Benign paroxysmal positional vertigo
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
initial presentation
patient education and reassurance
The initial step in managing BPPV is patient education and reassurance.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication]. https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv [42]Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005 Sep;26(5):1034-40. http://www.ncbi.nlm.nih.gov/pubmed/16151355?tool=bestpractice.com [43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010. This is done by explaining its non-life-threatening nature and favorable prognosis, with spontaneous remission in one third of patients at 3 weeks and the majority of patients at 6 months from onset.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93. http://www.cmaj.ca/content/169/7/681.full http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com [43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[68]White J, Savvides P, Cherian N, et al. Canalith repositioning for benign paroxysmal positional vertigo. Otol Neurotol. 2005 Jul;26(4):704-10. http://www.ncbi.nlm.nih.gov/pubmed/16015173?tool=bestpractice.com
Patients should be made aware that BPPV is a highly treatable condition, with the majority of episodes resolving after the administration of a single particle repositioning maneuver.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com [44]Helminski JO, Zee DS, Janssen I, et al. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010 May;90(5):663-78. https://academic.oup.com/ptj/article/90/5/663/2737747 http://www.ncbi.nlm.nih.gov/pubmed/20338918?tool=bestpractice.com [45]Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E, et al. Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo [in Spanish]. Neurologia. 2010 Jun;25(5):295-9. http://www.ncbi.nlm.nih.gov/pubmed/20643039?tool=bestpractice.com However, relapses and remissions can occur unpredictably in both treated and untreated patients.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com Patients who have secondary BPPV (e.g., secondary to vestibular neuronitis) should be encouraged to return to normal physical activity to facilitate central nervous system compensation.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.
3-position particle repositioning maneuver (PRM)
Treatment recommended for ALL patients in selected patient group
Contraindications to repositioning maneuvers include severe cervical disease, unstable cardiovascular disease, suspected vertebrobasilar disease, and high-grade carotid stenosis.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com For those patients without contraindications, the literature describes many minor variations of the PRM technique, but the 3-position PRM variant of the Epley maneuver is recommended.[54]Parnes LS, Price-Jones RG. Particle repositioning maneuver for benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1993 May;102(5):325-31. http://www.ncbi.nlm.nih.gov/pubmed/8489160?tool=bestpractice.com [91]Parnes LS, Robichaud J. Further observations during the particle repositioning maneuver for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1997 Feb;116(2):238-43. http://www.ncbi.nlm.nih.gov/pubmed/9051072?tool=bestpractice.com The PRM has a well documented short-term efficacy, with the majority of patients treated successfully after a single PRM attempt.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com [44]Helminski JO, Zee DS, Janssen I, et al. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010 May;90(5):663-78. https://academic.oup.com/ptj/article/90/5/663/2737747 http://www.ncbi.nlm.nih.gov/pubmed/20338918?tool=bestpractice.com [45]Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E, et al. Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo [in Spanish]. Neurologia. 2010 Jun;25(5):295-9. http://www.ncbi.nlm.nih.gov/pubmed/20643039?tool=bestpractice.com Postmaneuver instructions, including post-PRM postural restrictions, are not necessary.[59]Gordon CR, Gadoth N. Repeated vs single physical maneuver in benign paroxysmal positional vertigo. Acta Neurol Scand. 2004 Sep;110(3):166-9. http://www.ncbi.nlm.nih.gov/pubmed/15285773?tool=bestpractice.com [60]Devaiah AK, Andreoli S. Postmaneuver restrictions in benign paroxysmal positional vertigo: an individual patient data meta-analysis. Otolaryngol Head Neck Surg. 2010 Feb;142(2):155-9. http://www.ncbi.nlm.nih.gov/pubmed/20115966?tool=bestpractice.com [61]Toupet M, Ferrary E, Bozorg Grayeli A. Effect of repositioning maneuver type and postmaneuver restrictions on vertigo and dizziness in benign positional paroxysmal vertigo. ScientificWorldJournal. 2012;2012:162123. http://www.hindawi.com/journals/tswj/2012/162123 http://www.ncbi.nlm.nih.gov/pubmed/22973168?tool=bestpractice.com [62]Mostafa BE, Youssef TA, Hamad AS. The necessity of post-maneuver postural restriction in treating benign paroxysmal positional vertigo: a meta-analytic study. Eur Arch Otorhinolaryngol. 2013 Mar;270(3):849-52. http://www.ncbi.nlm.nih.gov/pubmed/22588196?tool=bestpractice.com
The procedure involves the following steps: [Figure caption and citation for the preceding image starts]: Particle-repositioning maneuver (right ear)Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003:169:681-693; used with permission [Citation ends].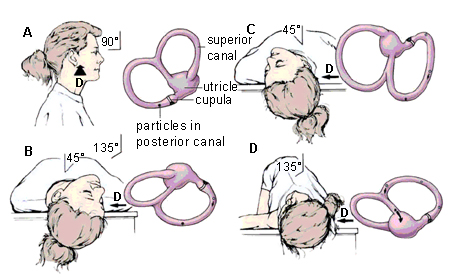
Place the patient in a sitting position at the end of the examination table.
Rotate the head 45° toward the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for primary stage nystagmus.
Maintain this position for 1-2 minutes.
The head is rotated 90° toward the opposite ear while maintaining the head hanging position.
Continue then to roll the whole patient another 90° toward the unaffected side until the head is facing 180° from the original Dix-Hallpike position. This change in position should take <3-5 seconds.
Observe for secondary-stage nystagmus. A favorable response occurs when the secondary-stage nystagmus is in the same direction as the primary-stage nystagmus, because the canalith particles would still be moving toward the utricle; an unfavorable response occurs when the nystagmus is in the opposite direction, which results when the particles regress away from the utricle toward its original position. Absence of nystagmus is not uncommon and may indicate mixed results, such as partial (incomplete) BPPV resolution.
Maintain the final position for 30-60 seconds, and then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful maneuver, because the particles will have been cleared from the posterior semicircular canal back into the utricle.
For horizontal canal and anterior canal BPPV, special maneuvers exist, but these patients should be referred to a specialist center.
vestibular suppressant medication (only useful in small subset of patients)
Treatment recommended for SOME patients in selected patient group
Medication is not an effective treatment for BPPV. The use of vestibular suppressant medications such as the benzodiazepines (lorazepam, diazepam) and antihistamines (meclizine, dimenhydrinate, promethazine) is not recommended in the vast majority of BPPV cases.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication]. https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv [48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com [49]McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980 Dec;9(6):472-7. http://www.ncbi.nlm.nih.gov/pubmed/6110782?tool=bestpractice.com [50]Fujino A, Tokumasu K, Yosio S, et al. Vestibular training for benign paroxysmal positional vertigo. Its efficacy in comparison with antivertigo drugs. Arch Otolaryngol Head Neck Surg. 1994 May;120(5):497-504. http://www.ncbi.nlm.nih.gov/pubmed/8172700?tool=bestpractice.com
Vestibular suppressant medications are not curative and are often ineffective at symptom management given the sudden and short-lived onset of BPPV.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Suppressants also produce unwanted adverse effects such as drowsiness. The central nervous system (CNS) suppression these drugs cause may result in disease prolongation by inhibiting central compensation for a coexisting vestibular loss: for example, in cases of BPPV secondary to vestibular neuronitis.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
There is, however, a small subpopulation of patients with prolonged autonomic dysfunction and imbalance who may benefit from vestibular suppressant medication (e.g., lorazepam or diazepam), but the CNS depressant adverse effects of these medications must be carefully weighed prior to initiating treatment.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Rarely, a small subset of patients become extremely nauseated and emetic during a repositioning maneuver, necessitating stopping the maneuver. Such individuals may benefit from a prophylactic antiemetic (e.g., meclizine, dimenhydrinate, promethazine) prior to subsequent maneuvers.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Primary options
lorazepam: 0.5 to 2 mg intravenously/intramuscularly every 4-8 hours when required; or 0.5 to 2 mg intravenously/intramuscularly as a single dose prior to repositioning maneuver
OR
diazepam: 2-10 mg orally/intravenously every 4-8 hours when required; or 2-10 mg orally/intravenously as single dose prior to repositioning maneuver
OR
meclizine: 12.5 to 25 mg orally every 4-8 hours when required, maximum 100 mg/day; or 12.5 to 25 mg orally as a single dose approximately 60 minutes prior to repositioning maneuver
OR
dimenhydrinate: 25-50 mg orally every 4-6 hours when required, maximum 400 mg/day; or 25-50 mg orally as a single dose approximately 30 minutes prior to repositioning maneuver
OR
promethazine: 12.5 to 25 mg orally/intravenously every 4-6 hours when required, maximum 100 mg/day; or 12.5 to 25 mg orally/intravenously as a single dose approximately 30-60 minutes prior to repositioning maneuver
vestibular rehabilitation exercises
Treatment recommended for SOME patients in selected patient group
Some patients may benefit from vestibular rehabilitation exercises to promote functional recovery and prevent recurrence, particularly if they are at higher risk of falls or have residual generalized dizziness after BPBPV treatment.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication]. https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv [70]McDonnell MN, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2015 Jan 13;(1):CD005397. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005397.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/25581507?tool=bestpractice.com Vestibular rehabilitation consists of home exercises or a customized program delivered by a therapist. Suitable home exercises include the modified self-Epley, modified Semont, and half somersault maneuvres.[71]Ismail EI, Morgan AE, Abdeltawwab MM. Home particle repositioning maneuver to prevent the recurrence of posterior canal BPPV. Auris Nasus Larynx. 2018 Oct;45(5):980-4. http://www.ncbi.nlm.nih.gov/pubmed/29526580?tool=bestpractice.com [72]Ranju RL, Lepcha A, Mammen MD, et al. An effective home-based particle repositioning procedure for posterior canal benign paroxysmal positional vertigo (BPPV). Indian J Otolaryngol Head Neck Surg. 2022 Dec;74(4):516-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9741680 http://www.ncbi.nlm.nih.gov/pubmed/36514424?tool=bestpractice.com [73]Foster CA, Ponnapan A, Zaccaro K, et al. A comparison of two home exercises for benign positional vertigo: half somersault versus Epley Maneuver. Audiology and Neurotology Extra. 2012 Apr 2020;2(1):16–23. https://karger.com/aue/article/2/1/16/44463/A-Comparison-of-Two-Home-Exercises-for-Benign [74]Radtke A, von Brevern M, Tiel-Wilck K, et al. Self-treatment of benign paroxysmal positional vertigo: Semont maneuver vs Epley procedure. Neurology. 2004 Jul 13;63(1):150-2. http://www.ncbi.nlm.nih.gov/pubmed/15249626?tool=bestpractice.com
Semont repositioning maneuver
Treatment recommended for ALL patients in selected patient group
Although the PRM and Semont maneuver share a similar mechanism and efficacy, the PRM is used preferentially by most clinicians in North America because it is more comfortable for the patient and simpler to perform, especially in overweight and older patients.[42]Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005 Sep;26(5):1034-40.
http://www.ncbi.nlm.nih.gov/pubmed/16151355?tool=bestpractice.com
[55]Salvinelli F, Trivelli M, Casale M, et al. Treatment of benign positional vertigo in the elderly: a randomized trial. Laryngoscope. 2004 May;114(5):827-31.
http://www.ncbi.nlm.nih.gov/pubmed/15126738?tool=bestpractice.com
[56]Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope. 1999 Apr;109(4):584-90.
http://www.ncbi.nlm.nih.gov/pubmed/10201745?tool=bestpractice.com
[57]Herdman SJ, Tusa RJ, Zee DS, et al. Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1993 Apr;119(4):450-4.
http://www.ncbi.nlm.nih.gov/pubmed/8457308?tool=bestpractice.com
[58]Mandalà M, Santoro GP, Asprella Libonati G, et al. Double-blind randomized trial on short-term efficacy of the Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. J Neurol. 2012 May;259(5):882-5.
http://www.ncbi.nlm.nih.gov/pubmed/22008871?tool=bestpractice.com
[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
If the PRM fails after repeated sessions, then the Semont (liberatory) maneuver is the next treatment option. The procedure involves the following steps: [Figure caption and citation for the preceding image starts]: Liberatory maneuver of Semont (right ear)Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003:169:681-693; used with permission [Citation ends].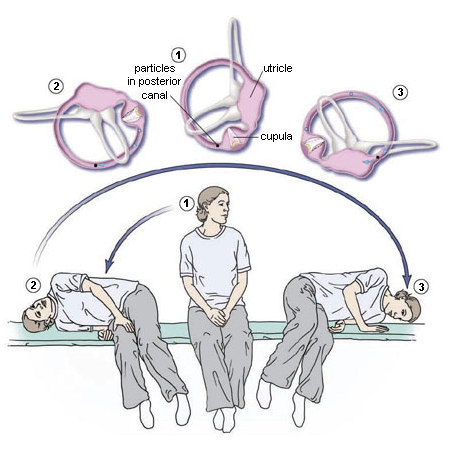
Sit the patient midway along the long side of an examination table, with their legs hanging over the edge.
Rotate the head 45° toward the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upward. This may induce nystagmus and vertigo because of particle movement toward the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1-2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downward. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1-2 minutes). Slowly return the patient to the sitting position of step 1.
vestibular suppressant medication (only useful in small subset of patients)
Treatment recommended for SOME patients in selected patient group
Medication is not an effective treatment for BPPV. The use of vestibular suppressant medications such as the benzodiazepines (lorazepam, diazepam) and antihistamines (meclizine, dimenhydrinate, promethazine) is not recommended in the vast majority of BPPV cases.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication]. https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv [48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com [49]McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980 Dec;9(6):472-7. http://www.ncbi.nlm.nih.gov/pubmed/6110782?tool=bestpractice.com [50]Fujino A, Tokumasu K, Yosio S, et al. Vestibular training for benign paroxysmal positional vertigo. Its efficacy in comparison with antivertigo drugs. Arch Otolaryngol Head Neck Surg. 1994 May;120(5):497-504. http://www.ncbi.nlm.nih.gov/pubmed/8172700?tool=bestpractice.com
Vestibular suppressant medications are not curative and are often ineffective at symptom management given the sudden and short-lived onset of BPPV.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Suppressants also produce unwanted adverse effects such as drowsiness. The The central nervous system (CNS) suppression these drugs cause may result in disease prolongation by inhibiting central compensation for a coexisting vestibular loss: for example, in cases of BPPV secondary to vestibular neuronitis.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
There is, however, a small subpopulation of patients with prolonged autonomic dysfunction and imbalance who may benefit from vestibular suppressant medication, but the CNS depressant adverse effects of these medications must be carefully weighed prior to initiating treatment.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Rarely, a small subset of patients become extremely nauseated and emetic during a repositioning maneuver, necessitating stopping the maneuver. Such individuals may benefit from an antiemetic vestibular suppressant (e.g., meclizine, promethazine) prior to subsequent maneuvers.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6. http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Primary options
lorazepam: 0.5 to 2 mg intravenously/intramuscularly every 4-8 hours when required; or 0.5 to 2 mg intravenously/intramuscularly as a single dose prior to repositioning maneuver
OR
diazepam: 2-10 mg orally/intravenously every 4-8 hours when required; or 2-10 mg orally/intravenously as single dose prior to repositioning maneuver
OR
meclizine: 12.5 to 25 mg orally every 4-8 hours when required, maximum 100 mg/day; or 12.5 to 25 mg orally as a single dose approximately 60 minutes prior to repositioning maneuver
OR
dimenhydrinate: 25-50 mg orally every 4-6 hours when required, maximum 400 mg/day; or 25-50 mg orally as a single dose approximately 30 minutes prior to repositioning maneuver
OR
promethazine: 12.5 to 25 mg orally/intravenously every 4-6 hours when required, maximum 100 mg/day; or 12.5 to 25 mg orally/intravenously as a single dose approximately 30-60 minutes prior to repositioning maneuver
vestibular rehabilitation exercises
Treatment recommended for SOME patients in selected patient group
Some patients may benefit from vestibular rehabilitation exercises to promote functional recovery and prevent recurrence, particularly if they are at higher risk of falls or have residual generalized dizziness after BPPV treatment.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication]. https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv [70]McDonnell MN, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2015 Jan 13;(1):CD005397. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005397.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/25581507?tool=bestpractice.com Vestibular rehabilitation consists of home exercises or a customized program delivered by a therapist. Suitable home exercises include the modified self-Epley, modified Semont, and half somersault maneuvres.[71]Ismail EI, Morgan AE, Abdeltawwab MM. Home particle repositioning maneuver to prevent the recurrence of posterior canal BPPV. Auris Nasus Larynx. 2018 Oct;45(5):980-4. http://www.ncbi.nlm.nih.gov/pubmed/29526580?tool=bestpractice.com [72]Ranju RL, Lepcha A, Mammen MD, et al. An effective home-based particle repositioning procedure for posterior canal benign paroxysmal positional vertigo (BPPV). Indian J Otolaryngol Head Neck Surg. 2022 Dec;74(4):516-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9741680 http://www.ncbi.nlm.nih.gov/pubmed/36514424?tool=bestpractice.com [73]Foster CA, Ponnapan A, Zaccaro K, et al. A comparison of two home exercises for benign positional vertigo: half somersault versus Epley Maneuver. Audiology and Neurotology Extra. 2012 Apr 2020;2(1):16–23. https://karger.com/aue/article/2/1/16/44463/A-Comparison-of-Two-Home-Exercises-for-Benign [74]Radtke A, von Brevern M, Tiel-Wilck K, et al. Self-treatment of benign paroxysmal positional vertigo: Semont maneuver vs Epley procedure. Neurology. 2004 Jul 13;63(1):150-2. http://www.ncbi.nlm.nih.gov/pubmed/15249626?tool=bestpractice.com
modified and specialized treatments
Treatment recommended for ALL patients in selected patient group
If repositioning maneuvres fail after repeat surgery visits, then prompt referral to a tertiary specialist dizziness clinic is indicated.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93. http://www.cmaj.ca/content/169/7/681.full http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
Patients with contraindications to repositioning maneuvers and those unable to tolerate repositioning maneuvers or exercises may benefit from vestibular habituation therapy under the supervision of a physical therapist.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.
For patients with cervical spine or other issues that limit neck extension, a 30° bed tilt during the PRM can avoid the need for neck extension. It should be noted that a 30° tilt is sufficient to cause the patient to slide down the bed. Thus, although most PRMs can be easily carried out by a solo clinician, a PRM with a 30° bed tilt will require at least one assistant.
A chair that can spin and position the patient in any plane in space without the need for neck movements is available.[75]Nakayama M, Epley JM. BPPV and variants: improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005 Jul;133(1):107-12. http://www.ncbi.nlm.nih.gov/pubmed/16025062?tool=bestpractice.com
multiple repositioning maneuvers and vestibular rehabilitation exercises ineffective
surgery
The vast majority of BPPV cases will respond to the repositioning maneuvers or resolve spontaneously. The surgical treatment of BPPV is reserved for unrelenting, incapacitating cases where repeated attempts with repositioning maneuvers and vestibular rehabilitation exercises have failed.[78]Walsh RM, Bath AP, Cullen JR, et al. Long-term results of posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol Allied Sci. 1999 Aug;24(4):316-23. http://www.ncbi.nlm.nih.gov/pubmed/10472467?tool=bestpractice.com [79]Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1990 May;99(5 Pt 1):330-4. http://www.ncbi.nlm.nih.gov/pubmed/2337310?tool=bestpractice.com Surgical treatment may also be considered for patients who respond to PRMs but have unremitting recurrences soon after, to the extent that they are eager for a definitive solution rather than repeated PRMs. Less than 1% of BPPV patients will ever require surgery, but because BPPV is so common, that number of surgical candidates is not negligible.[80]Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006 Mar;134(3):424-30. http://www.ncbi.nlm.nih.gov/pubmed/16500439?tool=bestpractice.com
Prior to surgery, all other diagnoses must be excluded and imaging of the posterior fossa is a prerequisite. There are two surgical procedures for BPPV: singular neurectomy and posterior canal occlusion. Posterior canal occlusion surgery is the recommended procedure and has been shown to be a highly efficacious, safe, and reproducible technique in numerous studies.[78]Walsh RM, Bath AP, Cullen JR, et al. Long-term results of posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol Allied Sci. 1999 Aug;24(4):316-23. http://www.ncbi.nlm.nih.gov/pubmed/10472467?tool=bestpractice.com [80]Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006 Mar;134(3):424-30. http://www.ncbi.nlm.nih.gov/pubmed/16500439?tool=bestpractice.com [81]Agrawal SK, Parnes LS. Human experience with canal plugging. Ann N Y Acad Sci. 2001 Oct;942:300-5. http://www.ncbi.nlm.nih.gov/pubmed/11710471?tool=bestpractice.com [82]Pace-Balzan A, Rutka JA. Non-ampullary plugging of the posterior semicircular canal for benign paroxysmal positional vertigo. J Laryngol Otol. 1991 Nov;105(11):901-6. http://www.ncbi.nlm.nih.gov/pubmed/1761943?tool=bestpractice.com [83]Dingle AF, Hawthorne MR, Kumar BU. Fenestration and occlusion of the posterior semicircular canal for benign positional vertigo. Clin Otolaryngol Allied Sci. 1992 Aug;17(4):300-2. http://www.ncbi.nlm.nih.gov/pubmed/1526046?tool=bestpractice.com [84]Hawthorne M, el-Naggar M. Fenestration and occlusion of posterior semicircular canal for patients with intractable benign paroxysmal positional vertigo. J Laryngol Otol. 1994 Nov;108(11):935-9. http://www.ncbi.nlm.nih.gov/pubmed/7829944?tool=bestpractice.com [85]Anthony PF. Partitioning the labyrinth for benign paroxysmal positional vertigo: clinical and histologic findings. Am J Otol. 1993 Jul;14(4):334-42. http://www.ncbi.nlm.nih.gov/pubmed/8238267?tool=bestpractice.com [86]Leveque M, Labrousse M, Seidermann L, et al. Surgical therapy in intractable benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2007 May;136(5):693-8. http://www.ncbi.nlm.nih.gov/pubmed/17478200?tool=bestpractice.com The technique is based on the premise that obstruction of the posterior semicircular canal lumen prevents endolymphatic flow and thus renders the cupula immobile.[79]Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1990 May;99(5 Pt 1):330-4. http://www.ncbi.nlm.nih.gov/pubmed/2337310?tool=bestpractice.com [87]Parnes LS, McClure JA. Posterior semicircular canal occlusion in the normal hearing ear. Otolaryngol Head Neck Surg. 1991;104:52-7. http://www.ncbi.nlm.nih.gov/pubmed/1900630?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer