Intussusception
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
clinically stable with no contraindications to contrast enema reduction
fluid resuscitation + contrast enema reduction
Careful monitoring is required during transit to the radiology department, as well as during the procedure. Access to monitoring and resuscitation equipment, and nursing and medical staff capable of managing a child who may become unstable, are essential.
Adequate intravenous access is required and isotonic fluid resuscitation initiated. Contrast enema (air or contrast liquid) should be performed only in patients who are clinically stable. Absolute contraindications include peritonitis, perforation, and hypovolemic shock.[28]American College of Radiology. ACR-SPR practice parameter for the performance of pediatric fluoroscopic contrast enema examinations. 2021 [internet publication]. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/fluourconenema-ped.pdf
Reduction should be first attempted by contrast enema (air or contrast liquid) which can be both diagnostic and therapeutic.[Figure caption and citation for the preceding image starts]: Site of intussusception as revealed by abdominal x-ray, showing the meniscusFrom the collection of Dr David J. Hackam; used with permission [Citation ends].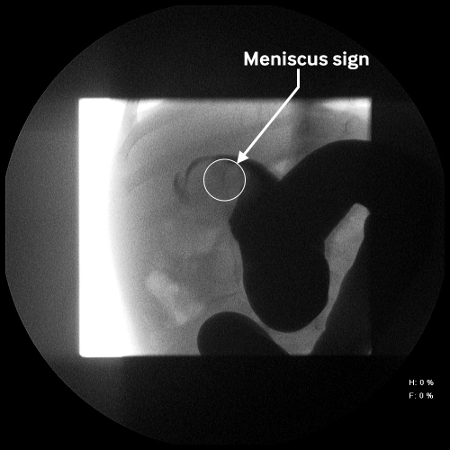 [Figure caption and citation for the preceding image starts]: Abdominal x-ray showing impaired passage of barium at site of obstruction due to intussusceptionFrom the collection of Dr David J. Hackam; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Abdominal x-ray showing impaired passage of barium at site of obstruction due to intussusceptionFrom the collection of Dr David J. Hackam; used with permission [Citation ends].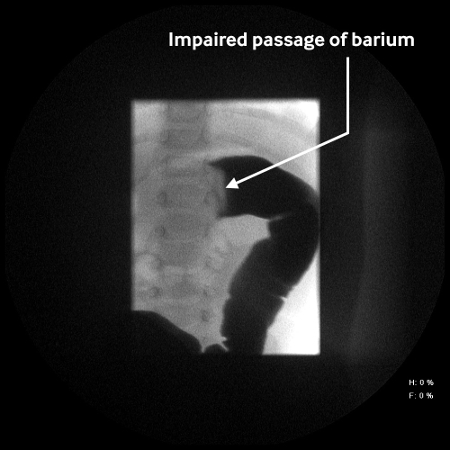 Pneumatic reduction is considered the method of choice for the treatment of intussusception in stable patients provided there is no indication for surgical reduction.[31]Beres AL, Baird R. An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery. 2013 Aug;154(2):328-34.
http://www.ncbi.nlm.nih.gov/pubmed/23889959?tool=bestpractice.com
[32]Beasley SW. The 'ins' and 'outs' of intussusception: Where best practice reduces the need for surgery. J Paediatr Child Health. 2017 Nov;53(11):1118-1122.
https://www.doi.org/10.1111/jpc.13738
http://www.ncbi.nlm.nih.gov/pubmed/29148203?tool=bestpractice.com
Protocols typically vary by institutions but often involve instillation of air and/or contrast at pressures ranging from 80 to 120 mm Hg.[28]American College of Radiology. ACR-SPR practice parameter for the performance of pediatric fluoroscopic contrast enema examinations. 2021 [internet publication].
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/fluourconenema-ped.pdf
The patient is kept nil by mouth.
Pneumatic reduction is considered the method of choice for the treatment of intussusception in stable patients provided there is no indication for surgical reduction.[31]Beres AL, Baird R. An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery. 2013 Aug;154(2):328-34.
http://www.ncbi.nlm.nih.gov/pubmed/23889959?tool=bestpractice.com
[32]Beasley SW. The 'ins' and 'outs' of intussusception: Where best practice reduces the need for surgery. J Paediatr Child Health. 2017 Nov;53(11):1118-1122.
https://www.doi.org/10.1111/jpc.13738
http://www.ncbi.nlm.nih.gov/pubmed/29148203?tool=bestpractice.com
Protocols typically vary by institutions but often involve instillation of air and/or contrast at pressures ranging from 80 to 120 mm Hg.[28]American College of Radiology. ACR-SPR practice parameter for the performance of pediatric fluoroscopic contrast enema examinations. 2021 [internet publication].
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/fluourconenema-ped.pdf
The patient is kept nil by mouth.
Barium enema: advantages over other types of contrast enema reduction include a long-standing experience in some centers, effective reduction in most cases, good evaluation for residual intussusception, and a low perforation rate. Disadvantages include the need for x-ray exposure, chemical peritonitis in the event of a perforation, and visualization of only intraluminal content. Water-soluble contrast enema has been used to reduce the risk of chemical peritonitis resulting from perforation. Reduction rate and perforation rate are comparable with other contrast agents.
Air enemas: these are noted to require less radiation and offer similar rates of failure, recurrence, and perforation to other agents.
Ultrasound-guided saline enema: excellent results have been described with the use of this modality, which offers the advantage of limiting exposure to radiation.[31]Beres AL, Baird R. An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery. 2013 Aug;154(2):328-34. http://www.ncbi.nlm.nih.gov/pubmed/23889959?tool=bestpractice.com [33]Xie X, Wu Y, Wang Q, et al. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediatr Surg. 2018 Aug;53(8):1464-1468. https://www.doi.org/10.1016/j.jpedsurg.2017.08.005 http://www.ncbi.nlm.nih.gov/pubmed/28827051?tool=bestpractice.com Although there is less experience with this method than fluoroscopic reduction, it is being used with increasing frequency in Europe and elsewhere.[21]Sorantin E, Lindbichler F. Management of intussusception. Eur Radiol. 2004 Mar;14(suppl 4):L146-54. http://www.ncbi.nlm.nih.gov/pubmed/14752570?tool=bestpractice.com [22]del-Pozo G, Albillos JC, Tejedor D, et al. Intussusception in children: current concepts in diagnosis and enema reduction. Radiographics. 1999 Mar-Apr;19(2):299-319. http://pubs.rsna.org/doi/full/10.1148/radiographics.19.2.g99mr14299 http://www.ncbi.nlm.nih.gov/pubmed/10194781?tool=bestpractice.com [32]Beasley SW. The 'ins' and 'outs' of intussusception: Where best practice reduces the need for surgery. J Paediatr Child Health. 2017 Nov;53(11):1118-1122. https://www.doi.org/10.1111/jpc.13738 http://www.ncbi.nlm.nih.gov/pubmed/29148203?tool=bestpractice.com [33]Xie X, Wu Y, Wang Q, et al. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediatr Surg. 2018 Aug;53(8):1464-1468. https://www.doi.org/10.1016/j.jpedsurg.2017.08.005 http://www.ncbi.nlm.nih.gov/pubmed/28827051?tool=bestpractice.com [34]Flaum V, Schneider A, Gomes Ferreira C, et al. Twenty years' experience for reduction of ileocolic intussusceptions by saline enema under sonography control. J Pediatr Surg. 2016 Jan;51(1):179-82. https://www.doi.org/10.1016/j.jpedsurg.2015.09.022 http://www.ncbi.nlm.nih.gov/pubmed/26592955?tool=bestpractice.com [37]Daneman A, Navarro O. Intussusception. Part 2: an update on the evolution of management. Pediatr Radiol. 2004 Feb;34(2):97-108. http://www.ncbi.nlm.nih.gov/pubmed/14634696?tool=bestpractice.com
broad-spectrum antibiotics
Treatment recommended for SOME patients in selected patient group
The role of antibiotics is unclear. In some centers they are no longer routinely indicated in children with intussusception. In others, the potential for poorly perfused or dilated bowel to translocate and produce a bacteraemia is seen as an indication. Administration of prophylactic antibiotics before enema reduction does not appear to reduce the risk of postreduction complications.[29]Kelley-Quon LI, Arthur LG, Williams RF, et al. Management of intussusception in children: a systematic review. J Pediatr Surg. 2021 Mar;56(3):587-96. https://www.doi.org/10.1016/j.jpedsurg.2020.09.055 http://www.ncbi.nlm.nih.gov/pubmed/33158508?tool=bestpractice.com
When indicated, broad-spectrum antibiotics covering intra-abdominal pathogens should be administered.
Administer antibiotics 1 hour before the procedure if possible, and then consider continuing antibiotics after reduction for up to 48 hours if ischemia or significant dilatation is present.
Antibiotic regimens vary according to local protocols; consult local guidance.
Primary options
clindamycin: neonates: consult specialist for guidance on dose; infants and children: 25-40 mg/kg/day intravenously/intramuscularly given in divided doses every 6-8 hours
and
gentamicin: neonates: consult specialist for guidance on dose; infants and children: 2 to 2.5 mg/kg intravenously/intramuscularly every 8 hours
OR
piperacillin/tazobactam: neonates and infants <2 months of age: consult specialist for guidance on dose; children: 2-8 months of age: 80 mg/kg intravenously every 8 hours; children ≥9 months of age and ≤40 kg: 100 mg/kg intravenously every 8 hours
More piperacillin/tazobactamDose refers to piperacillin component.
OR
cefoxitin: neonates and infants ≤3 months of age: consult specialist for guidance on dose; children >3 months of age: 25 mg/kg intravenously every 4-6 hours
and
vancomycin: neonates: consult specialist for guidance on dose; infants and children: 10 mg/kg intravenously every 6 hours
fluid resuscitation + surgical reduction
Failure of nonoperative reduction strategies requires surgical evaluation and reduction. Factors that suggest a lower reduction rate (as well as higher perforation rate) include patient age <3 months or >5 years, long duration of symptoms (>48 hours), passage of blood via the rectum, significant dehydration, small-bowel obstruction, and visualization of a coiled spring sign.[21]Sorantin E, Lindbichler F. Management of intussusception. Eur Radiol. 2004 Mar;14(suppl 4):L146-54. http://www.ncbi.nlm.nih.gov/pubmed/14752570?tool=bestpractice.com
Traditionally, operative reduction has been performed through an open approach via a right lower quadrant incision. The intussusception is identified and milked out of the intussuscipiens. Successful laparoscopic reduction has been described and is becoming popular; the intussusceptum is reduced by applying gentle traction.[29]Kelley-Quon LI, Arthur LG, Williams RF, et al. Management of intussusception in children: a systematic review. J Pediatr Surg. 2021 Mar;56(3):587-96. https://www.doi.org/10.1016/j.jpedsurg.2020.09.055 http://www.ncbi.nlm.nih.gov/pubmed/33158508?tool=bestpractice.com [35]Kia KF, Mony VK, Drongowski RA, et al. Laparoscopic vs open surgical approach for intussusception requiring operative intervention. J Pediatr Surg. 2005 Jan;40(1):281-4. http://www.ncbi.nlm.nih.gov/pubmed/15868598?tool=bestpractice.com [36]van der Laan M, Bax NM, van der Zee DC, et al. The role of laparoscopy in the management of childhood intussusception. Surg Endosc. 2001 Apr;15(4):373-6. http://www.ncbi.nlm.nih.gov/pubmed/11395818?tool=bestpractice.com
Intestinal resection may be necessary for cases complicated by bowel necrosis and perforation.
broad-spectrum antibiotics
Treatment recommended for SOME patients in selected patient group
Broad-spectrum antibiotics covering intra-abdominal pathogens should be administered. Antibiotic treatment should be initiated on clinical diagnosis of shock, perforation, peritonitis, or evidence of bowel wall necrosis.
Administer antibiotics 1 hour before the procedure if possible, and then consider continuing antibiotics after reduction for up to 48 hours if ischemia or significant dilatation is present.
For patients who undergo resection, use routine intestinal prophylactic regimens. Prolonged antibiotic administration is only recommended in cases of perforation or abscess formation.
Antibiotic regimens vary according to local protocols; consult local guidance.
Primary options
clindamycin: neonates: consult specialist for guidance on dose; infants and children: 25-40 mg/kg/day intravenously/intramuscularly given in divided doses every 6-8 hours
and
gentamicin: neonates: consult specialist for guidance on dose; infants and children: 2 to 2.5 mg/kg intravenously/intramuscularly every 8 hours
OR
piperacillin/tazobactam: neonates and infants <2 months of age: consult specialist for guidance on dose; children: 2-8 months of age: 80 mg/kg intravenously every 8 hours; children ≥9 months of age and ≤40 kg: 100 mg/kg intravenously every 8 hours
More piperacillin/tazobactamDose refers to piperacillin component.
OR
cefoxitin: neonates and infants ≤3 months of age: consult specialist for guidance on dose; children >3 months of age: 25 mg/kg intravenously every 4-6 hours
and
vancomycin: neonates: consult specialist for guidance on dose; infants and children: 10 mg/kg intravenously every 6 hours
with contraindications to contrast enema reduction and/or clinically unstable (e.g., shock, suspected perforation, peritonitis, evidence of bowel wall necrosis)
fluid resuscitation + surgical reduction
Adequate intravenous access and correction of hypovolemia with isotonic fluid resuscitation is necessary. In cases where there are contraindications to contrast enema reduction, or where the patient is clinically unstable, surgical reduction is required.
Absolute contraindications to contrast enema reduction include: peritonitis, perforation, toxic colitis, and hypovolemic shock.[28]American College of Radiology. ACR-SPR practice parameter for the performance of pediatric fluoroscopic contrast enema examinations. 2021 [internet publication]. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/fluourconenema-ped.pdf
Relative contraindications include: prolonged symptoms, ultrasound findings of intestinal ischemia or trapped fluid, and marked evidence of bowel obstruction (e.g., abdominal distension, signs on imaging).[28]American College of Radiology. ACR-SPR practice parameter for the performance of pediatric fluoroscopic contrast enema examinations. 2021 [internet publication]. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/fluourconenema-ped.pdf The procedure requires some cooperation from older children, who may not be able to tolerate the discomfort of the procedure.
Traditionally, operative reduction has been performed through an open approach via a right lower quadrant incision. The intussusception is identified and milked out of the intussuscipiens. Laparoscopic surgical techniques may be considered following surgical assessment, although would not be appropriate in clinically unstable patients.
Intestinal resection may be necessary for cases complicated by bowel necrosis and perforation.
broad-spectrum antibiotics
Treatment recommended for SOME patients in selected patient group
Broad-spectrum antibiotics covering intra-abdominal pathogens should be administered. Antibiotic treatment should be initiated on clinical diagnosis of shock, perforation, peritonitis, or evidence of bowel wall necrosis.
Administer antibiotics 1 hour before the procedure if possible, and then consider continuing antibiotics after reduction for up to 48 hours if ischemia or significant dilatation is present.
For patients who undergo resection, use routine intestinal prophylactic regimens. Prolonged antibiotic administration is only recommended in cases of perforation or abscess formation.
Antibiotic regimens vary according to local protocols; consult local guidance.
Primary options
clindamycin: neonates: consult specialist for guidance on dose; infants and children: 25-40 mg/kg/day intravenously/intramuscularly given in divided doses every 6-8 hours
and
gentamicin: neonates: consult specialist for guidance on dose; infants and children: 2 to 2.5 mg/kg intravenously/intramuscularly every 8 hours
OR
piperacillin/tazobactam: neonates and infants <2 months of age: consult specialist for guidance on dose; children: 2-8 months of age: 80 mg/kg intravenously every 8 hours; children ≥9 months of age and ≤40 kg: 100 mg/kg intravenously every 8 hours
More piperacillin/tazobactamDose refers to piperacillin component.
OR
cefoxitin: neonates and infants ≤3 months of age: consult specialist for guidance on dose; children >3 months of age: 25 mg/kg intravenously every 4-6 hours
and
vancomycin: neonates: consult specialist for guidance on dose; infants and children: 10 mg/kg intravenously every 6 hours
recurrence
consideration of evaluation for pathologic lead point + retreatment
Most recurrences after successful reduction of intussusception occur soon after reduction. The recurrence rate of intussusception after contrast enema (air or liquid contrast) reduction is approximately 10% and does not significantly differ based on the type of contrast reduction performed.[37]Daneman A, Navarro O. Intussusception. Part 2: an update on the evolution of management. Pediatr Radiol. 2004 Feb;34(2):97-108. http://www.ncbi.nlm.nih.gov/pubmed/14634696?tool=bestpractice.com The risk of recurrence within 48 hours is low after enema reduction suggesting that patients who appear well should be considered for outpatient management with follow-up.[38]Beres AL, Baird R, Fung E, et al. Comparative outcome analysis of the management of pediatric intussusception with or without surgical admission. J Pediatr Surg. 2014 May;49(5):750-2. http://www.ncbi.nlm.nih.gov/pubmed/24851762?tool=bestpractice.com [39]Gray MP, Li SH, Hoffmann RG, et al. Recurrence rates after intussusception enema reduction: a meta-analysis. Pediatrics. 2014 Jul;134(1):110-9. http://www.ncbi.nlm.nih.gov/pubmed/24935997?tool=bestpractice.com
Surgical reduction has been associated with a recurrence rate of 2% to 5%.[40]Ugwu BT, Legbo JN, Dakum NK, et al. Childhood intussusception: a 9-year review. Ann Trop Pediatr. 2000 Jun;20(2):131-5. http://www.ncbi.nlm.nih.gov/pubmed/10945064?tool=bestpractice.com
Although suspicion for a pathologic lead point must be increased with a recurrent intussusception, successful contrast enema reduction has been advocated. Surgical intervention is reserved for irreducible recurrences and the presence of an identified pathologic lead point.[2]McCollough M, Sharieff GQ. Abdominal pain in children. Pediatr Clin North Am. 2006 Feb;53(1):107-37. http://www.ncbi.nlm.nih.gov/pubmed/16487787?tool=bestpractice.com [37]Daneman A, Navarro O. Intussusception. Part 2: an update on the evolution of management. Pediatr Radiol. 2004 Feb;34(2):97-108. http://www.ncbi.nlm.nih.gov/pubmed/14634696?tool=bestpractice.com
After an infant's third episode of intussusception, a pathologic lead point must be considered. Computed tomography may be useful in evaluation for a pathologic lead point.[19]Plut D, Phillips GS, Johnston PR, et al. Practical imaging strategies for intussusception in children. AJR Am J Roentgenol. 2020 Dec;215(6):1449-63. https://www.doi.org/10.2214/AJR.19.22445 http://www.ncbi.nlm.nih.gov/pubmed/33084362?tool=bestpractice.com
In older children with intussusception, pathologic lead points must be considered. Diseases such as cystic fibrosis and Henoch-Schonlein purpura can cause bowel-wall abnormalities that function as lead points in intussusception.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer