The initial step in managing benign paroxysmal positional vertigo (BPPV) is patient education and reassurance.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication].
https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv
[42]Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005 Sep;26(5):1034-40.
http://www.ncbi.nlm.nih.gov/pubmed/16151355?tool=bestpractice.com
[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010. If lateral (horizontal) canal or superior (anterior) canal BPPV variants are suspected, then referral to a tertiary care dizziness clinic is indicated. All patients with posterior canal BPPV should be offered a particle repositioning maneuver (PRM) unless there is a specific contraindication.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
[44]Helminski JO, Zee DS, Janssen I, et al. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010 May;90(5):663-78.
https://academic.oup.com/ptj/article/90/5/663/2737747
http://www.ncbi.nlm.nih.gov/pubmed/20338918?tool=bestpractice.com
[45]Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E, et al. Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo [in Spanish]. Neurologia. 2010 Jun;25(5):295-9.
http://www.ncbi.nlm.nih.gov/pubmed/20643039?tool=bestpractice.com
Repositioning maneuvers are simple to perform and can be easily mastered by family practice and emergency physicians.[46]Munoz JE, Miklea JT, Howard M, et al. Canalith repositioning maneuver for benign paroxysmal positional vertigo: randomized controlled trial in family practice. Can Fam Physician. 2007 Jun;53(6):1049-53.
http://www.ncbi.nlm.nih.gov/pubmed/17872784?tool=bestpractice.com
[47]Chang AK, Schoeman G, Hill M. A randomized clinical trial to assess the efficacy of the Epley maneuver in the treatment of acute benign positional vertigo. Acad Emerg Med. 2004 Sep;11(9):918-24.
http://www.ncbi.nlm.nih.gov/pubmed/15347540?tool=bestpractice.com
Vestibular suppressant medications are not an effective treatment option in most patients.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication].
https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv
[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6.
http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
[49]McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980 Dec;9(6):472-7.
http://www.ncbi.nlm.nih.gov/pubmed/6110782?tool=bestpractice.com
[50]Fujino A, Tokumasu K, Yosio S, et al. Vestibular training for benign paroxysmal positional vertigo. Its efficacy in comparison with antivertigo drugs. Arch Otolaryngol Head Neck Surg. 1994 May;120(5):497-504.
http://www.ncbi.nlm.nih.gov/pubmed/8172700?tool=bestpractice.com
There is a small subpopulation of patients with prolonged autonomic dysfunction and imbalance who may benefit from vestibular suppressant medication, but the adverse effects of these medications must be carefully weighed prior to initiating treatment.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6.
http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Education and reassurance
Explaining the non-life-threatening nature of BPPV and its favorable prognosis reassures patients that BPPV is not a serious condition. BPPV spontaneously remits in one third of patients at 3 weeks and the majority of patients at 6 months from onset.[51]White J, Savvides P, Cherian N, et al. Canalith repositioning for benign paroxysmal positional vertigo. Otol Neurotol. 2005 Jul;26(4):704-10.
http://www.ncbi.nlm.nih.gov/pubmed/16015173?tool=bestpractice.com
[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.
It is highly treatable, with over 70% of episodes successfully treated after the administration of a single PRM.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
[44]Helminski JO, Zee DS, Janssen I, et al. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010 May;90(5):663-78.
https://academic.oup.com/ptj/article/90/5/663/2737747
http://www.ncbi.nlm.nih.gov/pubmed/20338918?tool=bestpractice.com
[45]Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E, et al. Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo [in Spanish]. Neurologia. 2010 Jun;25(5):295-9.
http://www.ncbi.nlm.nih.gov/pubmed/20643039?tool=bestpractice.com
However, relapses and remissions can occur unpredictably in both treated and untreated patients.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6.
http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Patients who have secondary BPPV (e.g., secondary to vestibular neuronitis) should be encouraged to return to normal physical activity to facilitate central nervous system (CNS) compensation.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.
Repositioning maneuvers
The first-line treatment of posterior canal BPPV is a PRM, designed to clear the affected semicircular canal of debris. The repositioning maneuvers have a proven efficacy in the treatment of objective, subjective, secondary, and bilateral forms of posterior canal BPPV.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
[44]Helminski JO, Zee DS, Janssen I, et al. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010 May;90(5):663-78.
https://academic.oup.com/ptj/article/90/5/663/2737747
http://www.ncbi.nlm.nih.gov/pubmed/20338918?tool=bestpractice.com
[45]Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E, et al. Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo [in Spanish]. Neurologia. 2010 Jun;25(5):295-9.
http://www.ncbi.nlm.nih.gov/pubmed/20643039?tool=bestpractice.com
Contraindications to their use include severe cervical disease, unstable cardiovascular disease, suspected vertebrobasilar disease, and high-grade carotid stenosis.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6.
http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
The goal of treating BPPV is to avoid many months of discomfort and the risk of accidents. Consequently, observation is not recommended in patients who are able to undergo a repositioning maneuver, given the maneuvers are simple, efficacious, and have a high benefit-to-risk ratio.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
There are several variants of PRM, including the Semont (liberatory) maneuver, the Epley maneuver, and the 3-position PRM.[52]Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290-3.
http://www.ncbi.nlm.nih.gov/pubmed/3213745?tool=bestpractice.com
[53]Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992 Sep;107(3):399-404.
http://www.ncbi.nlm.nih.gov/pubmed/1408225?tool=bestpractice.com
[54]Parnes LS, Price-Jones RG. Particle repositioning maneuver for benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1993 May;102(5):325-31.
http://www.ncbi.nlm.nih.gov/pubmed/8489160?tool=bestpractice.com
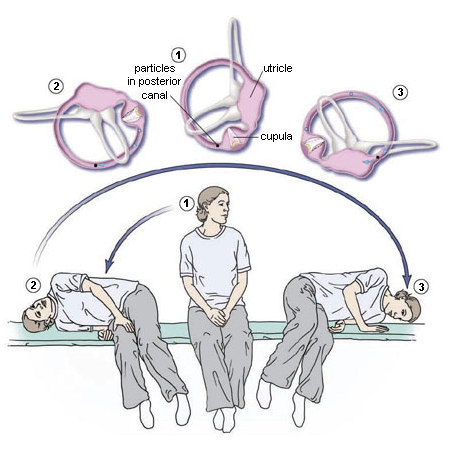
In the US, the 3-position PRM is used most frequently. It involves the following steps:
Place the patient in a sitting position at the end of the examination table.
Rotate the head 45° toward the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for primary stage nystagmus.
Maintain this position for 1-2 minutes.
The head is rotated 90° toward the opposite ear while maintaining the head hanging position.
Continue then to roll the whole patient (head and body) another 90° toward the unaffected side until the head is facing 180° from the original Dix-Hallpike position. This change in position should take <3-5 seconds.
The patient's eyes should be immediately observed for secondary-stage nystagmus. A favorable response occurs when the secondary-stage nystagmus is in the same direction as the primary-stage nystagmus, because the canalith particles would still be moving toward the utricle; an unfavorable response occurs when the nystagmus is in the opposite direction, which results when the particles regress away from the utricle toward its original position. Absence of nystagmus is not uncommon and may indicate mixed results, such as partial (incomplete) BPPV resolution.
Maintain the final position for 30-60 seconds, and then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful maneuver because the particles will have been cleared from the posterior semicircular canal back into the utricle.[Figure caption and citation for the preceding image starts]: Particle-repositioning maneuver (right ear)Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003:169:681-693; used with permission [Citation ends].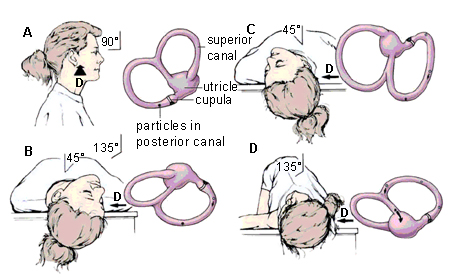
Trials have shown the Semont (liberatory) maneuver, the Epley maneuver, and the 3-position PRM to all be highly efficacious.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
The PRM is a variation of the Epley maneuver but is simpler and does not usually require sedation or mastoid vibration.[53]Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992 Sep;107(3):399-404.
http://www.ncbi.nlm.nih.gov/pubmed/1408225?tool=bestpractice.com
[54]Parnes LS, Price-Jones RG. Particle repositioning maneuver for benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1993 May;102(5):325-31.
http://www.ncbi.nlm.nih.gov/pubmed/8489160?tool=bestpractice.com
Although the PRM and Semont maneuvers share a similar mechanism and efficacy, the PRM is used by most clinicians in North America because it is more comfortable for the patient and simpler to perform, especially in overweight and older patients.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
[42]Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005 Sep;26(5):1034-40.
http://www.ncbi.nlm.nih.gov/pubmed/16151355?tool=bestpractice.com
[55]Salvinelli F, Trivelli M, Casale M, et al. Treatment of benign positional vertigo in the elderly: a randomized trial. Laryngoscope. 2004 May;114(5):827-31.
http://www.ncbi.nlm.nih.gov/pubmed/15126738?tool=bestpractice.com
[56]Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope. 1999 Apr;109(4):584-90.
http://www.ncbi.nlm.nih.gov/pubmed/10201745?tool=bestpractice.com
[57]Herdman SJ, Tusa RJ, Zee DS, et al. Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1993 Apr;119(4):450-4.
http://www.ncbi.nlm.nih.gov/pubmed/8457308?tool=bestpractice.com
[58]Mandalà M, Santoro GP, Asprella Libonati G, et al. Double-blind randomized trial on short-term efficacy of the Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. J Neurol. 2012 May;259(5):882-5.
http://www.ncbi.nlm.nih.gov/pubmed/22008871?tool=bestpractice.com
The PRM has a well-documented short-term efficacy, with the majority of patients successfully treated after a single PRM attempt.[2]Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003162.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25485940?tool=bestpractice.com
[44]Helminski JO, Zee DS, Janssen I, et al. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010 May;90(5):663-78.
https://academic.oup.com/ptj/article/90/5/663/2737747
http://www.ncbi.nlm.nih.gov/pubmed/20338918?tool=bestpractice.com
[45]Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E, et al. Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo [in Spanish]. Neurologia. 2010 Jun;25(5):295-9.
http://www.ncbi.nlm.nih.gov/pubmed/20643039?tool=bestpractice.com
Postmaneuver instructions, including post-PRM postural restrictions, are not necessary.[59]Gordon CR, Gadoth N. Repeated vs single physical maneuver in benign paroxysmal positional vertigo. Acta Neurol Scand. 2004 Sep;110(3):166-9.
http://www.ncbi.nlm.nih.gov/pubmed/15285773?tool=bestpractice.com
[60]Devaiah AK, Andreoli S. Postmaneuver restrictions in benign paroxysmal positional vertigo: an individual patient data meta-analysis. Otolaryngol Head Neck Surg. 2010 Feb;142(2):155-9.
http://www.ncbi.nlm.nih.gov/pubmed/20115966?tool=bestpractice.com
[61]Toupet M, Ferrary E, Bozorg Grayeli A. Effect of repositioning maneuver type
and postmaneuver restrictions on vertigo and dizziness in benign positional
paroxysmal vertigo. ScientificWorldJournal. 2012;2012:162123.
http://www.hindawi.com/journals/tswj/2012/162123
http://www.ncbi.nlm.nih.gov/pubmed/22973168?tool=bestpractice.com
[62]Mostafa BE, Youssef TA, Hamad AS. The necessity of post-maneuver postural restriction in treating benign paroxysmal positional vertigo: a meta-analytic study. Eur Arch Otorhinolaryngol. 2013 Mar;270(3):849-52.
http://www.ncbi.nlm.nih.gov/pubmed/22588196?tool=bestpractice.com
Many studies have found no benefit; however, a Cochrane review found a statistically significant benefit although this may not be clinically significant.[63]Hunt WT, Zimmermann EF, Hilton MP. Modifications of the Epley (canalith repositioning) manoeuvre for posterior canal benign paroxysmal positional vertigo (BPPV). Cochrane Database Syst Rev. 2012 Apr 18;(4):CD008675.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008675.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/22513962?tool=bestpractice.com
[  ]
In people with posterior canal benign paroxysmal positional vertigo (BPPV), how do modifications of the Epley (canalith repositioning) maneuver affect outcomes?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.68/fullShow me the answer
]
In people with posterior canal benign paroxysmal positional vertigo (BPPV), how do modifications of the Epley (canalith repositioning) maneuver affect outcomes?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.68/fullShow me the answer
A device for the home treatment of BPPV has been developed, which visually guides patients through the steps of the particle repositioning maneuver.[64]Bromwich MA, Parnes LS. The DizzyFIX: initial results of a new dynamic visual device for the home treatment of benign paroxysmal positional vertigo. J Otolaryngol Head Neck Surg. 2008 Jun;37(3):380-7.
http://www.ncbi.nlm.nih.gov/pubmed/19128643?tool=bestpractice.com
Adverse effects of particle repositioning maneuvers
Repositioning maneuvers have few adverse effects. An episode of BPPV is expected to occur during the therapeutic procedure. Occasionally, posterior BPPV can be converted to a lateral (horizontal) or anterior (superior) canal variant during a particle repositioning maneuver.[65]Herdman SJ, Tusa RJ. Complications of the canalith repositioning procedure. Arch Otolaryngol Head Neck Surg. 1996 Mar;122(3):281-6.
http://www.ncbi.nlm.nih.gov/pubmed/8607956?tool=bestpractice.com
These patients need to be treated with the appropriate maneuvers for these variants or referred to a specialist dizziness clinic. Fortunately, the lateral canal variant has a very high spontaneous recovery rate.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
Emesis has been reported during repositioning maneuvers, particularly with the lateral canal variant, and these patients may require antiemetic prophylaxis prior to initiating a subsequent repositioning maneuver.[66]Froehling DA, Bowen JM, Mohr DN, et al. The canalith repositioning procedure for the treatment of benign paroxysmal positional vertigo: a randomized controlled trial. Mayo Clin Proc. 2000 Jul;75(7):695-700.
http://www.ncbi.nlm.nih.gov/pubmed/10907384?tool=bestpractice.com
Prolonged autonomic dysfunction and imbalance may occur in a small subset of patients, and vestibular suppressant medications may be beneficial in these cases.
Repeating particle repositioning maneuvers
There is a dichotomy where some experts practice only one PRM treatment per clinic visit, while others repeat the PRM until no nystagmus is observed on Dix-Hallpike testing.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
The latter method is not recommended because an absent nystagmus response soon after a PRM may merely be the result of the Dix-Hallpike test's natural fatigability, as opposed to canalith clearance from the affected canal.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
Moreover, there does not appear to be a difference in efficacy between single versus repeated PRM treatments per clinic visit with regard to short-term results and long-term relapses.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
[59]Gordon CR, Gadoth N. Repeated vs single physical maneuver in benign paroxysmal positional vertigo. Acta Neurol Scand. 2004 Sep;110(3):166-9.
http://www.ncbi.nlm.nih.gov/pubmed/15285773?tool=bestpractice.com
It is recommended that repeated PRM attempts during a clinic visit be reserved only for patients with an unfavorable nystagmus response, such as a nonipsidirectional nystagmus (reversed or absent nystagmus) at the second stage of a 3-position PRM, or a reversed nystagmus in the sitting position at the conclusion of a 3-position PRM.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
An unfavorable nystagmus response has been documented to be a poor predictor of success.[54]Parnes LS, Price-Jones RG. Particle repositioning maneuver for benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1993 May;102(5):325-31.
http://www.ncbi.nlm.nih.gov/pubmed/8489160?tool=bestpractice.com
[67]Oh HJ, Kim JS, Han BI, et al. Predicting a successful treatment in posterior canal benign paroxysmal positional vertigo. Neurology. 2007 Apr 10;68(15):1219-22.
http://www.ncbi.nlm.nih.gov/pubmed/17420406?tool=bestpractice.com
However, it may take more than one clinic visit or session to successfully treat BPPV. Multiple sessions of the PRM are more efficacious than a single session.[68]White J, Savvides P, Cherian N, et al. Canalith repositioning for benign paroxysmal positional vertigo. Otol Neurotol. 2005 Jul;26(4):704-10.
http://www.ncbi.nlm.nih.gov/pubmed/16015173?tool=bestpractice.com
[69]Korres SG, Balatsouras DG, Papouliakos S, et al. Benign paroxysmal positional vertigo and its management. Med Sci Monit. 2007 Jun;13(6):CR275-82.
http://www.ncbi.nlm.nih.gov/pubmed/17534234?tool=bestpractice.com
Follow-up after particle repositioning maneuvers
If there is no sign of nystagmus and no symptoms of vertigo on Dix-Hallpike testing at follow-up, then the BPPV episode has resolved. All patients should undergo follow-up 1-4 weeks after treatment.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication].
https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv
The treated side should be retested first with the Dix-Hallpike maneuver. If it remains positive, another PRM should be attempted or a referral to a specialist dizziness clinic should be considered. If the Dix-Hallpike maneuver is negative on the treated side at follow-up, the Dix-Hallpike should be performed on the untreated side and if positive, a PRM should be carried out on this side.
Multiple failures of the particle repositioning maneuvers
If the PRM fails after repeat office visits, then timely referral to a tertiary care centre dizziness clinic is indicated.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
However, depending on the physician's experience and familiarity with BPPV and its management, other repositioning maneuvers may be attempted prior to referral. The Semont (liberatory) maneuver shares a similar mechanism and efficacy to the PRM and is the next option.[42]Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005 Sep;26(5):1034-40.
http://www.ncbi.nlm.nih.gov/pubmed/16151355?tool=bestpractice.com
[55]Salvinelli F, Trivelli M, Casale M, et al. Treatment of benign positional vertigo in the elderly: a randomized trial. Laryngoscope. 2004 May;114(5):827-31.
http://www.ncbi.nlm.nih.gov/pubmed/15126738?tool=bestpractice.com
[56]Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope. 1999 Apr;109(4):584-90.
http://www.ncbi.nlm.nih.gov/pubmed/10201745?tool=bestpractice.com
[57]Herdman SJ, Tusa RJ, Zee DS, et al. Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1993 Apr;119(4):450-4.
http://www.ncbi.nlm.nih.gov/pubmed/8457308?tool=bestpractice.com
[58]Mandalà M, Santoro GP, Asprella Libonati G, et al. Double-blind randomized trial on short-term efficacy of the Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. J Neurol. 2012 May;259(5):882-5.
http://www.ncbi.nlm.nih.gov/pubmed/22008871?tool=bestpractice.com
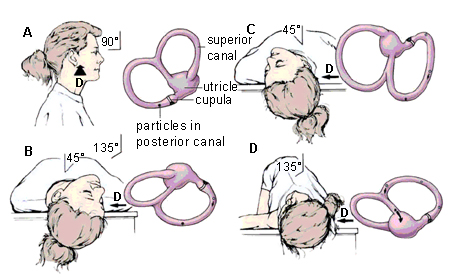
[Figure caption and citation for the preceding image starts]: Liberatory maneuver of Semont (right ear)Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003:169:681-693; used with permission [Citation ends].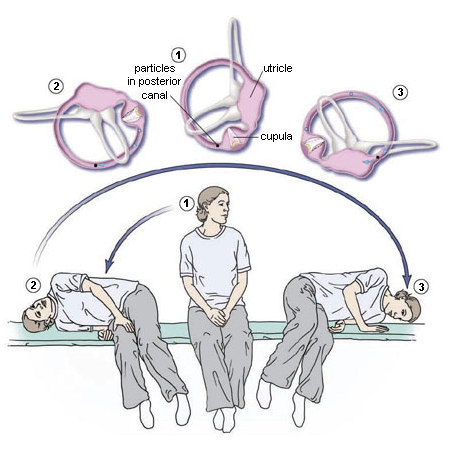
The Semont (liberatory) maneuver is thought to be useful for the treatment of both canalithiasis and cupulolithiasis forms of posterior canal BPPV.[69]Korres SG, Balatsouras DG, Papouliakos S, et al. Benign paroxysmal positional vertigo and its management. Med Sci Monit. 2007 Jun;13(6):CR275-82.
http://www.ncbi.nlm.nih.gov/pubmed/17534234?tool=bestpractice.com
The maneuver involves the following steps:
Sit the patient on an examination table, midway along the long side, with their legs hanging over the edge of the table.
Rotate the head 45° toward the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upward. This may induce nystagmus and vertigo because of particle movement toward the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downward. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes). Then slowly return the patient to the sitting position of step 1.
If both the PRM and the Semont (liberatory) maneuvers fail after repeat office visits, then referral to a specialist or tertiary care dizziness clinic is indicated.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
Repositioning maneuvers ineffective, contraindicated, or not tolerated
Contraindications to the use of repositioning maneuvers include severe cervical disease, unstable cardiovascular disease, suspected vertebrobasilar disease, and high-grade carotid stenosis.[48]Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999 Nov 18;341(21):1590-6.
http://www.ncbi.nlm.nih.gov/pubmed/10564690?tool=bestpractice.com
Patients with contra-indications to repositioning maneuvres and those unable to tolerate repositioning maneuvres or exercises may benefit from vestibular habituation therapy under the supervision of a physical therapist.[43]Wackym PA, Balaban CD, Schumacher TS. Vestibular disorders and rehabilitation. In: Bailey BJ, et al., eds. Head and neck surgery - otolaryngology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 2001:1993-2010.
If repositioning maneuvers fail after repeat office visits, then prompt referral to a tertiary specialist dizziness clinic is indicated.[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
Vestibular rehabilitation exercises
Some patients may benefit from vestibular rehabilitation exercises to promote functional recovery and prevent recurrence, particularly if they are at higher risk of falls or have residual generalized dizziness after BPPV treatment.[35]American Academy of Otolaryngology - Head and Neck Surgey. Clinical practice guideline: benign paroxysmal positional vertigo (update). Mar 2017 [internet publication].
https://www.entnet.org/quality-practice/quality-products/clinical-practice-guidelines/bppv
[70]McDonnell MN, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. 2015 Jan 13;(1):CD005397.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005397.pub4/full
http://www.ncbi.nlm.nih.gov/pubmed/25581507?tool=bestpractice.com
Vestibular rehabilitation consists of home exercises or a customised program delivered by a therapist. Suitable home exercises include the modified self-Epley, modified Semont, and half somersault maneuvres.[71]Ismail EI, Morgan AE, Abdeltawwab MM. Home particle repositioning maneuver to prevent the recurrence of posterior canal BPPV. Auris Nasus Larynx. 2018 Oct;45(5):980-4.
http://www.ncbi.nlm.nih.gov/pubmed/29526580?tool=bestpractice.com
[72]Ranju RL, Lepcha A, Mammen MD, et al. An effective home-based particle repositioning procedure for posterior canal benign paroxysmal positional vertigo (BPPV). Indian J Otolaryngol Head Neck Surg. 2022 Dec;74(4):516-23.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9741680
http://www.ncbi.nlm.nih.gov/pubmed/36514424?tool=bestpractice.com
[73]Foster CA, Ponnapan A, Zaccaro K, et al. A comparison of two home exercises for benign positional vertigo: half somersault versus Epley Maneuver. Audiology and Neurotology Extra. 2012 Apr 2020;2(1):16–23.
https://karger.com/aue/article/2/1/16/44463/A-Comparison-of-Two-Home-Exercises-for-Benign
[74]Radtke A, von Brevern M, Tiel-Wilck K, et al. Self-treatment of benign paroxysmal positional vertigo: Semont maneuver vs Epley procedure. Neurology. 2004 Jul 13;63(1):150-2.
http://www.ncbi.nlm.nih.gov/pubmed/15249626?tool=bestpractice.com
Patients with limited neck extension
For patients with cervical spine or other issues that limit neck extension, a 30° bed tilt during the PRM can avoid the need for neck extension. It should be noted that a 30° tilt is sufficient to cause the patient to slide down the bed. Thus, although most PRMs can be easily carried out by a solo clinician, a PRM with a 30° bed tilt will require at least one assistant. A chair that can spin and position the patient in any plane in space without the need for neck movements is available.[75]Nakayama M, Epley JM. BPPV and variants: improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005 Jul;133(1):107-12.
http://www.ncbi.nlm.nih.gov/pubmed/16025062?tool=bestpractice.com
Subjective BPPV
Subjective BPPV occurs when the Dix-Hallpike maneuver or supine lateral head roll induces the typical vertigo with latency and limited duration, but without any objective nystagmus. This subset of patients is also highly responsive to repositioning maneuvers.[16]Haynes DS, Resser JR, Labadie RF, et al. Treatment of benign positional vertigo using the Semont maneuver: efficacy in patients presenting without nystagmus. Laryngoscope. 2002 May;112(5):796-801.
http://www.ncbi.nlm.nih.gov/pubmed/12150609?tool=bestpractice.com
[39]Tirelli G, D'Orlando E, Giacomarra V, et al. Benign positional vertigo without detectable nystagmus. Laryngoscope. 2001 Jun;111(6):1053-6.
http://www.ncbi.nlm.nih.gov/pubmed/11404620?tool=bestpractice.com
Secondary BPPV and bilateral BPPV
Repositioning maneuvers are efficacious in both primary and secondary causes of BPPV.[76]O'Reilly RC, Elford B, Slater R. Effectiveness of the particle repositioning maneuver in subtypes of benign paroxysmal positional vertigo. Laryngoscope. 2000 Aug;110(8):1385-8.
http://www.ncbi.nlm.nih.gov/pubmed/10942146?tool=bestpractice.com
[77]Gordon CR, Levite R, Joffe V, et al. Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form? Arch Neurol. 2004 Oct;61(10):1590-3.
http://www.ncbi.nlm.nih.gov/pubmed/15477514?tool=bestpractice.com
Post-traumatic causes of BPPV are also highly amenable to treatment via the PRM, although it is more difficult to treat and has greater recurrences compared with nontraumatic forms.[77]Gordon CR, Levite R, Joffe V, et al. Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form? Arch Neurol. 2004 Oct;61(10):1590-3.
http://www.ncbi.nlm.nih.gov/pubmed/15477514?tool=bestpractice.com
Simultaneous bilateral BPPV is usually the result of a closed-head injury.[40]Kaplan DM, Nash M, Niv A, et al. Management of bilateral benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2005 Nov;133(5):769-73.
http://www.ncbi.nlm.nih.gov/pubmed/16274807?tool=bestpractice.com
This phenomenon is diagnosed when patients are Dix-Hallpike positive on both sides simultaneously, and this condition is also amenable to repositioning maneuvers.[40]Kaplan DM, Nash M, Niv A, et al. Management of bilateral benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2005 Nov;133(5):769-73.
http://www.ncbi.nlm.nih.gov/pubmed/16274807?tool=bestpractice.com
The side with the stronger vertigo and nystagmus response should be treated at the initial visit, whereas the other side is left alone to avoid re-displacing the canalith particles back into the contralateral (original) posterior canal.[40]Kaplan DM, Nash M, Niv A, et al. Management of bilateral benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2005 Nov;133(5):769-73.
http://www.ncbi.nlm.nih.gov/pubmed/16274807?tool=bestpractice.com
Surgical options
The vast majority of BPPV cases will respond to repositioning maneuvers or resolve spontaneously. The surgical treatment of BPPV is reserved for unrelenting cases in which severe symptoms and incapacity remain despite repeated attempts with repositioning maneuvers and vestibular rehabilitation exercises.[78]Walsh RM, Bath AP, Cullen JR, et al. Long-term results of posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol Allied Sci. 1999 Aug;24(4):316-23.
http://www.ncbi.nlm.nih.gov/pubmed/10472467?tool=bestpractice.com
[79]Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1990 May;99(5 Pt 1):330-4.
http://www.ncbi.nlm.nih.gov/pubmed/2337310?tool=bestpractice.com
Surgical treatment may also be considered for patients who respond to PRMs but have unremitting recurrences soon after and would prefer a definitive solution rather than repeated PRMs. Less than 1% of BPPV patients will ever require surgery, but because BPPV is so prevalent the actual number of surgical candidates is not negligible.[80]Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006 Mar;134(3):424-30.
http://www.ncbi.nlm.nih.gov/pubmed/16500439?tool=bestpractice.com
Prior to undergoing surgery, all other potential diagnoses must be excluded and the posterior fossa imaged.
There are two surgical procedures for BPPV: singular neurectomy and posterior canal occlusion. The recommended surgical procedure is posterior canal occlusion, as this has been shown to be a highly efficacious, safe, and reproducible technique.[78]Walsh RM, Bath AP, Cullen JR, et al. Long-term results of posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol Allied Sci. 1999 Aug;24(4):316-23.
http://www.ncbi.nlm.nih.gov/pubmed/10472467?tool=bestpractice.com
[79]Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1990 May;99(5 Pt 1):330-4.
http://www.ncbi.nlm.nih.gov/pubmed/2337310?tool=bestpractice.com
[80]Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006 Mar;134(3):424-30.
http://www.ncbi.nlm.nih.gov/pubmed/16500439?tool=bestpractice.com
[81]Agrawal SK, Parnes LS. Human experience with canal plugging. Ann N Y Acad Sci. 2001 Oct;942:300-5.
http://www.ncbi.nlm.nih.gov/pubmed/11710471?tool=bestpractice.com
[82]Pace-Balzan A, Rutka JA. Non-ampullary plugging of the posterior semicircular canal for benign paroxysmal positional vertigo. J Laryngol Otol. 1991 Nov;105(11):901-6.
http://www.ncbi.nlm.nih.gov/pubmed/1761943?tool=bestpractice.com
[83]Dingle AF, Hawthorne MR, Kumar BU. Fenestration and occlusion of the posterior semicircular canal for benign positional vertigo. Clin Otolaryngol Allied Sci. 1992 Aug;17(4):300-2.
http://www.ncbi.nlm.nih.gov/pubmed/1526046?tool=bestpractice.com
[84]Hawthorne M, el-Naggar M. Fenestration and occlusion of posterior semicircular canal for patients with intractable benign paroxysmal positional vertigo. J Laryngol Otol. 1994 Nov;108(11):935-9.
http://www.ncbi.nlm.nih.gov/pubmed/7829944?tool=bestpractice.com
[85]Anthony PF. Partitioning the labyrinth for benign paroxysmal positional vertigo: clinical and histologic findings. Am J Otol. 1993 Jul;14(4):334-42.
http://www.ncbi.nlm.nih.gov/pubmed/8238267?tool=bestpractice.com
[86]Leveque M, Labrousse M, Seidermann L, et al. Surgical therapy in intractable benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2007 May;136(5):693-8.
http://www.ncbi.nlm.nih.gov/pubmed/17478200?tool=bestpractice.com
[87]Parnes LS, McClure JA. Posterior semicircular canal occlusion in the normal hearing ear. Otolaryngol Head Neck Surg. 1991;104:52-7.
http://www.ncbi.nlm.nih.gov/pubmed/1900630?tool=bestpractice.com
The premise is that obstruction of the posterior semicircular canal lumen prevents endolymphatic flow and thus renders the cupula immobile.
Outcomes are excellent. One systematic review found 94 of 97 ears treated were completely cured, with only four cases of hearing loss.[86]Leveque M, Labrousse M, Seidermann L, et al. Surgical therapy in intractable benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2007 May;136(5):693-8.
http://www.ncbi.nlm.nih.gov/pubmed/17478200?tool=bestpractice.com
Studies that used the validated Dizziness Handicap Inventory (DHI) questionnaire found DHI scores of 18.05 and 38.5 in BPPV patients before a PRM treatment, whereas preoperative patients with intractable BPPV had DHI scores of 70.[76]O'Reilly RC, Elford B, Slater R. Effectiveness of the particle repositioning maneuver in subtypes of benign paroxysmal positional vertigo. Laryngoscope. 2000 Aug;110(8):1385-8.
http://www.ncbi.nlm.nih.gov/pubmed/10942146?tool=bestpractice.com
[88]Lopez-Escamez JA, Gamiz MJ, Fernandez-Perez A, et al. Impact of treatment on health-related quality of life in patients with posterior canal benign paroxysmal positional vertigo. Otol Neurotol. 2003 Jul;24(4):637-41.
http://www.ncbi.nlm.nih.gov/pubmed/12851558?tool=bestpractice.com
[80]Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006 Mar;134(3):424-30.
http://www.ncbi.nlm.nih.gov/pubmed/16500439?tool=bestpractice.com
Hence, many experts consider intractable BPPV a nonbenign condition, in contradistinction to what the name would suggest.[86]Leveque M, Labrousse M, Seidermann L, et al. Surgical therapy in intractable benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2007 May;136(5):693-8.
http://www.ncbi.nlm.nih.gov/pubmed/17478200?tool=bestpractice.com
One study involving 28 patients who had undergone posterior canal occlusion surgery with a mean follow-up of 40 months found all patients had a negative Dix-Hallpike test post-surgery, 95% improved significantly on the DHI questionnaire from an average score of 70 preoperatively to 13 postoperatively, and 85% were satisfied with their postoperative experience.[80]Shaia WT, Zappia JJ, Bojrab DI, et al. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006 Mar;134(3):424-30.
http://www.ncbi.nlm.nih.gov/pubmed/16500439?tool=bestpractice.com
Recurrent BPPV
Recurrences are common after successful treatment with repositioning maneuvers, as high as 50% after 40 months post-treatment, and further repositioning maneuvers are indicated in these circumstances.[89]Nunez RA, Cass SP, Furman JM. Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2000 May;122(5):647-52.
http://www.ncbi.nlm.nih.gov/pubmed/10793340?tool=bestpractice.com
Meniere disease (endolymphatic hydrops), central nervous system diseases, migraine headaches, and post-traumatic BPPV have all been associated with a greater risk of recurrence.[22]Ishiyama A, Jacobson KM, Baloh RW. Migraine and benign positional vertigo. Ann Otol Rhinol Laryngol. 2000 Apr;109(4):377-80.
http://www.ncbi.nlm.nih.gov/pubmed/10778892?tool=bestpractice.com
[23]Lempert T, Leopold M, von Brevern M, et al. Migraine and benign positional vertigo. Ann Otol Rhinol Laryngol. 2000 Dec;109(12 Pt 1):1176.
http://www.ncbi.nlm.nih.gov/pubmed/11130835?tool=bestpractice.com
[77]Gordon CR, Levite R, Joffe V, et al. Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form? Arch Neurol. 2004 Oct;61(10):1590-3.
http://www.ncbi.nlm.nih.gov/pubmed/15477514?tool=bestpractice.com
[90]Del Rio M, Arriaga MA. Benign positional vertigo: prognostic factors. Otolaryngol Head Neck Surg. 2004 Apr;130(4):426-9.
http://www.ncbi.nlm.nih.gov/pubmed/15100638?tool=bestpractice.com
Thus, all factors suggest that a long-term recurrence of BPPV is not due to a recalcitrant condition, but instead results from a new episode of the underlying condition that originally caused the BPPV. Persistent recurrences despite adequate treatment are an indication for referral to a tertiary specialist dizziness clinic. Some patients can be taught how to do repositioning maneuvers at home on an intermittent basis when their symptoms recur. Devices to assist patients perform these exercises are available.[64]Bromwich MA, Parnes LS. The DizzyFIX: initial results of a new dynamic visual device for the home treatment of benign paroxysmal positional vertigo. J Otolaryngol Head Neck Surg. 2008 Jun;37(3):380-7.
http://www.ncbi.nlm.nih.gov/pubmed/19128643?tool=bestpractice.com
Specialist referral
Referral to a tertiary specialist dizziness clinic is indicated in the following situations:[7]Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93.
http://www.cmaj.ca/content/169/7/681.full
http://www.ncbi.nlm.nih.gov/pubmed/14517129?tool=bestpractice.com
Nonresponse to treatment
Multiple recurrences despite adequate treatment
Suspected lateral (horizontal) canal and the rare superior (anterior) canal BPPV variants
Atypical cases (symptoms of hearing loss, tinnitus, pressure sensations or aural fullness, symptoms triggered by ear or intracranial pressure changes, signs of middle ear infection, odd nystagmus profiles during positioning maneuvers, persistent dizziness or unsteadiness)
Patients with other neurologic symptoms and signs that may require imaging of the posterior fossa.
Horizontal BPPV and anterior BPPV
If horizontal canal or anterior canal BPPV variants are suspected, then referral to a tertiary care dizziness clinic is indicated. Repositioning maneuvers do exist for both these variants. In the case of horizontal canal BPPV caused by canalithiasis, options include the "barrel roll", "log roll", or "barbeque roll" maneuvers, where the patient is moved supine to supine in 90 degree increments. It starts in the supine lateral position with the face and body turned toward the affected side. The face and body are then turned back to the midline neutral supine position and held there for 1 or 2 minutes. The face and body is then turned to the opposite side and held for 1 or 2 minutes. The face and body are then turned toward the ground by having the patient turn onto their belly and held for 1 or 2 minutes. Finally, the face and body are turned further in the same direction back to the original supine lateral position of the affected ear.
In anterior canal BPPV, studies examining therapeutic maneuver techniques and efficacy are scant versus its counterparts. The particle repositioning maneuver or Epley maneuver for posterior canal BPPV seems to have some efficacy in anterior canal BPPV. A "reverse Epley" maneuver has been described. Another variant is the Yacovino maneuver, where the patient is moved from a sitting to lying position, with the head hanging (extended) straight back without rotation. Subsequently the patient’s head is flexed, and then the patient is brought back up to the sitting position to complete the maneuver. Success rates vary from 36% to 100% in the literature for the various anterior canal BPPV positioning maneuvers.[38]Anagnostou E, Kouzi I, Spengos K. Diagnosis and treatment of anterior-canal benign paroxysmal positional vertigo: a systematic review. J Clin Neurol. 2015 Jul;11(3):262-7.
http://thejcn.com/DOIx.php?id=10.3988/jcn.2015.11.3.262
http://www.ncbi.nlm.nih.gov/pubmed/26022461?tool=bestpractice.com
 ]
]