The definitive method for the diagnosis of meningioma is with clinical history and physical exam followed by magnetic resonance imaging (MRI) with and without gadolinium-contrast enhancement.[43]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: central nervous system cancers [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425
[44]American College of Radiology. ACR appropriateness criteria: brain tumors. 2024 [internet publication].
https://acsearch.acr.org/docs/3195155/Narrative
[45]Szychot E, Goodden J, Whitfield G, et al. Children's Cancer and Leukaemia Group (CCLG): review and guidelines for the management of meningioma in children, teenagers and young adults. Br J Neurosurg. 2020 Apr;34(2):142-53.
http://www.ncbi.nlm.nih.gov/pubmed/32116043?tool=bestpractice.com
Increasingly, meningiomas are identified incidentally when imaging the neuro-axis for unrelated reasons.
History and physical exam
A thorough history should be undertaken in all patients with a suspected primary brain tumor. Signs and symptoms of meningiomas are generally nonspecific but may include:[46]Magill ST, Young JS, Chae R, et al. Relationship between tumor location, size, and WHO grade in meningioma. Neurosurg Focus. 2018 Apr;44(4):E4.
https://thejns.org/focus/view/journals/neurosurg-focus/44/4/article-pE4.xml
http://www.ncbi.nlm.nih.gov/pubmed/29606048?tool=bestpractice.com
New onset headache, cranial nerve deficit, and seizure are among the most common findings, occurring in up to 37%, 31%, and 17% of patients with meningioma, respectively; this symptom history should prompt an imaging evaluation of the patient for a potential brain tumor, especially with advancing age.[46]Magill ST, Young JS, Chae R, et al. Relationship between tumor location, size, and WHO grade in meningioma. Neurosurg Focus. 2018 Apr;44(4):E4.
https://thejns.org/focus/view/journals/neurosurg-focus/44/4/article-pE4.xml
http://www.ncbi.nlm.nih.gov/pubmed/29606048?tool=bestpractice.com
[47]Kernick DP, Ahmed F, Bahra A, et al. Imaging patients with suspected brain tumour: guidance for primary care. Br J Gen Pract. 2008 Dec;58(557):880-5.
http://bjgp.org/content/58/557/880
http://www.ncbi.nlm.nih.gov/pubmed/19068162?tool=bestpractice.com
The history should also establish risk factors for meningioma including: exposure to radiation or exogenous hormones, history of breast cancer, and genetic predisposition (i.e., family history of brain tumor or neurofibromatosis 2).[6]Withrow DR, Anderson H, Armstrong GT, et al. Pooled analysis of meningioma risk following treatment for childhood cancer. JAMA Oncol. 2022 Dec 1;8(12):1756-64.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9539736
http://www.ncbi.nlm.nih.gov/pubmed/36201196?tool=bestpractice.com
[25]Hemminki K, Li X, Collins VP. Parental cancer as a risk factor for brain tumors (Sweden). Cancer Causes Control. 2001 Apr;12(3):195-9.
http://www.ncbi.nlm.nih.gov/pubmed/11405324?tool=bestpractice.com
[26]Antinheimo J, Sankila R, Carpen O, et al. Population-based analysis of sporadic and type 2 neurofibromatosis-associated meningiomas and schwannomas. Neurology. 2000 Jan 11;54(1):71-6.
http://www.ncbi.nlm.nih.gov/pubmed/10636128?tool=bestpractice.com
[29]Lopez-Rivera V, Zhu P, Dono A, et al. Increased risk of subsequent meningioma among women with malignant breast cancer. World Neurosurg. 2020 Jul;139:e271-85.
http://www.ncbi.nlm.nih.gov/pubmed/32298823?tool=bestpractice.com
[34]Claus EB, Black PM, Bondy ML, et al. Exogenous hormone use and meningioma risk: what do we tell our patients? Cancer. 2007 Aug 1;110(3):471-6.
http://onlinelibrary.wiley.com/doi/10.1002/cncr.22783/full
http://www.ncbi.nlm.nih.gov/pubmed/17580362?tool=bestpractice.com
[35]Korhonen K, Raitanen J, Isola J, et al. Exogenous sex hormone use and risk of meningioma: a population-based case-control study in Finland. Cancer Causes Control. 2010 Dec;21(12):2149-56.
http://www.ncbi.nlm.nih.gov/pubmed/20730482?tool=bestpractice.com
Both a general exam and a detailed neurologic exam should be undertaken. Specific neurologic deficits, such as cranial nerve, motor, or sensory deficits, should be evaluated and recorded, including the specific spinal level where deficits are localized to, as this will then direct level-specific imaging. Some cranial nerve deficits may require formal evaluation by a specialist for clinically accurate documentation.
Imaging
The diagnostic study of choice is MRI brain or spine with and without gadolinium enhancement.[43]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: central nervous system cancers [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425
[44]American College of Radiology. ACR appropriateness criteria: brain tumors. 2024 [internet publication].
https://acsearch.acr.org/docs/3195155/Narrative
[45]Szychot E, Goodden J, Whitfield G, et al. Children's Cancer and Leukaemia Group (CCLG): review and guidelines for the management of meningioma in children, teenagers and young adults. Br J Neurosurg. 2020 Apr;34(2):142-53.
http://www.ncbi.nlm.nih.gov/pubmed/32116043?tool=bestpractice.com
Radiographic findings of brain MRI that support a diagnosis of meningioma include: dural-based mass, homogeneously contrast-enhancing tumor, dural tail, and cerebrospinal fluid cleft.[43]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: central nervous system cancers [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425
Around half of all meningiomas are found at the skull base (anterior, middle, or posterior cranial fossa), with around 40% occurring at the convexity, falx, or parasagittal regions.[46]Magill ST, Young JS, Chae R, et al. Relationship between tumor location, size, and WHO grade in meningioma. Neurosurg Focus. 2018 Apr;44(4):E4.
https://thejns.org/focus/view/journals/neurosurg-focus/44/4/article-pE4.xml
http://www.ncbi.nlm.nih.gov/pubmed/29606048?tool=bestpractice.com
Between 7% to 12% of all meningiomas occur at spinal sites.[48]Ogasawara C, Philbrick BD, Adamson DC. Meningioma: a review of epidemiology, pathology, diagnosis, treatment, and future directions. Biomedicines. 2021 Mar 21;9(3):319.
https://www.mdpi.com/2227-9059/9/3/319
http://www.ncbi.nlm.nih.gov/pubmed/33801089?tool=bestpractice.com
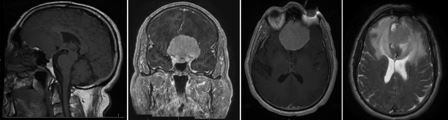
[Figure caption and citation for the preceding image starts]: Sagittal image (left) demonstrates large extra-axial mass isointense with brain. After contrast administration, the lesion avidly enhances, as shown in the coronal image (center left) and axial image (center right). Note the extensive edema surrounding the tumor on the T2 axial image (right)From the personal library of Dr William T. Couldwell; used with permission [Citation ends].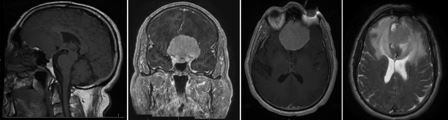
Computed tomography (CT) is indicated if concern exists about any bone involvement (e.g., loss of vision caused by hyperostosis around the optic nerve or involvement of the 8th cranial nerve) or if MRI is contraindicated (e.g., in patients with certain types of pacemakers or shrapnel/metal in their body). CT may add complementary information demonstrating hyperostosis associated with the tumor or calcifications, which may be present in a significant percentage of patients. Calcification within a meningioma usually indicates a slower-growing tumor.[49]Nakasu S, Fukami T, Nakajima M, et al. Growth pattern changes of meningiomas: long-term analysis. Neurosurgery. 2005 May;56(5):946-55.
http://www.ncbi.nlm.nih.gov/pubmed/15854242?tool=bestpractice.com
Cerebral angiography, although performed commonly in the past, is used less frequently for diagnosis in the era of contemporary MRI.[50]Goldbrunner R, Stavrinou P, Jenkinson MD, et al. EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol. 2021 Nov 2;23(11):1821-34.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8563316
http://www.ncbi.nlm.nih.gov/pubmed/34181733?tool=bestpractice.com
Occasionally, cerebral angiography will be performed to demonstrate the predominant arterial input to the tumor.[44]American College of Radiology. ACR appropriateness criteria: brain tumors. 2024 [internet publication].
https://acsearch.acr.org/docs/3195155/Narrative
It is also essential in surgical planning when the patency of major venous sinuses is in question.
Positron emission tomography (PET)/CT can be used to detect the somatostatin analogs DOTA-D-Phe1-Tyr3-octreotate (DOTATATE) or DOTA-D-Phe1-Tyr3-octreotide (DOTATOC) that are labeled with a radionuclide such as gallium-68, copper-64, or yttrium-90. Although not yet standard clinical practice, somatostatin receptor PET/CT can help confirm the diagnosis, or distinguish residual or recurrent tumors from postoperative scarring.[43]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: central nervous system cancers [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425
[50]Goldbrunner R, Stavrinou P, Jenkinson MD, et al. EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol. 2021 Nov 2;23(11):1821-34.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8563316
http://www.ncbi.nlm.nih.gov/pubmed/34181733?tool=bestpractice.com
[51]Prasad RN, Perlow HK, Bovi J, et al. (68)Ga-DOTATATE PET: the future of meningioma treatment. Int J Radiat Oncol Biol Phys. 2022 Jul 15;113(4):868-71.
https://linkinghub.elsevier.com/retrieve/pii/S0360-3016(22)00402-3
http://www.ncbi.nlm.nih.gov/pubmed/35772444?tool=bestpractice.com
It may also be useful in radiation planning to delineate the target volume.[44]American College of Radiology. ACR appropriateness criteria: brain tumors. 2024 [internet publication].
https://acsearch.acr.org/docs/3195155/Narrative
[52]Perlow HK, Siedow M, Gokun Y, et al. (68)Ga-DOTATATE PET-based radiation contouring creates more precise radiation volumes for patients with meningioma. Int J Radiat Oncol Biol Phys. 2022 Jul 15;113(4):859-65.
http://www.ncbi.nlm.nih.gov/pubmed/35460804?tool=bestpractice.com
[53]Hadi I, Biczok A, Terpolilli N, et al. Multimodal therapy of cavernous sinus meningioma: Impact of surgery and (68)Ga-DOTATATE PET-guided radiation therapy on tumor control and functional outcome. Neurooncol Adv. 2021 Jan-Dec;3(1):vdab114.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8541706
http://www.ncbi.nlm.nih.gov/pubmed/34704034?tool=bestpractice.com
Laboratory
There are no specific laboratory tests required to confirm a diagnosis of meningioma, or for preoperative planning, other than to confirm normal electrolytes and coagulation.
Where diagnosis is uncertain based on radiographic findings alone, surgical resection may be considered.[43]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: central nervous system cancers [internet publication].
https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425
Meningiomas have a wide range of appearances on histopathological analysis of the surgically resected tumor. The mitotic index may indicate a faster-growing tumor. There are significant differences in mitotic indices among tumor grades. The vast majority of meningiomas stain for epithelial membrane antigen (EMA) and somatostatin receptor 2A (SSTR2A), and vimentin positivity is found in all meningiomas. Diagnostic ultrastructural features include copious vimentin filaments, complex interdigitating cell processes, and desmosomal intercellular junctions.[54]Louis D, Scheithauer B, Budka H, et al. Meningiomas. In: Kleihues P, Cavenee W, editors. World Health Organization classification of tumours: pathology and genetics: tumours of the nervous system. Lyon, France: IARC Press, 2000.