Approach
Definitive diagnosis of Hirschsprung disease is established histologically by a rectal biopsy demonstrating the absence of ganglion cells, but this is typically not the first diagnostic test. A careful history and physical exam can help determine which patients warrant further workup. Contrast enemas and anorectal manometry are also useful adjuncts in establishing the diagnosis.
History and physical exam
The classical presentation of Hirschsprung disease is the full-term neonate who does not pass meconium within the first 48 hours of life. Most patients are diagnosed in the neonatal period.[1] A patient who presents later in life may have chronic symptoms of constipation, encopresis, feeding difficulties, and/or faltering growth.[47] A family history of Hirschsprung disease is reported in about 8% of patients.[44]
The most common signs of Hirschsprung disease are:
Abdominal distension
Vomiting
Delayed passage of meconium (past the first 24-48 hours of life)
Explosive passage of stool/gas
Constipation/obstipation
Faltering growth
Some patients may also present with signs and symptoms of Hirschsprung-associated enterocolitis (HAEC) which additionally include abdominal tenderness, fever, lethargy, diarrhea, bloody stool, and septic shock.[3][11] Severe HAEC can result in life-threatening sepsis and should be treated expeditiously as it is the leading cause of death in Hirschsprung disease.[11][12][13] Children with delayed diagnosis of Hirschsprung disease (older than 12 months of age) are less likely to present with HAEC.[47]
Imaging
A plain abdominal x-ray may show nonspecific signs of distal obstruction such as dilated intestines and air-fluid levels. There may be an absence of air in the lower pelvis. However, a normal film does not exclude the possibility of Hirschsprung disease.
[Figure caption and citation for the preceding image starts]: Abdominal x-ray image showing gaseous distension of the large bowel with air absent from the rectum (typical of Hirschsprung disease)BMJ Case Reports 2012; doi:10.1136/bmj.e5521 [Citation ends].
A contrast enema performed with water-soluble contrast material is the most valuable imaging test for Hirschsprung disease. A contrast enema is recommended if the clinical evaluation is suspicious for Hirschsprung disease or if there are signs of distal obstruction on x-ray. A rectosigmoid ratio (maximum diameter of the rectum divided by maximum diameter of the sigmoid colon during contrast enema) of <1 is highly suggestive of Hirschsprung disease. Other suggestive findings include retained contrast at >24 hours, mucosal irregularity, or microcolon.[48] A transition zone may be seen on contrast enema but this may be less obvious in neonates.[49] A transition zone on contrast enema can help with surgical planning, but it should be noted that the radiographic transition zone may not correlate with the histologic transition zone.[50] Contrast enema may demonstrate mucosal irregularity in the aganglionic distal colon and may show a transition zone between smaller caliber aganglionic distal colon and dilated proximal ganglionic colon.[Figure caption and citation for the preceding image starts]: Barium enema performed in a newborn with Hirschsprung disease. Often, classical changes are not obvious in the neonatal periodCorman ML. Colon and rectal surgery. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2005:555-603; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Contrast enema showing an abnormal rectosigmoid ratio (sigmoid diameter larger than rectal diameter)From the personal collection of Lily Cheng, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Contrast enema showing an abnormal rectosigmoid ratio (sigmoid diameter larger than rectal diameter)From the personal collection of Lily Cheng, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Contrast enema may demonstrate mucosal irregularity in the aganglionic distal colon and may show a transition zone between smaller caliber aganglionic distal colon and dilated proximal ganglionic colonFrom the personal collection of Lily Cheng, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Contrast enema may demonstrate mucosal irregularity in the aganglionic distal colon and may show a transition zone between smaller caliber aganglionic distal colon and dilated proximal ganglionic colonFrom the personal collection of Lily Cheng, MD; used with permission [Citation ends].
Rectal biopsy
A rectal biopsy is always necessary for definitive diagnosis of Hirschsprung disease. Biopsies should be obtained at least 2 cm proximal to the dentate line and should be at least 3 mm in diameter, ensuring that at least one third of the sample includes submucosal tissue.[27] Rectal biopsies can be performed using either suction or open surgical techniques, with a preference for the least invasive feasible method.[27] A traditional full-thickness rectal biopsy includes both the myenteric and submucosal plexuses and is performed under general anesthesia in the operating room. A suction rectal biopsy can be done at the bedside without sedation, but includes the submucosal plexus only. This may yield inadequate specimen in the older infant or child.[51] Bleeding and perforation are rare complications.[52]
Rectal biopsy pathology will show an absence of ganglion cells in Hirschsprung disease. It may also show the presence of hypertrophic nerves (greater than 40 micrometers in an infant less than 6 months), but this may be absent in patients with long-segment disease or total colonic aganglionosis (TCA).[53] Other immunohistochemical stains including calretinin, choline transporter, and acetylcholinesterase may be useful ancillary markers.[53][54]
[Figure caption and citation for the preceding image starts]: Hematoxylin and eosin showing ganglion cells in the myenteric plexusFrom the personal collection of Lily Cheng, MD; used with permission [Citation ends].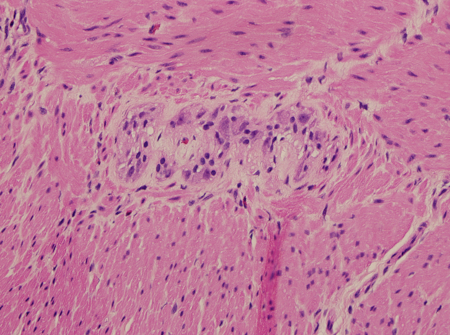
Anorectal manometry
Anorectal manometry may be helpful in older children as a screening test to identify patients who warrant rectal biopsy. A normal recto-anal inhibitor reflex (RAIR) on anorectal manometry has a negative predictive value of up to 100%.[55] An absent RAIR on manometry should be followed by a biopsy to confirm the diagnosis of Hirschsprung disease.
Use of this content is subject to our disclaimer