Tests
1st tests to order
CBC
Test
Test evaluates for presence of underlying immunosuppression. Duration of neutropenia correlates with increase in risk. Lymphopenia may not be as important a risk factor as neutropenia.[47]
Result
neutropenia, lymphopenia
basic metabolic profile
Test
Performed in patients with diabetes mellitus to look for metabolic acidosis. These help assess the severity of diabetic ketoacidosis.
Result
in patients with diabetes mellitus may see increased anion gap acidosis, hyperglycemia
ABG
Test
Evaluates the severity of acidosis in diabetic ketoacidosis. However, the disease can occur in the absence of acidosis.[48]
Result
low pH in diabetic ketoacidosis
urinalysis
Test
Positive dipstick confirms presence of ketones in urine. However, it does not diagnose diabetic ketoacidosis.
Result
positive for ketones in diabetic ketoacidosis
serum ketone level
Test
Carried out if urinary ketones are positive.
Result
positive in diabetic ketoacidosis
CT sinuses and brain
Test
Diffuse mucosal thickening without air-fluid levels is an early sign in mucormycosis. Bony destruction is usually a late finding.[49]
CT of the sinuses is less sensitive than MRI in demonstrating soft-tissue invasion. CT of the brain may not be able to differentiate between abscesses and early infarcts.[49]
Result
mucosal thickening, bony erosions, venous sinus thrombosis, abscesses, infarcts
MRI sinuses and brain
Test
If the infection is suspected to have spread to the eye or brain, MRI is preferred over CT due to its significantly higher sensitivity.[12] MRI delineates soft-tissue invasion into orbital tissues and cavernous sinus thrombosis. Provides better differentiation between abscess and infarcts, and information on posterior fossa involvement.
Result
soft tissue involvement of the orbital tissues, venous sinus thrombosis, abscesses, infarcts
CT chest with contrast
Test
CT chest with intravenous contrast is a sensitive test to detect abnormalities in pulmonary mucormycosis.[43] In one study, chest radiographs did not reveal any pathology in 53% of patients, all of whom had abnormalities on CT chest.[44]
Air crescent sign is more commonly seen in aspergillosis on recovery of neutropenia.[43]
Result
neutropenic patients: nodules with/without halo sign, reversed halo sign (early); hypodense sign, multiple nodules (1 week); pleural effusions, cavitation (≥2 weeks). Other patients (solid organ transplant recipients, intensive care unit patients, patients with diabetes): consolidation, masses, nodules, bronchial wall thickening with tree-in-bud nodules (early); hypodense sign (1 week); cavitation (≥2 weeks)
nasal endoscopy
Test
Essential to establish diagnosis with biopsy on suspicion of rhino-orbito-cerebral disease, because radiologic findings lag behind invasion.[3]
Result
necrotic mucosa
gastrointestinal endoscopy
Test
Gastrointestinal mucormycosis is infrequently diagnosed ante mortem owing to its rarity. In one case report, upper endoscopy revealed a plaque-like ulcer with necrotic slough.[52]
Result
mucosal ulcers, necrotic mucosa
Tests to consider
bronchoscopy with bronchoalveolar lavage and/or transbronchial biopsy fungal culture
Test
Literature on utility of bronchoalveolar lavage (BAL) in diagnosing pulmonary mucormycosis is scarce. The disease was diagnosed in 5 of 5 patients, 2 of these by cytology of BAL fluid alone and 3 by transbronchial biopsy.[50] Diagnosis by fungal culture on BAL or transbronchial specimens was poor (20%).[50]
Calcofluor white staining on early biopsy specimens from suspicious lesions can be useful in differentiating mucormycosis from aspergillosis.[51] Because sensitivity of cultures is limited, a specimen must be obtained for biopsy.
Result
demonstration of wide aseptate hyphae branching at 90° angle
histopathology of biopsy
Test
Biopsy specimens obtained at endoscopy, CT-guided fine needle aspiration biopsy, transbronchial biopsy, and open surgical methods (skin, lung) are key for suspecting mucormycosis.
Fungi are best observed by using special stains such as periodic acid Schiff or Gomori methenamine silver.[12][Figure caption and citation for the preceding image starts]: Methenamine silver stain demonstrating sparsely septate hyphae of Mucor pusillusFrom the CDC Public Health Image Library (PHIL): Dr Libero Ajello [Citation ends]. [Figure caption and citation for the preceding image starts]: Fluorescent antigen-stained Rhizopus arrhizusFrom the CDC Public Health Image Library (PHIL): Dr William Kaplan [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescent antigen-stained Rhizopus arrhizusFrom the CDC Public Health Image Library (PHIL): Dr William Kaplan [Citation ends].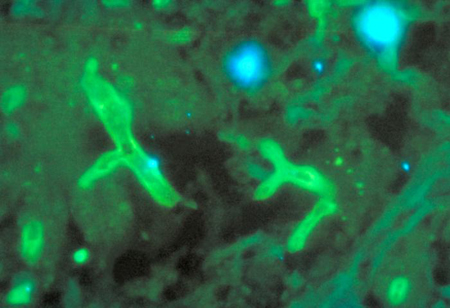
Angioinvasion with demonstration of broad, nonseptate hyphae is classically diagnostic; however, definitive diagnosis requires a positive fungal culture or molecular identification (where available).[12]
Result
nonseptate or minimally septate broad, ribbon-like hyphae (6-25 micrometers), branching at 90°
microbiology of biopsy
Emerging tests
polymerase chain reaction (PCR)
Test
PCR diagnosis, based on amplification of Mucorales-specific fungal genes (usually ribosomal DNA), has shown considerable promise, and is recommended in centers where it is available.[12] The CotH gene has emerged as a promising PCR target, demonstrating high sensitivity and specificity in animal models.[1] Commercial assays may also offer early diagnosis potential, often preceding culture positivity. However, the diagnostic yield of PCR from serum or whole blood remains variable.[1] Further clinical studies are required to better define the role of PCR in diagnosis of mucormycosis.
Result
positive for Mucorales
Use of this content is subject to our disclaimer