History and exam
Key diagnostic factors
common
diabetes
Patients with diabetic retinopathy usually have diabetes diagnosed before retinopathy is identified. Higher-risk features include young-onset diabetes requiring insulin treatment, long duration of diabetes, or poor glycaemic control.
Other diagnostic factors
common
microaneurysms
Round intraretinal lesions, 10 to 100 micrometres in diameter, red or occasionally cream/white in colour, and may be associated with haemorrhage, exudation, and retinal thickening.
A feature of non-proliferative diabetic retinopathy (NPDR), but may also occur in proliferative diabetic retinopathy (PDR). If present in the macular area, may be associated with macular oedema.[72]
The number of microaneurysms is an important predictor of the risk of progression from NPDR to PDR retinopathy, although in eyes with extensive capillary non-perfusion the number may fall.[72][Figure caption and citation for the preceding image starts]: Fluorescein angiogram of non-proliferative diabetic retinopathy: microaneurysms (red arrow), intraretinal microvascular abnormalities (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].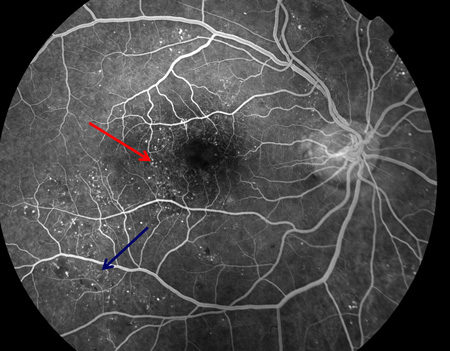
cotton wool spots
Appear as localised white elevations of the nerve fibre layer, within which nerve fibre striations may be visible.
A feature of non-proliferative diabetic retinopathy, but may also occur in proliferative diabetic retinopathy (PDR).
They represent the arrest of axoplasmic material at the margin of a microvascular infarct and are predictive of progression to PDR.[73][Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: cluster haemorrhages (red circle), cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].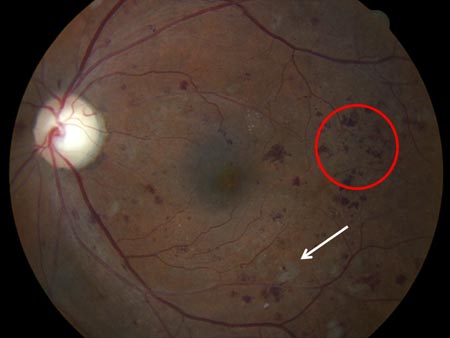 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].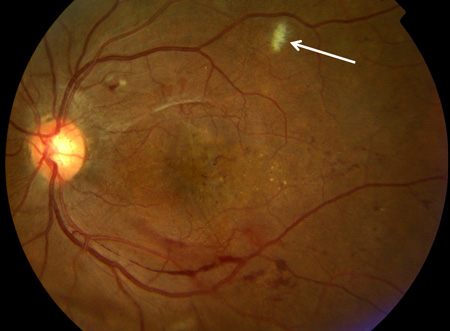
intraretinal haemorrhage
The form (flame, dot/blot, or cluster) is dictated by the layer of the retina within which the haemorrhage lies.
May be present in non-proliferative diabetic retinopathy (NPDR). Presence in the macular area may be associated with macular oedema.
The presence of numerous (>20) haemorrhages in four quadrants of the retina is indicative of severe NPDR.[1] It is predictive of progression to proliferative diabetic retinopathy.[73][Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: flame haemorrhage (red arrow), venous beading (white rectangle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].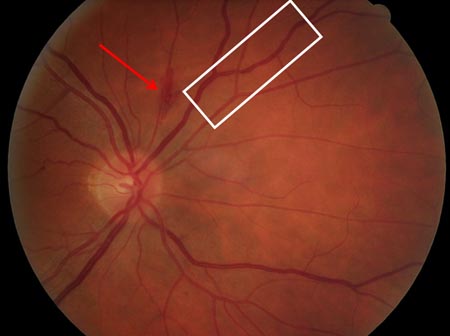 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].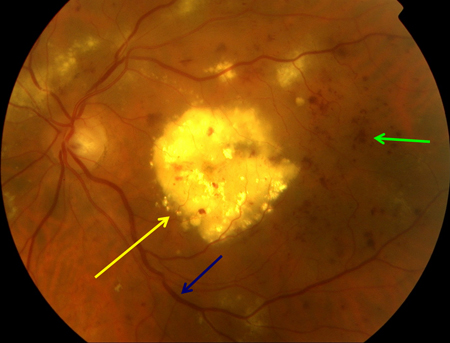 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: blot haemorrhage (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: blot haemorrhage (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
lipid exudates
Creamy yellow dots, flecks, or plaques of exudate represent precipitation of extravasated lipoprotein at the border between thickened and non-thickened retina.
A feature of non-proliferative diabetic retinopathy but may also occur in proliferative diabetic retinopathy (PDR).
They are not predictive of progression to PDR, but their presence in the macular area suggests macular oedema.[73][Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: thickened retina (white ellipse), exudate (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].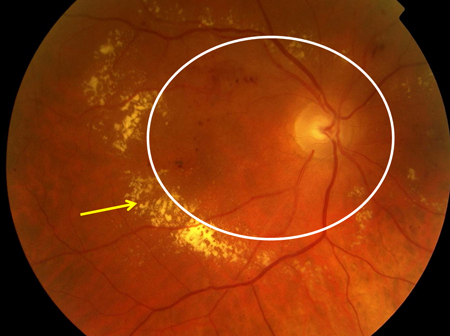
macular oedema
Ophthalmoscopically, macular oedema appears as elevation or thickening of the central macula.
Occurs in non-proliferative diabetic retinopathy or proliferative diabetic retinopathy and arises from intraretinal oedema.
It is best identified by optical coherence tomography, although it may be inferred from the loss of the foveal reflex, central cystoid spaces, or surrounding hard exudate as seen by direct ophthalmoscopy.
It is commonly associated with the presence of haemorrhage, microaneurysms, and hard exudate in the macular area.[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate (yellow arrow), microaneurysms (red arrow), thickened retina (white circle), cystic change at macula (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].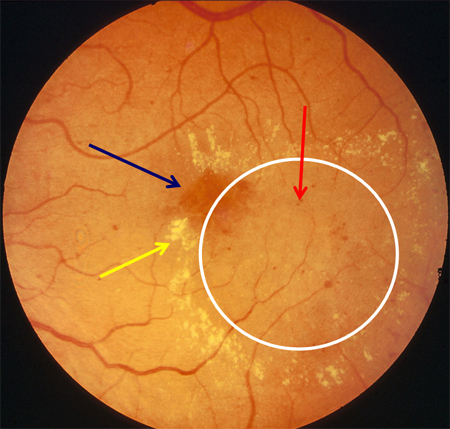 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: cotton wool spot (white arrow), thickened retina (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: cotton wool spot (white arrow), thickened retina (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].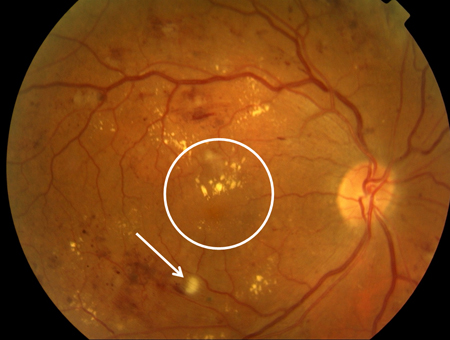 [Figure caption and citation for the preceding image starts]: Optical coherence tomography in macular oedema: loss of central foveal depression (yellow arrow), accumulation of fluid within cystoid spaces at fovea (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Optical coherence tomography in macular oedema: loss of central foveal depression (yellow arrow), accumulation of fluid within cystoid spaces at fovea (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].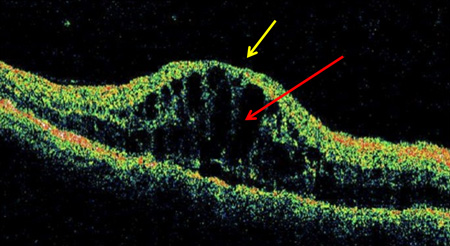
uncommon
venous beading
In contrast to the generalised venous dilatation of early retinopathy, venous beading refers to localised dilatation of veins, in extreme cases leading to segmentation. It occurs where capillary non-perfusion extends up to the vein wall, causing it to lose its glial support.
A feature of non-proliferative diabetic retinopathy (NPDR) but may also occur in proliferative diabetic retinopathy (PDR). Its presence in two quadrants of retina is indicative of severe NPDR.[1] It is a potent predictor of progression to PDR.[73][Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate (yellow arrow), microaneurysms (red arrow), venous dilatation (blue arrow), cotton wool spot (white arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].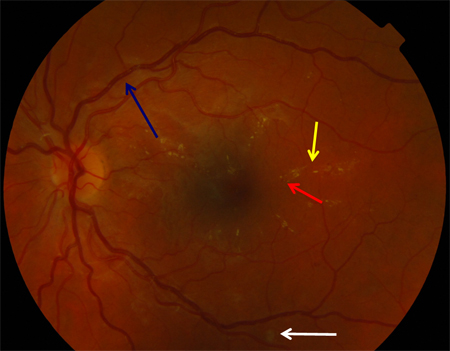 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy with macular oedema: exudate plaque (yellow arrow), cluster haemorrhage (green arrow), venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].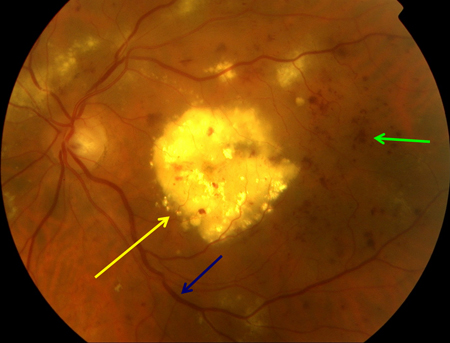 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].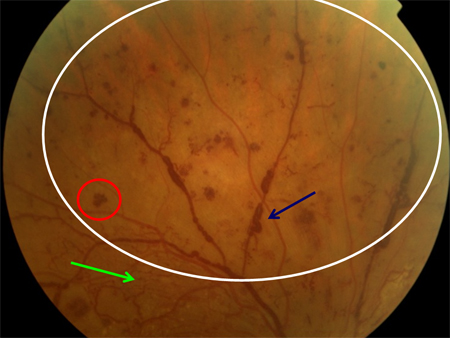 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].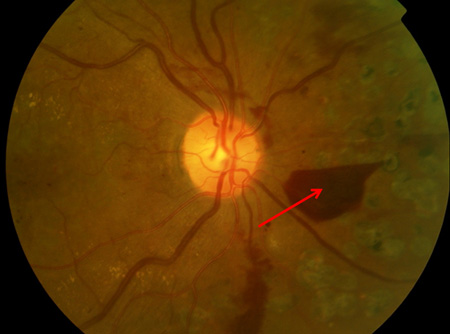
intraretinal microvascular abnormalities
Occur in both non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR) and consist of vascular elements within the retina that branch with a frequency, number, and angulation unlike normal retinal vessels.
Within the retina, they typically lie between artery and vein, and unlike new vessels do not overlie other vessels and are not associated with vitreous haemorrhage.
Their presence in one quadrant of retina is indicative of severe NPDR.[1] Their presence is a predictor of progression to PDR.[73][Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: optic disc new vessels (red arrow), intraretinal microvascular abnormality (IRMA; green arrow), cotton wool spot (white arrow), venous beading and segmentation (red rectangle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].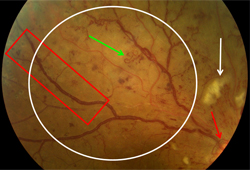 [Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-proliferative diabetic retinopathy: intraretinal microvascular abnormality (IRMA; green arrow), venous beading and segmentation (blue arrow), cluster haemorrhage (red circle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].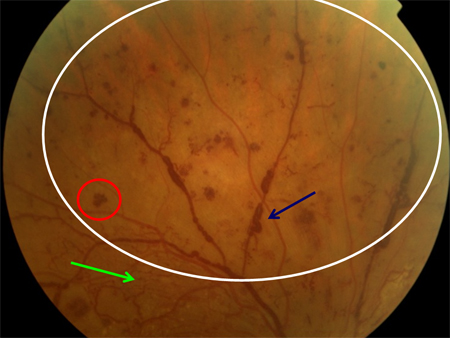
optic disc neovascularisation
Occurs in proliferative diabetic retinopathy and consists of a vascular network, often overlying other retinal vessels, with a branching structure unlike that of normal retinal vessels, arising within 1500 micrometres of the optic disc.
Commonly associated with pre-retinal haemorrhage, vitreous haemorrhage, intraretinal microvascular abnormalities, and venous beading.
Risk of severe visual loss in untreated eyes at 2 years ranges from 13%, for patients with mild new vessels on optic disc (NVD) without vitreous haemorrhage, to 40%, for those with moderate to severe NVD and vitreous haemorrhage.[74][Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].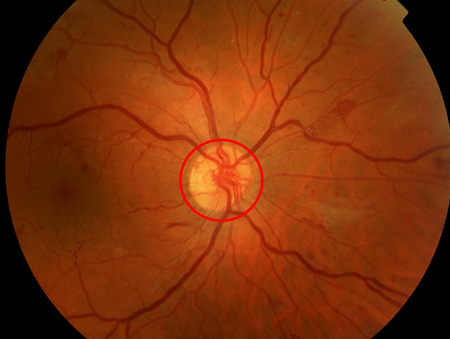 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle), retrohyaloid haemorrhage (red arrow), new vessels elsewhere with fibrosis (white arrow), dot and blot haemorrhage (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle), retrohyaloid haemorrhage (red arrow), new vessels elsewhere with fibrosis (white arrow), dot and blot haemorrhage (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].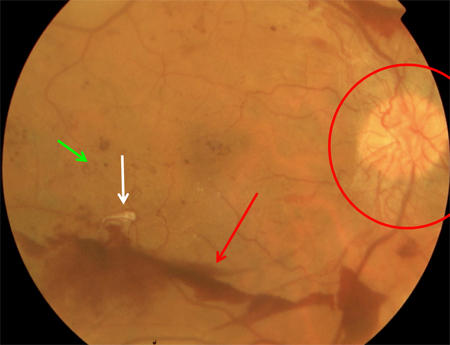 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: macular laser burns (black arrow), misty vitreous haemorrhage (blue arrow), clot within vitreous haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: macular laser burns (black arrow), misty vitreous haemorrhage (blue arrow), clot within vitreous haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].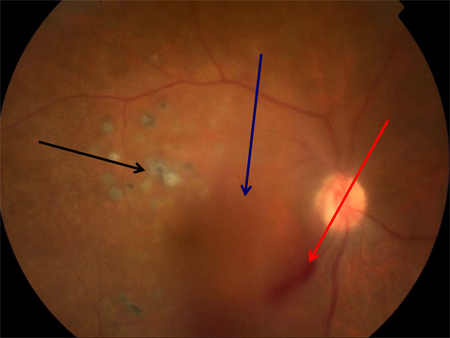 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: optic disc new vessels (red arrow), intraretinal microvascular abnormality (IRMA; green arrow), cotton wool spot (white arrow), venous beading and segmentation (red rectangle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: optic disc new vessels (red arrow), intraretinal microvascular abnormality (IRMA; green arrow), cotton wool spot (white arrow), venous beading and segmentation (red rectangle), featureless retina suggestive of capillary non-perfusion (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].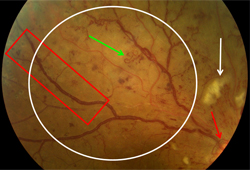 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].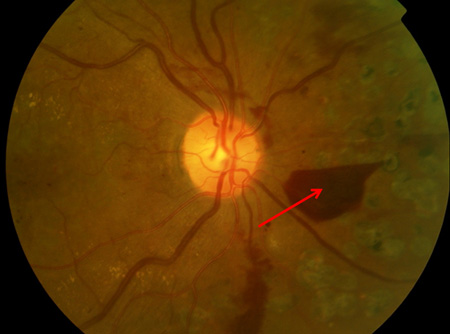
retinal neovascularisation
Occurs in proliferative diabetic retinopathy and consists of a vascular network, often overlying other retinal vessels, with a branching structure unlike that of normal retinal vessels, arising anywhere in the retina >1500 micrometres from the optic disc.
Commonly associated with pre-retinal haemorrhage, vitreous haemorrhage, intraretinal microvascular abnormalities, and venous beading.
Risk of severe visual loss in untreated eyes at 2 years ranges from 8%, for patients with mild new vessels elsewhere in the retina (NVE) without vitreous haemorrhage, to 36%, for those with moderate to severe NVE and vitreous haemorrhage.[74][Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels on the optic disc (red circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].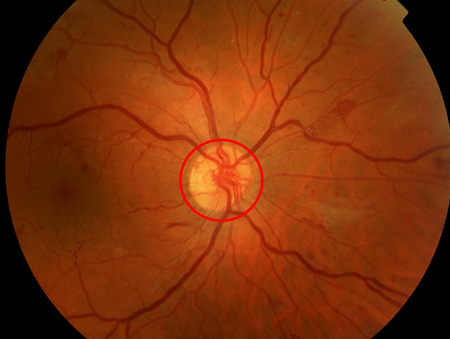 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (red arrow), venous beading (blue arrow), intraretinal microvascular abnormality (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (red arrow), venous beading (blue arrow), intraretinal microvascular abnormality (green arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].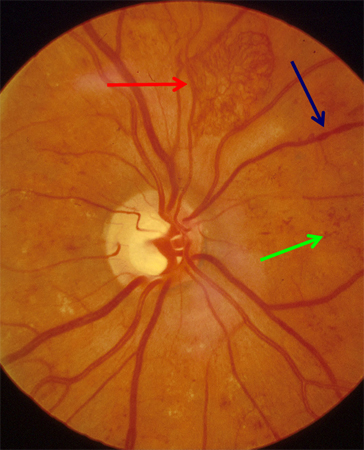 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].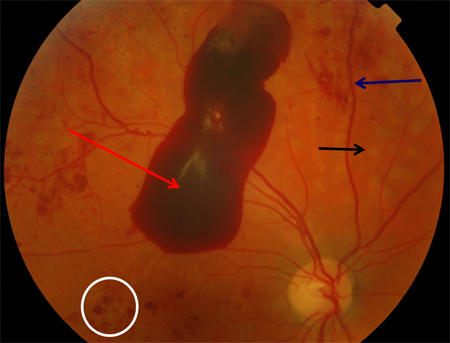 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction towards optic disc and consequent total retinal detachment (white block arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction towards optic disc and consequent total retinal detachment (white block arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].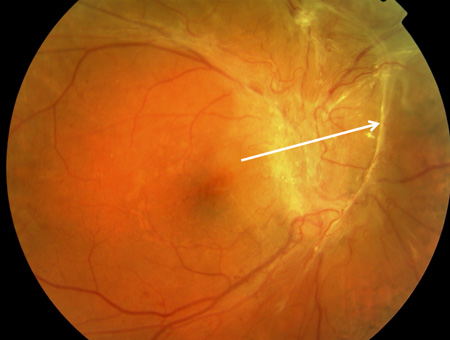
pre-retinal or vitreous haemorrhage
Blood anterior to retina may take on a flat-topped or boat-shaped appearance in the pre-retinal space, may form a rounded collection, or, if within the vitreous cavity, causes a more or less homogeneous opacity obstructing the fundus view.
Both of these variants overlie retinal blood vessels and suggest proliferative retinopathy.
When associated with new vessels on the optic disc or moderate to severe new vessels elsewhere, they indicate an eye at high risk of visual loss and in need of urgent pan-retinal photocoagulation.[74][Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: nerve fibre layer haemorrhage (yellow arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].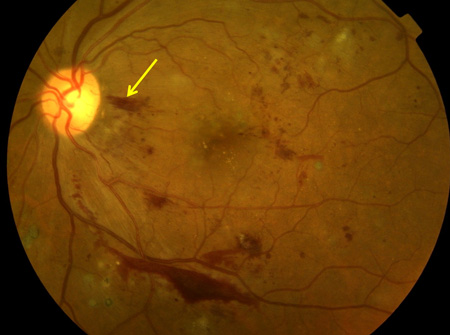 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: venous beading (blue arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].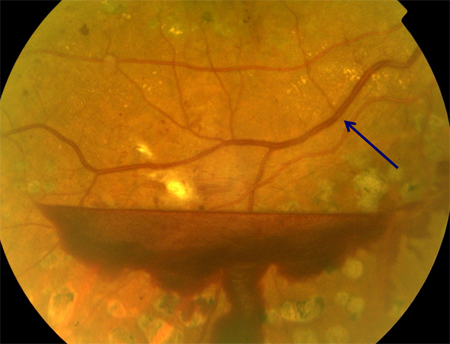 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: extensive vitreous haemorrhage obscuring most of fundus (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: extensive vitreous haemorrhage obscuring most of fundus (white circle)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].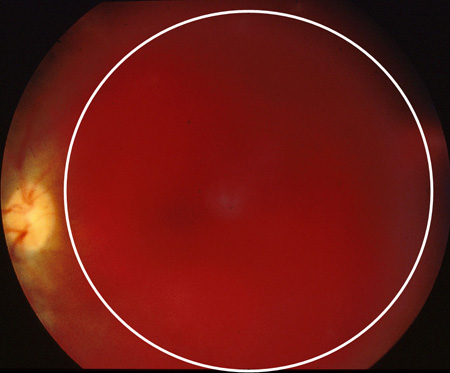 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: retrohyaloid haemorrhage (red arrow), venous beading (blue arrow), cluster haemorrhage (white circle), pan-retinal laser burns (black arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].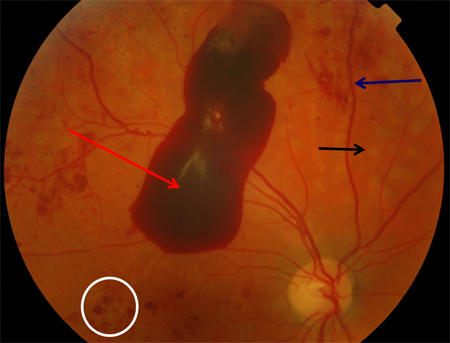 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (white arrow), vitreous (intra-gel) haemorrhage (green arrow), retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: new vessels elsewhere (white arrow), vitreous (intra-gel) haemorrhage (green arrow), retrohyaloid haemorrhage (red arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].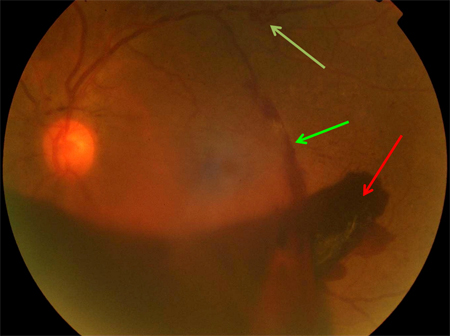
retinal detachment
Occurs in advanced proliferative diabetic retinopathy and is associated with a greyish elevation of the retina, typically concave if purely tractional or convex if vitreoretinal traction tears the retina, allowing recruitment of subretinal fluid (traction-rhegmatogenous detachment). Some tractional elevations of the retina represent schisis rather than detachment.[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction towards optic disc and consequent total retinal detachment (white block arrow)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].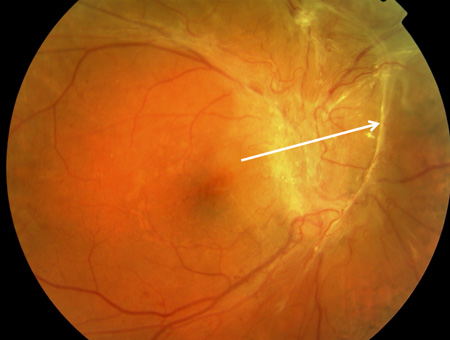 [Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction tear (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Proliferative diabetic retinopathy: traction tear (white ellipse)Courtesy of Moorfields Photographic Archive; used with permission [Citation ends].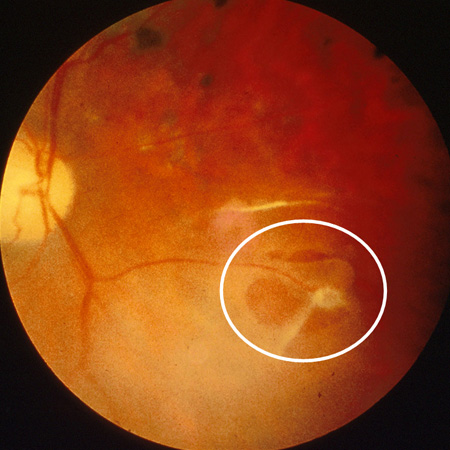
Risk factors
strong
longer duration of diabetes
In the Wisconsin Epidemiological Study of Diabetic Retinopathy, retinopathy prevalence in patients aged <30 years at the time of diagnosis of diabetes was 17% in those who had diabetes (type 1 and 2) for <5 years and 98% in those who had diabetes for >15 years.[8] Prevalence in patients aged >30 years at time of diagnosis was 29% in those who had diabetes for <5 years, and 78% in those who had diabetes >15 years.[9]
poor glycaemic control
The UK Prospective Diabetes Study in people with type 2 diabetes showed a 25% reduction in microvascular end points, including retinal photocoagulation or vitreous haemorrhage, with intensive treatment compared with conventional treatment (10-year haemoglobin A1c [HbA1c] 7% vs. 8%, respectively).[48] The ACCORD-EYE study in type 2 diabetes showed a 33% reduction in 3-step retinopathy progression (HbA1c 6.4% vs. 7.5%).[49] The Diabetes Control and Complications Trial of type 1 diabetes showed a 76% reduction in the incidence of retinopathy and a 54% reduction in progression with intensive treatment compared with conventional treatment (HbA1c approximately 7% vs. 9%).[50] A review concluded in people with diabetic retinopathy, increased HbA1c is likely to be associated with progression to proliferative diabetic retinopathy.[51]
[  ]
]
elevated lipid levels
In the ACCORD-EYE study, 1593 patients with type 2 diabetes and HbA1c <7.5% were randomised to fenofibrate plus statin or placebo plus statin. Retinopathy progression was reduced by 40% in the fenofibrate group compared with placebo.[49] A meta-analysis concluded that statin use reduced the incidence and progression of diabetic retinopathy and diabetic macular oedema, and the need for intervention with laser, intravitreal therapy, and vitrectomy.[52]
hypertension
The UK Prospective Diabetes Study (UKPDS) in people with type 2 diabetes demonstrated a 34% reduction in 2-step retinopathy progression using the modified Early Treatment Diabetic Retinopathy Study (ETDRS) final scale, and a 47% reduction in 3-line decline in ETDRS visual acuity using the ETDRS chart, following improved blood pressure control.[53] This effect was not apparent in the ACCORD-EYE study, where intensive blood pressure control did not affect retinopathy progression or visual acuity.[54] It should be noted, however, that in the ACCORD-EYE study, only patients at high cardiovascular risk were studied, and targets for intensive control were stringent: a systolic blood pressure <120 mmHg for intensive treatment and <140 mmHg for less intensive. In the UKPDS, patients with a history of certain cardiovascular events were specifically excluded, and target blood pressures were less stringent: <150/85 mmHg for intensive control and <180/105 for less intensive. No studies on a similar scale have been performed in people with type 1 diabetes.
weak
renal disease
ethnicity
pregnancy
cataract surgery
Use of this content is subject to our disclaimer