Approach
Transient synovitis is a self-limited inflammatory disorder of the hip that commonly affects young children. It is part of the differential diagnosis for a limping child with coxalgia (pain in or disease of the hip or hip joint). The immediate concern is ruling out septic arthritis, which is one of the few true orthopedic emergencies. A delay in treatment of septic arthritis can have devastating consequences, with near-total destruction of the hip.[7][8]
History
Often presents acutely as mild to moderate hip pain, which gradually improves, but the child may have periods of relative comfort intermixed with discomfort.[1] There may be a recent history of the child having an upper respiratory illness or gastrointestinal illness in the past but they will be currently healthy.[6] The child should be able to ambulate (although may have an aversion to walking) and typically will have a limp. The child may choose not to bear weight. A history of recent antibiotic or antipyretic use may be important to identify masking of an underlying infection such as septic arthritis.
Physical exam
The child will often rest their hip in abduction and external rotation. Hip motion may be limited, but the patient will usually allow movement through a limited arc of motion or micromotion. Restriction of motion may be particularly apparent in abduction and internal rotation. However, some patients may not display any restriction in hip movement. There may be pain on hip movement, even with passive movement, and there may be tenderness on palpation of the hip or groin.
The log roll is the most sensitive test for transient synovitis of the hip. In this exam, the patient lies supine and the leg is rolled gently from side to side. A positive test results in involuntary muscle guarding in the affected limb.
In an orthopedic exam, the joints above and below the affected joint should be examined as well as the contralateral joint. The femur bone may also be palpated to assess for osteomyelitis or other periarticular infection. Exam of the pelvis and knee should always be included to rule out pathology affecting these joints. In transient synovitis, exam of the pelvis and knee should be normal.
Laboratory tests
There are no identifying laboratory tests, although complete blood count, erythrocyte sedimentation rate, and C-reactive protein may be slightly elevated.
Four independent clinical predictors have been identified to differentiate between septic arthritis and transient synovitis. In transient synovitis, fever should be <101.3°F (<38.5°C), the child may limp but should be able to bear weight, erythrocyte sedimentation rate should be well under 40 mm/hour, and serum white blood cell count <12,000 cells/mm³. If all of the above criteria are met, the predicted probability of septic arthritis is <0.2% for zero predictors, and 3.0% for one predictor.[9][10][11] C-reactive protein over 2.0 mg/dL (>20 mg/L) is a strong independent predictor of septic arthritis of the hip.[8][12]
Radiographs
Radiographs of transient synovitis of the hip are typically normal; however, they may reveal subtle signs early in the disease process, such as capsular distention, joint space widening, diminution of the definition of soft tissue planes around the hip joint, or slight demineralization of the bone of the proximal femur.[13] The primary role of plain radiographs is ruling out other disorders, such as Legg-Calvé-Perthes disease, fractures, and tumors, and ensuring that the metaphyseal bone of the femur and acetabulum do not have signs of other processes such as osteomyelitis.[14][Figure caption and citation for the preceding image starts]: Radiograph of a 5-year-old child with an irritable right hip showing subtle signs early in the disease process, such as capsular distention, joint space widening, and diminution of the definition of soft-tissue planes around the hip joint or slight demineralization of the bone of the proximal femurFrom the collection of J. McCarthy [Citation ends].
Ultrasound
An effusion is a common finding.[15] Ultrasound is not typically used for the evaluation of transient synovitis but is quick, painless, imparts no ionizing radiation, and can detect an effusion in nearly all of the established cases. The specificity of a hip joint effusion on ultrasound is low, and unfortunately the finding is not specific for septic arthritis, but the absence of an effusion does make septic arthritis unlikely, except very early in the disease process. Ultrasound can also be useful for guiding needle aspiration if septic arthritis has to be excluded.[13] If septic arthritis is being considered as a differential diagnosis, joint aspiration should be performed and fluid sent for cell count and culture/Gram stain.[16] Joint aspiration is the first choice for diagnosing septic arthritis and may be helpful in distinguishing between transient synovitis of the hip and septic arthritis in select cases.[Figure caption and citation for the preceding image starts]: Ultrasound of a hip documenting a hip effusionFrom the collection of J. McCarthy [Citation ends].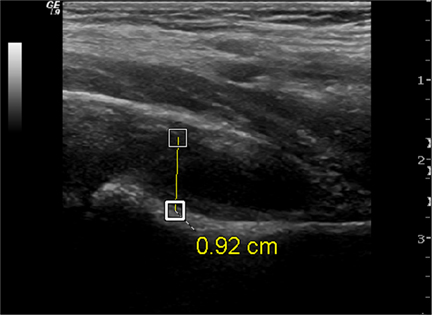
Magnetic resonance imaging (MRI)
The main role of contrast-enhanced MRI is to rule out other disorders including coexisting osteomyelitis in the proximal femur or pelvis, especially if the patient does not respond to treatment.[13] It is typically not employed for the diagnosis of transient synovitis.[17][18] MRI should not be ordered for a child until all appropriate clinical, laboratory, and plain radiographic exams have been completed, unless there is concern for infection.[13][14][19]
Use of this content is subject to our disclaimer