Mucormycosis infections progress rapidly and can be fatal without early diagnosis and prompt treatment. A high index of suspicion is crucial, particularly in immunosuppressed patients, and should be guided by clinical presentation, radiologic findings, histopathologic exam of the affected tissue, and recognition of presenting signs and symptoms.[38]Gupta MK, Kumar N, Dhameja N, et al. Laboratory diagnosis of mucormycosis: present perspective. J Family Med Prim Care. 2022 May;11(5):1664-71.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9254769
http://www.ncbi.nlm.nih.gov/pubmed/35800582?tool=bestpractice.com
Definitive diagnosis requires positive fungal culture or detection of fungal DNA through molecular testing (where available).[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
Molecular-based detection techniques are not yet fully standardized or commercially available; however, they show promise for improving the rapid and accurate diagnosis of mucormycosis.[4]Centers for Disease Control and Prevention. Mucormycosis: clinical overview of mucormycosis. Apr 2024 [internet publication].
https://www.cdc.gov/mucormycosis/hcp/clinical-overview/index.html
Recommended test availability may vary by region.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
Clinical presentation
Typical symptoms and signs of mucormycosis in a susceptible patient should be actively pursued. Risk factors include poorly-controlled diabetes mellitus with or without ketoacidosis, bone marrow or solid organ transplant, graft-versus-host disease, hematologic malignancy, corticosteroid therapy, iron overload, iron chelation therapy with deferoxamine, malnourishment, prematurity in newborns, burns, traumatic inoculation, and illicit drug use.
Rhino-orbito-cerebral disease commonly presents with facial pain; sinusitis, which may be accompanied by a viscid, dark brown or black nasal discharge; eye pain; blurred vision; and proptosis.[4]Centers for Disease Control and Prevention. Mucormycosis: clinical overview of mucormycosis. Apr 2024 [internet publication].
https://www.cdc.gov/mucormycosis/hcp/clinical-overview/index.html
Periorbital cellulitis is also common.[3]Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005 Jul;18(3):556-69.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195964
http://www.ncbi.nlm.nih.gov/pubmed/16020690?tool=bestpractice.com
Any of these clinical findings in a patient with diabetes mellitus necessitates prompt investigation for mucormycosis since the illness may be aggressive and can be fatal. Involvement of cranial nerves resulting in cranial nerve palsies is an ominous sign and indicates invasion into the central nervous system. Ophthalmoplegia commonly results from the spread of untreated infection from the ethmoid sinuses. Involvement of the contralateral eye signifies cavernous sinus thrombosis. Thrombosis of the internal carotid artery can lead to neurologic deficits and altered mental status. Necrotic eschar on the skin, palate, or nasal turbinates is common in the later stages of the infection.[4]Centers for Disease Control and Prevention. Mucormycosis: clinical overview of mucormycosis. Apr 2024 [internet publication].
https://www.cdc.gov/mucormycosis/hcp/clinical-overview/index.html
This appearance is due to thrombosis of the vessel by the invading fungus and subsequent tissue infarction.
Typically a dry cough (with or without dyspnea), fever, and chest pain are common symptoms in pulmonary mucormycosis.[4]Centers for Disease Control and Prevention. Mucormycosis: clinical overview of mucormycosis. Apr 2024 [internet publication].
https://www.cdc.gov/mucormycosis/hcp/clinical-overview/index.html
In patients with hematologic malignancies, initial respiratory symptoms are often attributed to invasive aspergillosis and usually treated with voriconazole or echinocandins, drugs not active against mucormycosis. However, persistence or worsening of symptoms should heighten suspicion of mucormycosis. Another clinical feature that may help differentiate pulmonary mucormycosis from aspergillosis is the higher incidence of accompanying sinus disease in mucormycosis.[39]Kontoyiannis DP, Lionakis MS, Lewis RE, et al. Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: a case-control observational study of 27 recent cases. J Infect Dis. 2005 Apr 15;191(8):1350-60.
http://jid.oxfordjournals.org/content/191/8/1350.full
http://www.ncbi.nlm.nih.gov/pubmed/15776383?tool=bestpractice.com
Hemoptysis can be massive and fatal. Death usually results from dissemination rather than respiratory failure in untreated cases except in hemoptysis. Overall mortality is high, 50% to 70%, and is more than 95% in disseminated disease.[3]Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005 Jul;18(3):556-69.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195964
http://www.ncbi.nlm.nih.gov/pubmed/16020690?tool=bestpractice.com
Cutaneous mucormycosis is usually a locally invasive disease, with nodules extending to the soft tissue, fascia, muscles, and even bone. This deep extension into the soft tissues and beyond occurs in about 44% of the patients with cutaneous disease.[40]Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005 Sep 1;41(5):634-53.
http://cid.oxfordjournals.org/content/41/5/634.full
http://www.ncbi.nlm.nih.gov/pubmed/16080086?tool=bestpractice.com
It usually presents in otherwise immunocompetent patients as a result of traumatic inoculation, dressings, or burns. Skin nodules are more common when skin is involved as a part of disseminated disease. Mortality can be over 80% in very locally invasive disease in an immunocompromised host without extensive surgery.[3]Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005 Jul;18(3):556-69.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195964
http://www.ncbi.nlm.nih.gov/pubmed/16020690?tool=bestpractice.com
Two types of cutaneous disease have been described: central and peripheral (involving only the extremities). Central cutaneous disease has a mortality of 32% compared with 15.5% in peripheral disease. This difference may be due to less immunosuppression and better ability to surgically control the disease in the case of peripheral disease.[41]Ledgard JP, van Hal S, Greenwood JE. Primary cutaneous zygomycosis in a burns patient: a review. J Burn Care Res. 2008 Mar-Apr;29(2):286-90.
http://www.ncbi.nlm.nih.gov/pubmed/18354283?tool=bestpractice.com
Gastrointestinal (GI) mucormycosis is a rare condition except in extremely malnourished people and premature neonates.[4]Centers for Disease Control and Prevention. Mucormycosis: clinical overview of mucormycosis. Apr 2024 [internet publication].
https://www.cdc.gov/mucormycosis/hcp/clinical-overview/index.html
An outbreak of GI mucormycosis was identified due to contamination of wooden tongue depressors used to mix nasogastric feeds.[3]Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005 Jul;18(3):556-69.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195964
http://www.ncbi.nlm.nih.gov/pubmed/16020690?tool=bestpractice.com
It presents with nonspecific symptoms of abdominal pain and distension, and GI bleeding. GI ulcers and subsequent perforation of the bowel can also occur, resulting in peritonitis.[3]Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005 Jul;18(3):556-69.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195964
http://www.ncbi.nlm.nih.gov/pubmed/16020690?tool=bestpractice.com
[42]Huang H, Xie L, Zheng Z, et al. Mucormycosis-induced upper gastrointestinal ulcer perforation in immunocompetent patients: a report of two cases. BMC Gastroenterol. 2021 Aug 3;21(1):311.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8370051
http://www.ncbi.nlm.nih.gov/pubmed/34404350?tool=bestpractice.com
GI mucormycosis is rapidly fatal and most commonly diagnosed post mortem.
Rapid clinical deterioration is a cause for alarm. Even in the presence of a presumptive diagnosis of mucormycosis and appropriate therapy, continued clinical assessment should be done to evaluate for any signs of dissemination of localized disease. Disseminated disease is involvement of 2 or more noncontiguous organ systems and/or positive blood cultures. Disseminated disease could manifest as nodular skin lesions or metastatic brain abscesses. The spleen, heart, skin, and other organs can also be affected.[4]Centers for Disease Control and Prevention. Mucormycosis: clinical overview of mucormycosis. Apr 2024 [internet publication].
https://www.cdc.gov/mucormycosis/hcp/clinical-overview/index.html
Laboratory
Routine blood work is rarely diagnostic of mucormycosis but may help in elucidating the underlying risk factor. Patients with diabetes mellitus should have blood chemistry, arterial blood gas, and urinary and serum ketones analyzed to detect the presence of metabolic acidosis. Patients with an underlying malignancy or suspected immunosuppression require a complete blood count to look for neutropenia.
Imaging
In the presence of compatible signs and symptoms in the appropriate susceptible host, imaging can be of great value in evaluating the extent of the disease and determining the accessibility of the lesion for imaging-guided biopsy or open surgical biopsy, and response to therapy. The choice of imaging depends on the site involved. Imaging can help in determining the extent of mucormycosis in a suspect case, but it cannot definitively diagnose the disease.
Patients with diabetes mellitus and sinusitis should have a computed tomography (CT) scan of the sinuses and brain.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
CT is less sensitive than magnetic resonance imaging (MRI) in detecting invasion into soft tissues but is more readily available and good for evaluating bony erosions. However, absence of bony erosions early in the disease course does not rule out mucormycosis. If the infection is suspected to have spread to the eye or brain, MRI is preferred over CT due to its significantly higher sensitivity.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
If sinusitis is diagnosed, endoscopy is recommended to diagnose mucormycosis.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
Patients with immunosuppression and respiratory symptoms or persistent fever should have a CT chest to assess for possible pulmonary mucormycosis.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
CT is far superior to plain radiographs in detecting the presence and extent of the disease.[43]Alexander BD, Lamoth F, Heussel CP, et al. Guidance on imaging for invasive pulmonary aspergillosis and mucormycosis: from the imaging working group for the revision and update of the consensus definitions of fungal disease from the EORTC/MSGERC. Clin Infect Dis. 2021 Mar 12;72(suppl 2):S79-88.
https://academic.oup.com/cid/article/72/Supplement_2/S79/6168275
http://www.ncbi.nlm.nih.gov/pubmed/33709131?tool=bestpractice.com
Typical findings include:[43]Alexander BD, Lamoth F, Heussel CP, et al. Guidance on imaging for invasive pulmonary aspergillosis and mucormycosis: from the imaging working group for the revision and update of the consensus definitions of fungal disease from the EORTC/MSGERC. Clin Infect Dis. 2021 Mar 12;72(suppl 2):S79-88.
https://academic.oup.com/cid/article/72/Supplement_2/S79/6168275
http://www.ncbi.nlm.nih.gov/pubmed/33709131?tool=bestpractice.com
For neutropenic patients:
At diagnosis: Nodules with/without halo sign; reversed halo sign
At 1 week: Hypodense sign; multiple nodules
At ≥2 weeks: Pleural effusions; cavitation
For other patients, including solid organ transplant recipients, patients under intensive care, and patients with diabetes mellitus:
At diagnosis: Consolidation, masses, nodules, bronchial wall thickening associated with tree-in-bud nodules
At 1 week: Hypodense sign
At ≥2 weeks: Cavitation
In patients with cutaneous mucormycosis, MRI is superior to CT scan in determining the extent of infection.[3]Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005 Jul;18(3):556-69.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195964
http://www.ncbi.nlm.nih.gov/pubmed/16020690?tool=bestpractice.com
[44]McAdams HP, Rosado de Christenson M, Strollo DC, et al. Pulmonary mucormycosis: radiologic findings in 32 cases. AJR Am J Roentgenol. 1997 Jun;168(6):1541-8.
http://www.ncbi.nlm.nih.gov/pubmed/9168721?tool=bestpractice.com
Patients with abdominal pain and risk factors for mucormycosis should have a CT scan. If there is evidence of colitis on CT scan or active GI bleeding, endoscopy with biopsy is indicated.
Microbiology
Fungal culture from clinical specimens is recommended, as it is more specific than imaging, can identify the agent at species level, and can inform antifungal susceptibility testing.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
Results may be affected by several factors:
Agents of mucormycosis in certain specimens, like sputum, could be laboratory contaminants but should never be dismissed in an immunocompromised patient.
Recovery of these fungi from blood, cerebrospinal fluid, wound swabs, and bronchoalveolar lavage (BAL) is not always successful, even in the presence of invasive disease.[41]Ledgard JP, van Hal S, Greenwood JE. Primary cutaneous zygomycosis in a burns patient: a review. J Burn Care Res. 2008 Mar-Apr;29(2):286-90.
http://www.ncbi.nlm.nih.gov/pubmed/18354283?tool=bestpractice.com
The best yield is from tissue cut into small pieces. Grinding of the specimen during certain procedures causes nonviability.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
Positive cultures are useful and diagnostic in the appropriate clinical setting. Negative cultures do not rule out infection.[7]Gonzalez CE, Rinaldi MG, Sugar AM. Zygomycosis. Infect Dis Clin North Am. 2002 Dec;16(4):895-914.
http://www.ncbi.nlm.nih.gov/pubmed/12512186?tool=bestpractice.com
Histopathology
Diagnosing mucormycosis based on histopathology alone is challenging. Definitive diagnosis requires a positive fungal culture or molecular identification (where available).[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
However, mucormycosis is classically suspected based on histopathologic findings.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
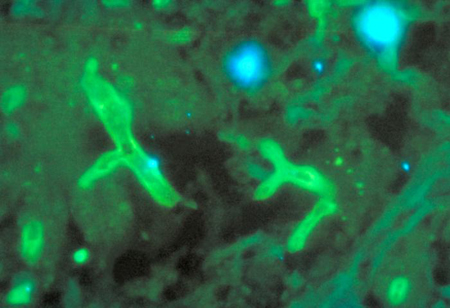
Mucorales species exhibit nonseptate or minimally septate broad, ribbon-like hyphae (6-25 micrometers) that branch at right angles and invade blood vessels in tissue specimens. However, due to tissue pressure and processing artefacts, branching angles can be difficult to assess, making hyphal width and irregular shape more reliable distinguishing features.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Methenamine silver stain demonstrating sparsely septate hyphae of Mucor pusillusFrom the CDC Public Health Image Library (PHIL): Dr Libero Ajello [Citation ends]. [Figure caption and citation for the preceding image starts]: Fluorescent antigen-stained Rhizopus arrhizusFrom the CDC Public Health Image Library (PHIL): Dr William Kaplan [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescent antigen-stained Rhizopus arrhizusFrom the CDC Public Health Image Library (PHIL): Dr William Kaplan [Citation ends].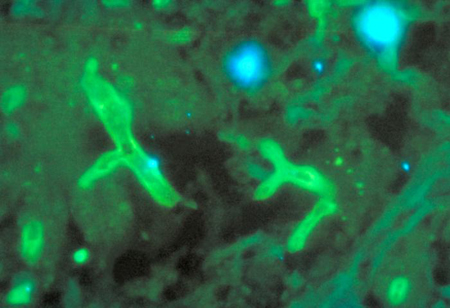
All patients should have an appropriate procedure to acquire a histologic diagnosis.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
However, biopsy may not be possible in patients with underlying hematologic disease due to thrombocytopenia.[45]Skiada A, Lanternier F, Groll AH, et al. Diagnosis and treatment of mucormycosis in patients with hematological malignancies: guidelines from the 3rd European Conference on Infections in Leukemia (ECIL 3). Haematologica. 2013 Apr;98(4):492-504.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3659979
http://www.ncbi.nlm.nih.gov/pubmed/22983580?tool=bestpractice.com
In such patients, a combination of high clinical suspicion with a positive culture, when obtained, should be sufficient information to treat the mycoses.
Specimens can be obtained by:
Emerging tests
Diagnostic tools outside of culture and histopathology are improving.
Molecular techniques are useful in diagnosing mucormycosis, particularly in the absence of standardized tests, and are recommended in centers where they are available.[12]Cornely OA, Alastruey-Izquierdo A, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019 Dec;19(12):e405-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8559573
http://www.ncbi.nlm.nih.gov/pubmed/31699664?tool=bestpractice.com
Fresh clinical material is preferred due to DNA degradation in formalin-fixed tissues.[1]Pham D, Howard-Jones AR, Sparks R, et al. Epidemiology, modern diagnostics, and the management of mucorales infections. J Fungi (Basel). 2023 Jun 12;9(6):659.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10304757
http://www.ncbi.nlm.nih.gov/pubmed/37367595?tool=bestpractice.com
Molecular assays such as polymerase chain reaction (PCR) have shown promise for detecting Mucorales DNA in culture-negative specimens. The CotH gene has emerged as a promising PCR target, demonstrating high sensitivity and specificity in animal models.[1]Pham D, Howard-Jones AR, Sparks R, et al. Epidemiology, modern diagnostics, and the management of mucorales infections. J Fungi (Basel). 2023 Jun 12;9(6):659.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10304757
http://www.ncbi.nlm.nih.gov/pubmed/37367595?tool=bestpractice.com
Commercial assays may also offer early diagnosis potential, often preceding culture positivity. However, the diagnostic yield of PCR from serum or whole blood remains variable.[1]Pham D, Howard-Jones AR, Sparks R, et al. Epidemiology, modern diagnostics, and the management of mucorales infections. J Fungi (Basel). 2023 Jun 12;9(6):659.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10304757
http://www.ncbi.nlm.nih.gov/pubmed/37367595?tool=bestpractice.com
Further clinical studies are required to better define the role of PCR in diagnosis of mucormycosis.
Galactomannan and (1-3)-beta-D-glucan are not helpful in diagnosing mucormycosis.[1]Pham D, Howard-Jones AR, Sparks R, et al. Epidemiology, modern diagnostics, and the management of mucorales infections. J Fungi (Basel). 2023 Jun 12;9(6):659.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10304757
http://www.ncbi.nlm.nih.gov/pubmed/37367595?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Fluorescent antigen-stained Rhizopus arrhizusFrom the CDC Public Health Image Library (PHIL): Dr William Kaplan [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescent antigen-stained Rhizopus arrhizusFrom the CDC Public Health Image Library (PHIL): Dr William Kaplan [Citation ends].