi.nlm.nih.gov/pubmed/14623066?tool=bestpractice.com
[90]Abu-Judeh HH, Parker R, Singh M, et al. SPET brain perfusion imaging in mild traumatic brain injury without loss of consciousness and normal computed tomography. Nucl Med Commun. 1999 Jun;20(6):505-10.
http://www.ncbi.nlm.nih.gov/pubmed/10451861?tool=bestpractice.com
Newer, advanced multimodal MRI technologies (e.g., diffusion tensor imaging, resting state functional MRI, quantitative susceptibility imaging, magnetic resonance spectrography, and arterial spin labeling) are being studied in research protocols aimed at understanding the neurobiologic effects of, and recovery after, mild TBI.[3]Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019 Feb;53(4):213-25.
https://bjsm.bmj.com/content/53/4/213.long
http://www.ncbi.nlm.nih.gov/pubmed/30705232?tool=bestpractice.com