Tests
1st tests to order
multidetector computed tomography (MDCT)
Test
Noncontrast, MDCT is the initial imaging modality of choice to evaluate the cervical spine.[14]
More effective than x-ray for evaluation of cervical spine alignment, possibility of fracture, or soft-tissue swelling. The cervical spine is imaged from the skull base or craniocervical junction, through the cervicothoracic junction. Thinner slices increase sensitivity but may add to the radiation burden. Contiguous axial slices of no greater than 3 mm are recommended to obtain reformatted images in axial, coronal, and sagittal planes in the cervical spine.[14][30]
The main limitation of CT rests in its relative inability to detect changes in soft tissues, including the spinal cord and ligamentous structures.[14] Despite the high sensitivity of the MDCT in identifying bony abnormalities, interpretation may be difficult in patients with severe degenerative changes or osteopenia.[14]
In obtunded or intubated patients, the use of CT alone is sufficient to exclude unstable cervical spine injuries.[36]
Result
may show cervical spine vertebral misalignment, fracture, and prevertebral soft-tissue swelling
Tests to consider
CT whole spine
Test
If a cervical spine injury or a fracture is identified, a CT scan of the whole spine is indicated to identify a concomitant thoracolumbosacral fracture.[11] See Thoracolumbar spine trauma.
Result
may be normal; may show a concomitant thoracolumbosacral fracture
cervical spine x-ray series
Test
CT is now considered the primary imaging modality to evaluate the cervical spine.[14] Plain radiographs of the cervical and thoracolumbar spine are not recommended in the initial screening of spinal trauma because of their low sensitivity.[14] Multiple randomized control trials with Class I evidence now consider plain radiography to be insufficient to identify clinically relevant fractures.[14][31][32][33][34][35]
In the absence of CT, plain x-rays remain effective at evaluating for cervical spine misalignment, and prevertebral soft-tissue measurements. Views in this series include anteroposterior, lateral, open-mouth odontoid, and swimmer's (pull down) view.
All levels between the occiput and upper half of T1 need to be visualized. If this cannot be accomplished on a lateral view, a lateral swimmer's or pulldown view is required.
Anteroposterior and lateral views are useful at evaluating for misalignment, and prevertebral soft-tissue thickening. An open-mouth odontoid view can be used to assess for fractures of the dens or for transverse ligament injury. Ligamentous injury should be suspected if the combined overhang of the C1 lateral masses on C2 is >7 mm.[Figure caption and citation for the preceding image starts]: Normal cervical spine: lateral, AP, and open-mouth odontoid viewFrom the personal collection of Michael G. Fehlings [Citation ends].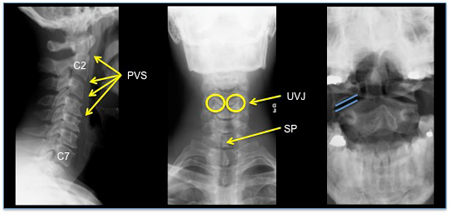
Result
may show cervical spine vertebral misalignment, fracture, prevertebral soft-tissue swelling, suspected transverse ligament injury
MRI cervical spine
Test
MRI is complementary to CT in the assessment of cervical spinal injuries.[14] It has high sensitivity for the identification of soft-tissue injuries and is considered the reference standard in identifying injuries to the spinal cord and discoligamentous complex.[14] It is the only modality for evaluating the internal structure of the spinal cord.[56] Caution should be taken when interpreting MRI results as the specificity for identifying significant soft-tissue injuries is shown to be only modest. Therefore, clinical correlation is of essence in each patient scenario.[40] MRI is not reliable in the identification of osseous injuries.
MRI is recommended in the following clinical scenarios: patients with clinical or imaging findings suggesting mechanically unstable cervical spine or ligamentous disruption; patients with neurologic deficit, suspected spinal cord injury or nerve root injury; comatose patients with normal CT of the cervical spine, to assess for possible ligamentous injury; and patients with normal CT of the cervical spine with persistent neck pain/tenderness, to assess for possible ligamentous injury.[39]
AOSpine guidelines suggest that when feasible, and as long as there are no contraindications, MRI should be used in spinal cord injury patients prior to surgical intervention to improve clinical decision making and to predict the neurologic outcome.[41] Patients on ventilator support, with hemodynamic instability or who are unable to remain still for prolonged periods of time often require help from an anesthesiologist for adequate sedation.
Result
may show cervical disk herniation, anterior or posterior ligament disruption, cord compression, spinal canal compromise, and intramedullary T1- and/or T2-weighted hyperintensity and/or hypointensity
CT myelogram
Test
CT myelogram can be used for the evaluation of spinal cord or nerve compression in the setting of cervical spinal trauma. Although considered to be inferior and technically more challenging to perform, CT myelogram provides an alternative for individuals with contraindication for MRI or when it is unavailable.
Result
May show spinal canal compromise, spinal cord compression secondary to disc herniation, hematoma, bony fragments, etc.
CT angiography (CTA) and MR angiography (MRA)
Test
CTA and MRA can be used in individuals with suspected arterial injury secondary to cervical spine trauma. Although both modalities were found to be inferior to catheter angiography, they were largely comparable in their ability in identifying all the clinically significant arterial injuries.[42][43][44][45][46]
CTA exposes the individual to adverse effects of intravenous contrast, therefore this technique should be used only in patients with high suspicion of arterial injury.[39]
Result
May show evidence of vascular injury, arterial dissection, pseudoaneurysm, stenosis, occlusion, transection, intramural hematoma, thrombus, etc.
flexion-extension (F/E) cervical spine x-rays
Test
F/E x-rays are contraindicated in cases of spinal cord injury, particularly if there is evidence of cord compression.
Useful for identifying the presence of dynamic instability in the presence of cervical spine ligamentous injury.
Patient undergoes lateral cervical spine x-rays at greatest possible neck flexion and greatest possible extension. Any subluxation of one vertebral body relative to an adjacent one by more than 3 mm signifies the possibility of dynamic instability and raises concern for ligamentous injury.
This should only be performed on a fully conscious patient capable of voluntary neck flexion and extension.
F/E x-rays may be performed in a patient with a normal cervical CT and no neurological deficits but with persistent neck pain/midline tenderness. In this case, normal F/E x-rays rule out ligamentous injury and cervical spine precautions can be discontinued.
However, in the acute traumatic setting, the range of motion of the neck may be restricted due to pain and muscle spasm, and the visualization of the cervical spine on lateral x-ray may be suboptimal. Hence, the result of F/E x-ray needs to be interpreted with caution and carefully correlated clinically.[37]
Result
subluxation of one vertebral body relative to an adjacent one by more than 3 mm
nerve conduction studies
Test
Ordered if radiculopathy is suspected. Slowing of nerve conduction occurs with peripheral nerve compression.
Result
slowing of nerve conduction velocity
electromyography
Test
Ordered if radiculopathy is suspected. Results require interpretation by a neurologist. However, do not order electromyography for isolated neck pain after a motor vehicle accident.[57] If neck pain is not associated with arm pain, arm tingling, arm weakness, or arm numbness, electromyography does not improve outcomes.[57]
Result
radiculopathy: altered S potentials and insertion potential
Use of this content is subject to our disclaimer