Tests
1st tests to order
Wells score
Test
Not a definitive test but should be determined in all patients with suspected DVT. Wells score provides a method to determine the clinical probability of DVT and is the most widely accepted pretest probability tool used in diagnostic algorithms for DVT.[117][118] If the Wells score is 2 or greater, condition is likely (absolute risk is approximately 40%).[117][118] People with a score of <2 are unlikely to have a DVT (probability <15%).[117][118]
The criteria are as follows:
Active cancer (any treatment within past 6 months): 1 point
Calf swelling where affected calf circumference measures >3 cm more than the other calf (measured 10 cm below tibial tuberosity): 1 point
Prominent superficial veins (nonvaricose): 1 point
Pitting edema (confined to symptomatic leg): 1 point
Swelling of entire leg: 1 point
Localized pain along distribution of deep venous system: 1 point
Paralysis, paresis, or recent cast immobilization of lower extremities: 1 point
Recent bed rest for >3 days or major surgery requiring regional or general anesthetic within past 12 weeks: 1 point
Previous history of DVT or pulmonary embolism: 1 point
Alternative diagnosis at least as probable: subtract 2 points.
This test has not been validated in the pregnant population and, therefore, should not be routinely used to risk stratify a pregnant woman with a suspected DVT. A clinical prediction rule termed the LEFt score has been developed specifically for the pregnant population; however, this rule has yet to be rigorously validated and should also not be used routinely.[119]
Result
score ≥2: DVT likely (proceed to imaging); score <2: DVT unlikely (proceed to D-dimer)
quantitative D-dimer level
Test
Indicated in all patients where a DVT is considered unlikely (e.g., Wells score of <2). In these patients a normal D-dimer value excludes the diagnosis of DVT.[122]
Clinicians should not obtain a D-dimer measurement in patients with a high clinical probability of DVT; immediate imaging is indicated.[27]
In outpatients with a suspected venous thromboembolic event, point-of-care tests can contribute important information and guide patient management in patients with a low-probability score on a clinical decision rule.[123] For example, a negative test excludes DVT when the pretest probability is low.
Not a definitive test. Elevated levels are highly sensitive but nonspecific.[117][124][125] It is frequently abnormal in patients who are older, are acutely ill, have underlying hepatic disease, have an infection, or are pregnant.
Regardless of the patient group, D-dimer has a low positive predictive value. Approaches to mitigate the low specificity of D-dimer have included adjusting the cutoff value based on the patient's age (e.g., age [years] × 10 micrograms/L [using D-dimer assays with a cutoff of 500 micrograms/L] in patients >50 years old) or by the pretest probability of DVT (if using a risk assessment model with three categories).[126]
The D-dimer assay plays a limited role in pregnancy due to its natural rise with each trimester.[128] However, a negative D-dimer test may be useful in ruling out a diagnosis of DVT in these patients.[129]
Result
normal (DVT excluded if Wells score <2); elevated (proceed to imaging)
venous duplex ultrasound (DUS)
Test
Assesses venous flow by the use of Doppler and vein compression.[120]
First-line test in all high-probability patients (Wells score of 2 or more) or in low-probability patients (Wells score <2) with an elevated D-dimer level.[120] Diagnosis of an acute clot is based on the inability to completely collapse the walls of the vein in the transverse plane by pressing down on the vein with a transducer probe (the presence of thrombus prevents compression).[120][Figure caption and citation for the preceding image starts]: Short-axis ultrasound view showing the femoral vein and profunda femoris vein adjacent to the femoral artery before compression (left) and compressed (right)From the collection of Jeffrey W. Olin; used with permission [Citation ends].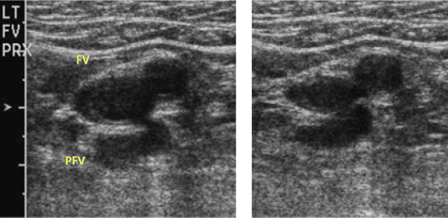
High sensitivity and specificity of over 95%.[130] Venous ultrasound has a high sensitivity because: 1) deep veins in the lower extremities are easily visualized; 2) it scans multiple areas, making it likely that at least a portion of a clot is detected; and 3) compression readily identifies intravascular thrombus.
There are two well-validated techniques to perform venous ultrasound of the leg. Whole-leg ultrasound assesses the veins of both the upper leg and the calf. It takes longer to perform, is technically more demanding, and identifies calf-vein DVT, which might resolve without treatment (thus can lead to over-diagnosis and potentially over-treatment with anticoagulation, subjecting the patient to possible bleeding complications). However, it is able to reach a diagnostic conclusion in a single session.[120] Proximal DUS assesses only the veins above the calf. While faster and simpler, if negative it must be repeated 5-7 days later to exclude any undetected calf-vein DVTs that have propagated proximally.
Ultrasound cannot provide the exact age of a vein clot, but comparison to prior imaging studies, if available, is a reliable method for differentiating acute from preexisting thrombosis.
Ultrasound testing can be limited to only the proximal deep venous system, so long as patients with a positive D-dimer or high probability and who have an initially normal proximal ultrasound undergo a repeat ultrasound in 5-7 days.[131] A serial ultrasound strategy may be necessary to exclude proximal extension of the thrombus into the popliteal veins or beyond.[120]
In high-probability patients, a repeat ultrasound is indicated in 5-7 days if the initial ultrasound test is normal.
In low-probability patients, a repeat ultrasound is indicated in 5-7 days if D-dimer level is elevated and initial ultrasound is normal.
The subsequent rate of venous thromboembolism following a negative diagnostic evaluation does not appear to meaningfully differ between whole-leg ultrasound and serial proximal ultrasound.[131]
The initial test of choice for a pregnant woman suspected of having a DVT. The American College of Chest Physicians advocates the use of serial, proximal ultrasonography if a DVT is suspected in pregnant women.[27]
Result
abnormal: inability to fully compress lumen of vein using ultrasound transducer; normal: all vein segments fully compressible, nondiagnostic
INR and activated partial thromboplastin time (aPTT)
Test
INR is required before starting warfarin, and aPTT is required before starting intravenous heparin.
Result
baseline values
BUN and creatinine
Test
Doses of some anticoagulants (e.g., low molecular weight heparin, fondaparinux, apixaban, rivaroxaban, dabigatran, edoxaban) may need to be adjusted or discontinued in patients with renal impairment, so baseline values should be obtained.
Result
baseline values
LFTs
Test
May detect abnormalities associated with underlying provoking factor (e.g., cancer). Some anticoagulants are not approved for varying degrees of hepatic dysfunction
Result
baseline values
CBC
Test
A component of the assessment of bleeding risk while using an anticoagulant. Very low values are a contraindication to anticoagulation.
May detect abnormalities such as underlying hematologic malignancy (e.g., anemia, leukopenia).
A high platelet count may suggest essential thrombocytosis or a myeloproliferative disorder. Exceedingly low platelet count may preclude the use of some anticoagulants.
Heparin therapy can be associated with heparin-induced thrombocytopenia; platelet counts should be measured at baseline and regularly throughout treatment.
Result
baseline values
Tests to consider
Doppler venous flow testing
Test
Color flow Doppler and pulse-wave are sometimes done in conjunction with B-mode image ultrasonography. The absence of respiratory variations on pulse-wave Doppler raises the suspicion of a proximal venous obstruction.[120]
Low sensitivity (75%) and medium specificity (85%).[132][133]
Result
reduced or absent spontaneous flow, lack of respiratory variation, intraluminal echoes, or color flow patency abnormalities
CT abdomen and pelvis with contrast
Test
More accurate than ultrasound for visceral veins and deep veins of abdomen and pelvis.
May be utilized when more proximal thrombosis is clinically suspected or suggested by flow patterns on Doppler ultrasound.[132]
Result
presence of an intraluminal filling defect
thrombophilia screen
Test
Thrombophilia commonly refers to five hereditary conditions (factor V Leiden, prothrombin gene 20210A, deficiencies in antithrombin, protein C deficiency, and protein S deficiency) and antiphospholipid syndrome (an acquired condition). However, many gene variants and acquired conditions modify thrombosis risk.[134]
Indications for screening are controversial.[134][135] Hereditary thrombophilia does not sufficiently modify the predicted risk of recurrent thrombosis to affect treatment decisions, and does not significantly increase the predicted risk of recurrent venous thromboembolism (VTE) after a provoked DVT; a conservative approach to testing is reasonable, and in general guidelines discourage testing in this setting.[18][55][56] Some guidelines suggest testing only in situations where the result is likely to change a clinical decision (such as in patients with unprovoked DVT or pulmonary embolism [PE] who are considering stopping anticoagulants).[19][54][136]
If a thrombophilia screen is indicated, it should be deferred until a minimum of 3 months of anticoagulant therapy has been completed because some thrombophilia tests are influenced by the presence of acute thrombosis or anticoagulant therapy.[134]
Antiphospholipid antibodies may predict a higher risk of future thrombosis following an initial VTE event and may impact selection of therapy.[62] Controversy exists regarding whether broad screening for antiphospholipid antibodies or screening only on the basis of clinical suspicion should be preferred.[137] Some guidelines suggest testing only in situations where the result is likely to change a clinical decision (such as in patients with unprovoked DVT or PE who are considering stopping anticoagulants; however, these guidelines recommend seeking specialist advice as these tests may be affected by anticoagulants).[19]
For antiphospholipid antibody screening, cardiolipin and beta-2 glycoprotein-I antibodies can be performed without regard to the presence of anticoagulants; however, most anticoagulants interfere with assays for lupus anticoagulant.[62]
Result
positive in inherited thrombophilias; elevated titers/abnormal result in antiphospholipid syndrome
Use of this content is subject to our disclaimer