Approach
Information about the child's diet should include specifics of vitamin D and calcium intake. Sunlight exposure should be noted. Review of systems should focus on growth and orthopedic concerns.
Clinical
Rickets is characterized by delayed growth, bone pain, and bone deformity. The type of deformity depends on the biomechanical situation of the extremities at the time when the structural weakness develops. Bone deformities of the forearms and posterior bowing of the distal tibia can occur in infants, whereas exaggerated physiologic bowing of the legs (genu varum) is a finding in toddlers who have started walking. Older children may have valgus or windswept (valgus deformity of one leg and varus deformity of the other) deformities of the legs.[4][5][23] Metaphyseal widening can be seen adjacent to the major joints as well as along the costochondral joints, creating the “rachitic rosary.”
Signs and symptoms of hypocalcemia, such as muscle cramps, muscle weakness, numbness, paresthesias, carpopedal spasm, tetany, and seizures may be present in hypocalcemic rickets.[4][Figure caption and citation for the preceding image starts]: Malnutrition manifested as rickets. Note the bowed legs and enlarged right wristCDC [Citation ends]. [Figure caption and citation for the preceding image starts]: Malnutrition manifested as rickets. Note the bowed legs and kneesCDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Malnutrition manifested as rickets. Note the bowed legs and kneesCDC [Citation ends].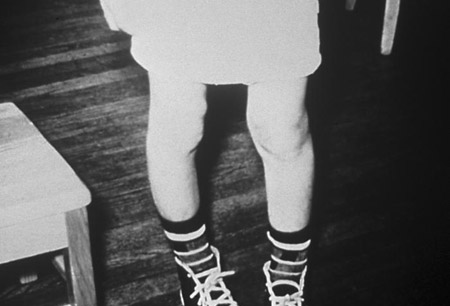
Laboratory
Traditional rickets is caused by a quantitative or qualitative lack of vitamin D. Serum levels of calcium, phosphorus, calcidiol, alkaline phosphatase, parathyroid hormone (PTH), BUN, and creatinine are all measured initially. Calcitriol (1,25-dihydroxyvitamin D) is the active form of vitamin D, but calcidiol (25-hydroxyvitamin D) is preferred for testing as it has a longer half-life and is found at much higher levels in the serum. Urine calcium and phosphorus are also tested initially.[4]
The most common laboratory findings in nutritional rickets (due to vitamin D deficiency) are decreases in serum calcium, serum phosphorus, calcidiol, calcitriol, and urinary calcium, with elevated serum PTH and alkaline phosphatase and urinary phosphorus. Rickets is unlikely if both serum inorganic phosphorus and PTH levels are normal.[4][5]
Hypophosphatemic rickets is caused by renal phosphate wasting. Serum phosphate levels are low and urine phosphate levels are high. Serum alkaline phosphatase levels will be elevated. Serum levels of calcium, PTH, calcidiol, and calcitriol are normal in hypophosphatemic rickets. Vitamin D deficiency is common and can complicate the presentation of hypophosphatemic rickets. Vitamin D deficiency must be corrected before the diagnosis of hypophosphatemic rickets can be made. A low percent tubular reabsorption of phosphate (TRP) in the absence of vitamin D deficiency is diagnostic of hypophosphatemic rickets.[24]
Imaging
A radiograph of a long bone showing cupping, splaying, and fraying of the metaphysis is required for diagnosis. Widening of the epiphyseal plate and loss of definition of the zone of provisional calcification at the epiphyseal/metaphyseal interface are the early signs of rickets.
The distal ulna is the site that best demonstrates the early signs of impaired mineralization, and the metaphyses above and below the knees are more useful sites in older children.[4][Figure caption and citation for the preceding image starts]: Right wrist of a patient with vitamin D deficient rickets before treatment. His right wrist x-ray showed sclerotic and widened end plates of the radius and ulna (arrows)Seerat I, Greenberg M. Hypocalcaemic fit in an adolescent boy with undiagnosed rickets. BMJ Case Reports 2010; doi:10.1136/bcr.10.1136/bcr10.2008.1153 [Citation ends]. [Figure caption and citation for the preceding image starts]: Right wrist of a patient with vitamin D deficient rickets after treatment (arrows)Seerat I, Greenberg M. Hypocalcaemic fit in an adolescent boy with undiagnosed rickets. BMJ Case Reports 2010; doi:10.1136/bcr.10.1136/bcr10.2008.1153 [Citation ends].
[Figure caption and citation for the preceding image starts]: Right wrist of a patient with vitamin D deficient rickets after treatment (arrows)Seerat I, Greenberg M. Hypocalcaemic fit in an adolescent boy with undiagnosed rickets. BMJ Case Reports 2010; doi:10.1136/bcr.10.1136/bcr10.2008.1153 [Citation ends]. [Figure caption and citation for the preceding image starts]: Bony changes (arrows) before (bottom panels) and after (top panel) treatment of ricketsBangalore H, Bisht S, Inusa B. Rickets and tracheobronchomalacia. BMJ Case Reports 2009; doi:10.1136/bcr.01.2009.1422 [Citation ends].
[Figure caption and citation for the preceding image starts]: Bony changes (arrows) before (bottom panels) and after (top panel) treatment of ricketsBangalore H, Bisht S, Inusa B. Rickets and tracheobronchomalacia. BMJ Case Reports 2009; doi:10.1136/bcr.01.2009.1422 [Citation ends].
Use of this content is subject to our disclaimer