Etiology
A dangerous mechanism of injury is a strong risk factor for cervical spine injury; a fall from a height of greater than one 1 meter or 5 steps, axial loading injury to the head (e.g., falls, diving accidents, and nontraffic motorized vehicle collision [snowmobiles or all-terrain vehicles]).[10][11]
Vehicle accidents are the most common cause of cervical spine injuries. The injury mechanism commonly referred to as a whiplash injury occurs most often in rear-impact collisions, although it can occur in any type of collision.[12] Momentary hyperextension of the spine produces peak rotational forces, most often at the C5-C6 level (although all segments of the cervical spine can be injured), resulting in a unique facet injury mechanism at this level, in which the articulating surface of the upper segment is jammed into that of the lower segment.[13] The unique whiplash injury mechanism results in cervical spine flexion, compression, extension, distraction, and shear, all in less than one fifth of a second.[13]
Older adults are more susceptible to spinal injuries due to their increased risk for low velocity falls, and the increasingly likely presence of underlying conditions (e.g., osteoporosis and osteopenia, ankylosing spondylitis, and diffuse idiopathic skeletal hyperostosis), which may render the spine highly unstable even after a minor injury.[14] The upper cervical spine is the most common injury location for spinal fractures in older adults.[14][15]
Violent assaults are an increasingly common mechanism of cervical spine injury.[8] Blunt assault rarely results in cervical spine injury, although the risk increases with age ≥55 years.[16] High energy penetrating injuries (e.g., gunshot wounds) are at much greater risk of cervical spine injury than low velocity penetrating injuries (e.g., stab wounds).[14][17]
Pathophysiology
Injuries to the cervical spine can involve a variety of tissues: facet joints, disks and disk endplates, and cervical spine ligaments such as the posterior longitudinal ligament and ligamentum flavum. Occasionally a nerve root or the spinal cord will be injured immediately, but more typically inflammatory processes are set in motion by the initial injury. Persistent injury may produce alterations in pain thresholds throughout the body, mediated by pain-processing changes in the spinal cord and brain, a process known as centrally mediated pain or central sensitization. Muscles may be injured acutely, but may also be a source of pain in chronic cases, as injured muscles can develop trigger points and give rise to myofascial pain syndromes secondarily to other painful injury elsewhere in the spine.[18]
Injury to the cervical spine can be characterized based on:
Location within the spine (e.g., craniocervical junction, atlantoaxial, and subaxial)
Forces applied to the spine (e.g., flexion injuries, extension injuries)
Resulting fracture patterns (e.g., facet dislocation, fracture dislocation injury)
While a detailed description of cervical spine injuries taking into account each of these three characteristics is beyond the scope of this topic, the common fracture patterns are listed here: upper and subaxial spine fractures, plus a more detailed overview of motor vehicle accidents - perhaps the most common cause of cervical spine injury.
Common fracture patterns in the upper cervical spine are:
Occipital condyle fractures
Jefferson fractures and other atlas (C1) fractures, including fractures of the lateral mass
Atlantoaxial dislocation
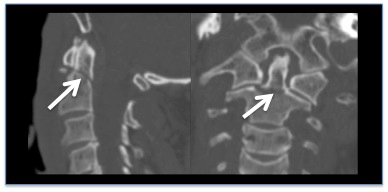
Fractures of C2: hangman fractures (spondylolisthesis of C2), odontoid fractures, and lateral body fractures[Figure caption and citation for the preceding image starts]: CT reconstruction demonstrating undisplaced odontoid fractureFrom the personal collection of Michael G. Fehlings [Citation ends].
Common fracture patterns in the lower cervical spine are:
Clay-shoveler fracture
Simple wedge compression fracture
Bilateral facet dislocation
Flexion teardrop fracture
Classification
Odontoid dens fracture
The Anderson and D'Alonzo classification links the height of the line through the odontoid process with prognosis:[1]
Type I: fracture of the upper part of the odontoid dens
Type II: fracture at the base of the odontoid dens
Type III: fracture affecting the body of the axis.
Hangman fracture
Traumatic spondylolisthesis of the axis is known as the hangman fracture.
The Levine and Edwards classification divides traumatic spondylolisthesis of the axis into 4 types:[2]
Type I: fracture without an angular deviation and translational deviation of <3.5 mm, which occurs due to hyperextension and axial compression
Type II: fracture with a significant translational or angular deviation, which occurs due to hyperextension and axial compression combined with a mechanism of flexion-compression
Type IIa: fracture with a small translational deviation and wide angulation, with an increase in posterior disk space between C2-C3 upon application of traction, which occurs due to a flexion-distraction
Type III: fracture with a large translational and angular deviation, which is associated with unilateral or bilateral dislocation of the C2-C3 joint facets and occurs due to a flexion-compression mechanism.
AOSpine subaxial cervical spine injury classification system[3]
A morphology-based classification system for clinical and research purposes.The AOSpine subaxial cervical spine injury classification system characterizes injury morphology, mechanism of injury, integrity of facets, and neurological status. AOSpine Injury Classification System Opens in new window These criteria (and additional modifiers believed to be important in the management of cervical spine injuries) can be combined using standardized nomenclature to succinctly convey complex information about a patient’s injury pattern.
Lower cervical spine fractures
A classification tool has been derived by expert consensus and validated for intra- and inter-rater reliability.[3] Injuries are assessed by four criteria: 1) morphology, 2) associated facet injury, 3) neurologic status, and 4) case-specific modifiers. Morphology is divided into A) compression injuries, B) tension-band injuries, and C) translational injuries. Each category is further subclassified as:
Morphology
Type A - compression injuries
A0: No bony or minor injury
A1: Single endplate fracture; posterior vertebral wall spared
A2: Both endplates fractured; posterior vertebral wall spared
A3: Single endplate fracture involving posterior vertebral wall
A4: Both endplates fractured involving posterior vertebral wall
Type B - tension-band injuries
B1: Predominately bony posterior tension-band injury
B2: Complete disruption of posterior capsuloligamentous or bony-capsuloligamentous structures
B3: Anterior tension-band injury
Type C - Translational injuries
C: Displacement or translation of vertebral body relative to another in any direction
Facet injury
F1: Not displaced; fragment <1 cm; <40% lateral mass involved
F2: Displaced or fragment >1 cm or >40% lateral mass involved
F3: Floating lateral mass (complete bony disconnection)
F4: Subluxed/perched/dislocated facet (inferior articular process of rostral vertebra rests on or anterior to superior articular process of caudal vertebra).
Neurology
N0: Intact
N1: Transient deficit completely resolved at time of assessment
N2: Radiculopathy
N3: Incomplete spinal cord injury (spared function below injury)
N4: Complete spinal cord injury (no spared function below injury)
NX: Undetermined
+ Designates ongoing compression.
Modifiers
M1: Partial posterior capsuloligamentous injury
M2: Critical disk herniation (extruded nucleus pulposus)
M3: Spine-stiffening disease (i.e., diffuse idiopathic skeletal hyperostosis, ankylosing spondylitis, ossification of the posterior longitudinal ligament, and ossification of the ligamentum flavum)
M4: Vertebral artery injury.
Use of this content is subject to our disclaimer