Approach
Characteristic history and skin changes, if still present on clinical examination, are often sufficient to diagnose PLE. Skin biopsy is reserved for rare variants of PLE and to exclude more severe differential diagnoses, such as lupus erythematosus.
History
Typically, patients complain of the development of itchy, erythematous patches, followed by papules, plaques, or vesicles in sun-exposed areas, primarily on the chest, neck, and extensor surfaces of the arms and legs; after intensive, repeated sun exposure.
Lesions appear between several hours to a few days after exposure, depending on the individual threshold and intensity of ultraviolet radiation (UVR) exposure.
Skin changes last several days and remission occurs spontaneously without leaving any permanent changes.[1][10]
The clinical picture for PLE may vary between patients; however, it remains monomorphous in the same patient over the course of the disease.[1][10][38]
Young women and adolescents are more commonly affected.[1][20]
Most patients experience a so-called natural hardening (habituation) over the course of the year and at the end of the summer may tolerate high UVR doses, without provoking PLE lesions.[5][39]
PLE is a chronic condition that recurs annually and persists over many years or even decades.
Physical examination
On a patient's individual predilection sites (sites where PLE lesions recur), itchy, erythematous papules, plaques, or vesicles are typically present. Frequently affected areas include the V-shaped neck area and the extensor surfaces of the arms and legs.[Figure caption and citation for the preceding image starts]: Small papular type of PLE with densely aggregated pinpoint size papules on the faceImage provided by Dr Hadshiew; used with permission [Citation ends].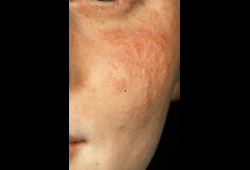 [Figure caption and citation for the preceding image starts]: Typical presentation of extensive plaque-type PLE on the chestImage provided by Dr Hadshiew; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Typical presentation of extensive plaque-type PLE on the chestImage provided by Dr Hadshiew; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Papular-vesicular type on the commonly affected V-neck areaImage provided by Dr Hadshiew; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Papular-vesicular type on the commonly affected V-neck areaImage provided by Dr Hadshiew; used with permission [Citation ends].
Phototesting
Phototesting involves assessment of the minimal erythema doses (MED) for ultraviolet A (UV-A) and ultraviolet B (UV-B) to detect abnormal photosensitivity. For patients with PLE, phototesting is requested only when the diagnosis is not clear. In PLE this test is typically normal. Additional testing comprises photoprovocation with monochromator wavelengths of UV-A and UV-B, to induce specific PLE lesions after repeated exposure.[1] This is done to provoke the typical individual lesions, which can be biopsied in order to confirm the diagnosis on histology.
A combined photoprovocation might be necessary in individual patients where the history suggests different action spectra or where monochromator UV-A and UV-B photoprovocation tests alone yield negative results. This procedure affects both confirmation of the diagnosis (by successfully provoking PLE lesions) and decisions on potential prophylactic measures (such as the use of both UV-A and UV-B for hardening via phototherapy).
Where initial phototests are negative (especially for darker skin types), higher, repeated UVR doses (especially for UV-A) may be needed to elicit typical PLE symptoms.[Figure caption and citation for the preceding image starts]: Pronounced bullous PLE after photoprovocation (3 x 100 J/cm^2 UV-A)Image provided by Dr Hadshiew; used with permission [Citation ends].
Skin biopsy
PLE is a clinical diagnosis and biopsy is rarely necessary except to exclude more severe conditions such as SLE.
Typical histologic findings in PLE are:[45]
Perivascular lymphocytic infiltration that is more pronounced in the upper dermal vascular plexus
Subepidermal edema
Minimal epidermal changes with vacuolar degeneration of the basement membrane, focal spongiosis of the lower epidermis, and scarce exocytosis.
Clinical subtypes and variants also differ in their histological picture.
The hemorrhagic type shows extravasation of erythrocytes in the stratum papillare.
Findings for plaque type PLE include band-like lymphocytic infiltration in the upper dermis and pronounced subepidermal edema.
The rare erythema exudativum multiforme type histopathologically resembles the plaque type, but tends to have more pronounced subepidermal edema.
The vesiculobullous variant shows a marked spongiosis with formation of vesicles and amplification of subepidermal edema to the extent of bullous changes with focal separation of the epidermis from the dermis.
The ictus type resembles the papular variant; however, focal necrosis of the epidermis may occur.
Additionally, neutrophils or eosinophils may be found.[45]
Use of this content is subject to our disclaimer