Tests
1st tests to order
CBC with differential
Test
Anemia can be due to blood loss or anemia of chronic disease.
Thrombocytopenia occurs due to bone marrow involvement.
Result
may show anemia and/or thrombocytopenia
blood smear
Test
Microcytosis and hypochromasia are features of anemia due to chronic blood loss.
Anemia of chronic disease presents with normal red cell indices.
Result
red cell morphology may be hypochromic, microcytic or normochromic, normocytic
comprehensive metabolic panel (including LFTs)
serum lactate dehydrogenase (LDH)
serum beta-2 microglobulin
Test
Provides an indirect indication of the proliferative rate of the lymphoma (i.e., disease activity), and should be measured as part of the initial workup to guide diagnosis and prognosis.[14]
Rarely elevated in MALT lymphoma.
Result
may be elevated
upper GI endoscopy
Test
Should be performed if gastric MALT lymphoma is suspected.[4][23]
The endoscopic appearance of gastric MALT lymphoma mimics chronic gastritis and peptic ulcer; therefore, endoscopic biopsy is essential to confirm the diagnosis of gastric MALT lymphoma.
Result
may show features of chronic gastritis or peptic ulcer
biopsy of affected site
Test
Tissue biopsy specimens should be obtained from abnormal- and normal-appearing areas of an affected site, wherever possible.[14][23] Multiple biopsies may be required if disease is multifocal (e.g., stomach, skin). Fine-needle aspiration biopsy should be avoided, as this may not provide an adequate specimen for diagnosis.
Histopathologic and immunophenotypic analysis of the biopsy specimens should be carried out to establish a diagnosis.[23] It should be noted that gastric MALT lymphoma preferentially spreads to the splenic marginal zone, where it can remain undetected by conventional histopathologic techniques.[32]
The morphologic features of MALT lymphoma are generally the same across anatomic sites.[34] There may be certain site-specific differences; for example, in gastric and salivary/parotid gland MALT lymphoma, lymphoepithelial lesions may develop due to neoplastic cells infiltrating the epithelium.[34] This is usually absent (or inconspicuous) in intestinal and conjunctival MALT lymphoma.
High-grade transformation of MALT lymphoma is characterized by the presence of increased numbers of transformed blast cells with the phenotype of a diffuse large B-cell lymphoma. These cases should be formally diagnosed as DLBCL, and the presence of accompanying MALT lymphoma should be noted.[5]
[Figure caption and citation for the preceding image starts]: Infiltrate of lymphoid cells in the lung, confirming their B-cell origin (CD20 staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Lung MALT lymphoma: residual respiratory epithelium has been distorted by infiltrating lymphocytes; the lymphoepithelial lesion (cytokeratin staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Lung MALT lymphoma: residual respiratory epithelium has been distorted by infiltrating lymphocytes; the lymphoepithelial lesion (cytokeratin staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].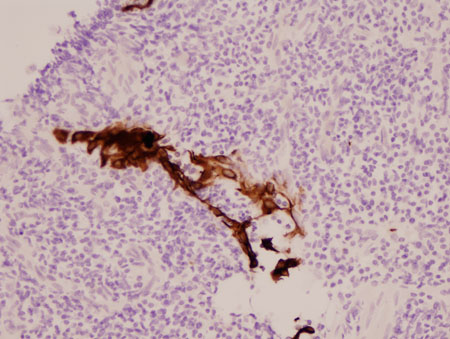 [Figure caption and citation for the preceding image starts]: Gastric MALT lymphoma: infiltration of the gastric epithelium by neoplastic B-lymphocytes (CD20 staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Gastric MALT lymphoma: infiltration of the gastric epithelium by neoplastic B-lymphocytes (CD20 staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].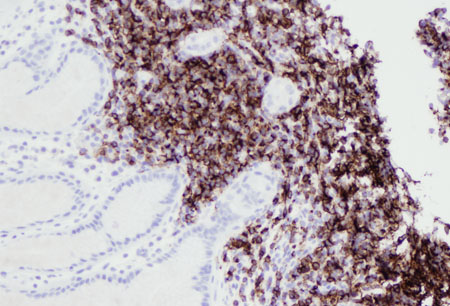 [Figure caption and citation for the preceding image starts]: Lung MALT lymphoma: lung parenchyma has been replaced by a neoplastic infiltrate of small lymphocytes; a follicle surrounded by neoplastic marginal zone cells can be recognized in the center of the image (hematoxylin and eosin [H&E] staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Lung MALT lymphoma: lung parenchyma has been replaced by a neoplastic infiltrate of small lymphocytes; a follicle surrounded by neoplastic marginal zone cells can be recognized in the center of the image (hematoxylin and eosin [H&E] staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].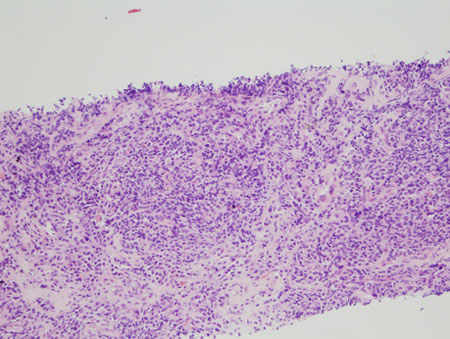 [Figure caption and citation for the preceding image starts]: Gastric MALT lymphoma: normal gastric epithelium distorted by a neoplastic infiltrate of lymphocytes extending into the superficial gastric epithelium (hematoxylin and eosin [H&E] staining, × 200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Gastric MALT lymphoma: normal gastric epithelium distorted by a neoplastic infiltrate of lymphocytes extending into the superficial gastric epithelium (hematoxylin and eosin [H&E] staining, × 200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].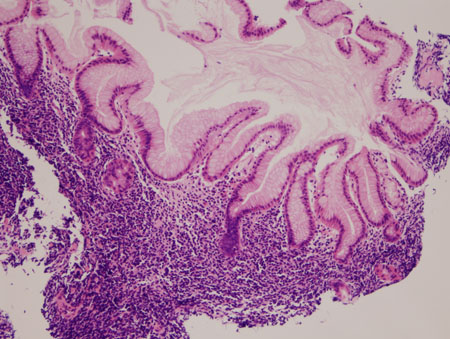
Result
infiltration of the lymphoma cells around the reactive B-cell follicles outside the preserved mantle zone in a marginal zone distribution, and extending into the interfollicular region; lymphoepithelial lesions may be present (e.g., in gastric and salivary/parotid gland MALT lymphoma biopsy)
immunophenotyping
Test
Immunohistochemistry (with or without flow cytometry) of the biopsy specimens should be carried out to identify tumor markers to confirm a diagnosis.[23]
Result
typical immunophenotype for MALT lymphoma: CD5-, CD10-, CD20+, CD23-/+, CD43-/+, cyclin D1-, with BCL2- follicles
H pylori (histologic testing)
Test
Histologic testing (immunohistochemical staining) for Helicobacter pylori infection should be carried out on biopsy specimens if gastric MALT lymphoma is suspected.[23]
In advanced gastric MALT lymphoma with extensive infiltration of the gastric wall, H pylori can be difficult to demonstrate on histologic specimens.[33]
Result
may identify H pylori infection
CT scan
Test
CT scan (contrast enhanced) of the neck, chest, abdomen, and pelvis should be carried out in all patients for staging and assessing treatment response.[14][23]
CT scan of the salivary/parotid glands should be ordered if there are symptoms or signs of salivary gland involvement.
Approximately 25% of patients with nongastric MALT lymphoma present with disseminated disease (including advanced-stage).[8]
Result
may identify nodal or extranodal involvement
Tests to consider
H pylori (stool antigen test)
Test
Indicated in cases of gastric MALT lymphoma if Helicobacter pylori infection is not confirmed histologically.[23]
Result
may be positive for H pylori
H pylori (urea breath test)
Test
Indicated in cases of gastric MALT lymphoma if Helicobacter pylori infection is not confirmed histologically.[23]
Result
may be positive for H pylori
H pylori (serology test)
PCR testing for infectious agents
Test
PCR testing for Chlamydia psittaci, Campylobacter jejuni, and Borrelia burgdorferi may be done on biopsy specimens if nongastric MALT lymphoma is suspected.[4][14]
C psittaci infection is associated with ocular adnexal MALT lymphoma.[14]
C jejuni infection is associated with intestinal MALT lymphoma (including immunoproliferative small intestinal disease).[14]
B burgdorferi infection is associated with skin/cutaneous MALT lymphoma.[14]
Result
may identify C psittaci, C jejuni, or B burgdorferi
bone marrow biopsy with aspirate
Test
Helpful in determining bone marrow involvement, and important for staging of the disease.
The bone marrow aspirate should be sent for morphology and immunophenotyping, and the trephine biopsy should be sent for histology, immunohistochemistry, and genetic studies.
Result
may detect lymphoma
genetic studies
Test
Cytogenetic (e.g., fluorescence in situ hybridization [FISH] and karyotype) and/or molecular (e.g., PCR) evaluation of biopsy samples should be considered to detect cytogenetic abnormalities associated with MALT lymphoma.[4][18][23]
t(11;18) is mainly detected in gastric and lung MALT lymphoma. Patients with gastric MALT lymphoma who are t(11;18)-positive are unlikely to be positive for Helicobacter pylori infection and unlikely to respond to H pylori-eradication therapy.[25][26]
t(14;18) is detected in liver, skin, lung, and ocular adnexa MALT lymphoma.
t(3;14) is detected in thyroid, ocular adnexa, and skin MALT lymphoma.
t(1;14) is detected in gastric and lung MALT lymphoma.
Other cytogenetic abnormalities that may be detected in MALT lymphoma include trisomy 3 and trisomy 18.[35]
Result
may show t(11;18), t(14;18), t(3;14), t(1;14), trisomy 3, trisomy 18
immunoglobulin gene rearrangement studies
Test
Molecular testing for immunoglobulin gene rearrangement may help distinguish malignant (clonal) lymphoma from benign (polyclonal) conditions (e.g., hyperplasia, chronic inflammation).
In some cases monoclonality can be demonstrated in uncomplicated chronic gastritis, and this may precede the emergence of gastric MALT lymphoma.[39][40]
Result
may detect clonal immunoglobulin gene rearrangement
MYD88 mutation testing
Test
Molecular testing for MYD88 mutation may help distinguish MALT lymphoma (with plasmacytic differentiation) from Waldenström macroglobulinemia.
The MYD88 mutation is common in Waldenström macroglobulinemia (over 90%), but uncommon in MALT lymphoma.[41]
Result
negative
serum protein electrophoresis
Test
Serum protein electrophoresis should be considered because a paraprotein may be detected if there is plasmacytic differentiation, which occurs in around one third of patients.[5][23]
Serum protein electrophoresis can also be used to monitor the disease.[Figure caption and citation for the preceding image starts]: Lung MALT lymphoma: parts of this tumor demonstrate striking plasmacytic differentiation (CD138 staining, ×200)From the collections of Dr R. Joshi and Dr C. McNamara; used with permission [Citation ends].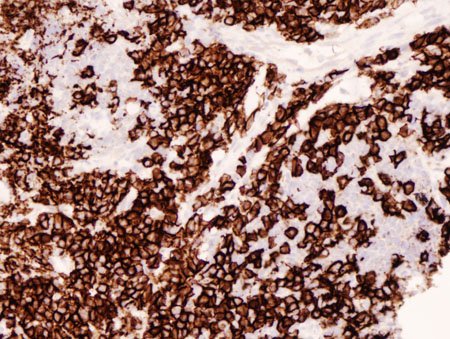
Result
may be positive for a paraprotein
18F-fluorodeoxyglucose (FDG) PET/CT scan
Test
May be useful for tumor staging and assessing treatment response.[36][37][38]
FDG-PET/CT scans may have higher sensitivity and specificity than CT scan alone, but can lead to false-negative findings due to the low metabolic rate of MALT lymphoma.[30][36]
Result
may identify nodal or extranodal involvement
endoscopic ultrasound of the stomach
Test
Endoscopic ultrasound of the stomach can be used for staging of gastric MALT lymphoma.
It is particularly useful for evaluating gastric wall infiltration (depth of invasion) and regional lymph node involvement.[4][23][30]
Result
may show gastric wall infiltration and thickening; may show lymph node involvement
lower GI endoscopy
Test
Although the stomach and small intestine are more commonly involved than the large intestine, the latter can be affected. Staging endoscopy of the entire GI tract should, therefore, be considered.[4]
Result
may show polyps, ulcers, nodular lesions, or mucosal discoloration
MRI orbit, brain
mammography
breast ultrasound
MRI breast
thyroid ultrasound
bronchoscopy
hepatitis C serology
Test
There is an association between hepatitis C and nongastric MALT lymphoma (e.g., liver).[14]
If serology is positive, then further testing by PCR to determine viral load is indicated.
Result
usually negative; may be positive
hepatitis B serology
Test
There is an association between hepatitis B and nongastric MALT lymphoma (e.g., liver).[14]
Hepatitis B status should be determined prior to treatment due to risk of virus reactivation during chemotherapy and/or immunosuppressive therapy.
Result
usually negative; may be positive
HIV serology
Test
There is a weak association between HIV and nongastric MALT lymphomas (e.g., lung).[14]
Result
usually negative; may be positive
multigated acquisition (MUGA) scan
Test
Should be ordered to assess cardiac function prior to commencing anthracycline-based treatment.[23]
Result
baseline cardiac function
echocardiography
Test
Should be ordered to assess cardiac function prior to commencing anthracycline-based treatment.[23]
Result
baseline cardiac function
Use of this content is subject to our disclaimer