Approach
The exact diagnosis of uveitis can be extremely challenging given the vast array of presentations and etiologies. While clinical examination and laboratory testing are important for the diagnosis of uveitis, making a sound differential diagnosis of the underlying etiology also requires careful attention to the patient's presentation and history, and to demographic information. Bilaterality is more commonly seen in systemic conditions, whereas idiopathic and herpetic uveitis is more commonly unilateral. The nongranulomatous versus granulomatous nature of the presentation will also help to narrow further the differential diagnosis of the underlying etiology. Early referral to an ophthalmologist with experience in uveitis is essential.
There are several pathologic entities that mimic uveitis, known as "masquerade syndromes", and each may have an associated intraocular cellular reaction. None of these are related to either autoimmune inflammation or ocular infection. Broadly, they can be classified as neoplastic and non-neoplastic. Please see the "Differentials diagnosis" section for more information.
Ocular symptoms
Symptoms in uveitis generally depend on the location of the inflammation in the uvea, which is useful in differentiating between anterior and posterior uveitis. However, a thorough eye examination is the only way to confirm the diagnosis. A patient’s symptoms are less useful in further classifying the disease when dealing with possible intermediate or panuveitis.
Patients with anterior uveitis often complain of ocular symptoms, including pain, redness, photophobia, and tearing. Patients may also have unilateral, dull pain that extends from the eye to the surrounding orbit. The area may be tender to palpation through the eyelid. Common causes of anterior uveitis include human leukocyte antigen-B27 (HLA-B27)-associated iritis (including ankylosing spondylitis, psoriatic arthritis, and reactive arthritis), Behçet disease, juvenile idiopathic arthritis (JIA), Fuchs heterochromic iridocyclitis, and masquerade syndromes (disorders that may mimic uveitis).
In contrast, patients with posterior uveitis usually have a painless presentation. Decreased vision, floaters, photopsia (a perception of flashes of light), or asymptomatic presentation may occur in posterior uveitis, although this is highly variable depending on the location, severity, and etiology of the inflammation. Common causes of posterior uveitis include toxoplasmosis retinochoroiditis, herpes simplex virus (HSV) retinitis, tuberculosis (TB) choroiditis, sarcoidosis, and Vogt-Koyanagi-Harada syndrome (a multisystem autoimmune disorder characterized by chronic uveitis with skin, neurologic, and auditory manifestations).
Most causes of uveitis result in bilateral disease. However, cases of unilateral uveitis are often seen in post-surgical uveitis, HSV-associated uveitis, and most parasitic diseases. Therefore, a bilateral versus unilateral presentation can assist in determining the etiology.
Ocular symptom onset and duration
Onset and duration of the ocular symptoms offer clues to the etiology. Acute uveitis, characterized by sudden onset (over hours or days) and limited duration (≤3 months' duration), is seen in certain uveitis-associated diseases. Most forms of anterior uveitis present acutely, and acute anterior uveitis is the most common form of acute uveitis. Common causes of acute anterior uveitis include HLA-B27-associated disorders, systemic disease (e.g., sarcoidosis, Behçet disease), infection, drug reactions, and trauma. Acute anterior uveitis may also be idiopathic, or mimicked by a masquerade syndrome.[15] Post-surgical bacterial endophthalmitis (a form of infectious panuveitis) also usually presents acutely.
Chronic uveitis is defined as persistent uveitis (>3 months' duration) characterized by relapse within 3 months of therapy termination.[2] Several types of uveitis, such as JIA, tuberculous uveitis, and Fuchs heterochromic cyclitis, may present this way. Common causes of chronic anterior uveitis include systemic disease (e.g., JIA, sarcoidosis), Fuchs heterochromic cyclitis, infection, chronic idiopathic anterior uveitis, and postoperative inflammation. Chronic anterior uveitis is not associated with HLA-B27.[15] Chronic intermediate uveitis is often idiopathic, or may be associated with multiple sclerosis, sarcoidosis, syphilis, Lyme disease, or ocular lymphoma.[16] Chronic posterior uveitis may be caused by an infection, including syphilis, TB, Lyme disease, or fungal, viral, or parasitic infection. It may be associated with many systemic diseases, including sarcoidosis, Behçet disease, or Vogt-Koyanagi-Harada syndrome, or it may be associated with ocular syndromes such as sympathetic ophthalmia or birdshot chorioretinopathy.[16]
Recurrent uveitis, characterized by repeated episodes separated by disease inactivity ≥3 months, whether on or off treatment, may be seen in many types of chronic uveitis, including Fuchs heterochromic cyclitis and sarcoid-associated uveitis.
Systemic symptoms
Uveitis may occur as a manifestation of a disease with extra-ocular involvement, whether an infectious disease, an autoimmune-mediated systemic disease, or a masquerade syndrome.[10] Other uveitis syndromes may be confined primarily to the eye. Therefore, a good review of systems should help to narrow the possible etiologies.
Arthritis is an important systemic symptom in relation to uveitis patients. Symptoms such as pain or stiffness of the hands, wrists, fingers, toes, lower back, spine, or any weight-bearing joints should be sought. These symptoms may be found in patients with JIA, HLA-B27-associated disorders, rheumatoid arthritis, and systemic lupus erythematosus (SLE).
Rashes can be a systemic sign found in uveitis-associated diseases such as Lyme disease, syphilis, SLE, Kawasaki disease, and drug or hypersensitivity reactions.
Gastrointestinal disease, suggested by abdominal discomfort, nausea, vomiting, diarrhea, or melena, may point to Crohn disease or ulcerative colitis. Behçet disease and Whipple disease may also have gastrointestinal manifestations.
Oral lesions (Behçet disease, inflammatory bowel disease), genital lesions (Behçet disease, syphilis), headache (Behçet disease, Vogt-Koyanagi-Harada syndrome), neurological symptoms (multiple sclerosis, Behçet disease), and pulmonary findings (TB) may also be useful in diagnosis.
The absence of systemic symptoms may also prove useful in diagnosis. A lack of systemic findings is seen in uveitic syndromes confined primarily to the eye, including acute posterior multifocal placoid pigment epitheliopathy (APMPPE), Fuchs heterochromic cyclitis, birdshot choroidopathy (a bilateral inflammatory disease affecting the choroid layer), and pars planitis.
[Figure caption and citation for the preceding image starts]: Comparison of common symptoms and causes of anterior and posterior uveitisCreated by John Huang, MD, CPE [Citation ends].
Medical, ocular, and medication history
The patient’s past medical history (including past ocular history, previous illnesses, and medications) and family history may provide crucial information.
Any previous episode and treatment of uveitis should be documented to determine the duration of the disease and/or to determine if the current presentation is a relapse of an existing condition. Documentation of previous disease course and treatments may help to classify the disease and guide treatment. History of past ocular surgeries or trauma that may be associated with the current presentation is also important. Existing ocular conditions including glaucoma, cataracts, and cystoid macular edema should also be discussed and may be related to the current presentation.
It is important to know if a patient has been diagnosed with any prior illness known to be associated with uveitis, because the presentation could be a manifestation of the underlying disease. History of any autoimmune disease, infectious disease, or neoplastic and paraneoplastic disorders with possible associated uveitis should be sought.
Uveitis secondary to an inflammatory response to medications is rare, but a careful review of a patient’s medications may help with the diagnosis. Drug-induced uveitis is most commonly seen with the use of rifabutin, used to treat TB and other atypical mycobacterial infections. Cidofovir, an antiviral agent used to treat cytomegalovirus (CMV) in AIDS, has also been shown to cause uveitis. Protease inhibitors used in the treatment of AIDS, particularly indinavir, have also been associated with uveitis. Because all of these drugs are used in patients with HIV, which is itself a potential cause of anterior uveitis, determining the exact etiology may be difficult in these patients. However, most drug-related uveitis responds well to topical corticosteroid treatment, often making the diagnosis of drug-induced uveitis possible shortly after initiation of treatment.
Family history
Family history is important since many autoimmune disorders have a genetic predisposition and are seen more commonly in family members. In addition, many infectious diseases can be transmitted congenitally and may underlie the uveitis.
HLA-B27-associated iridocyclitis as seen in ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and inflammatory bowel disease is seen in families with HLA-B27 encoded in the major histocompatibility complex on chromosome 6. Birdshot retinochoroidopathy is associated with HLA-A29. Patients with known HLA correlations or those with a family history of an HLA-related disease may be at increased risk for associated conditions.
TORCH (Toxoplasmosis, Other agents, Rubella, CMV, HSV) syndrome covers the common list of perinatal infections associated with congenital infection and associated ocular manifestations. Toxoplasmosis is an example of a disease causing uveitis by congenital transmission. This disease may be passed from mother to child, leading to ocular disease in the child. Additional common congenital infections include syphilis and HIV.
Demographic information in relation to disease risk
Age, sex, ancestry, social habits, sexual habits, and geographic and occupational exposure risks are important factors.
Age:
The age of a patient may be the most useful demographic consideration when classifying uveitis, given that certain diseases often present in certain age groups:
Childhood uveitis, although less commonly seen than uveitis in older patients, may be seen in the pediatric population associated with JIA, HLA-B27-associated disorders, Lyme disease, toxocariasis, and retinoblastoma.[17]
In young adults, uveitis most often occurs in HLA-B27-associated uveitis, Fuchs heterochromic iridocyclitis, multiple sclerosis, Behçet disease, APMPPE, and pars planitis.
Middle-aged patients with uveitis often have ocular disease associated with sarcoidosis, SLE, birdshot retinochoroidopathy, and Vogt-Koyanagi-Harada syndrome.
Older adults rarely present with primary uveitis. This may be related to the overall decreased immune response in the older population. One of the rare instances of an autoimmune disease in older adults is giant cell arteritis. In patients with chronic persistent intraocular inflammation with poor response to treatment, intraocular lymphoma, other malignancies, and masquerade syndromes should be high on the list of possible causes.
Despite these guidelines, it is important to consider that certain causes may present at any age.
Sex:
Although many causes of uveitis affect the sexes equally, certain types show predominance in either men or women. Reactive arthritis, ankylosing spondylitis, and Behçet disease are more commonly seen in men. As a result of lifestyle differences, men are also more commonly found to have traumatic iritis, fungal endophthalmitis (a form of infectious panuveitis), and sympathetic ophthalmia, resulting from trauma or intravenous drug use. In contrast, JIA and SLE are 2 to 3 times and 7 to 15 times more common, respectively, in females than in males.
Ancestry:
Some systemic diseases associated with uveitis are found to be much more common in certain ethnic groups. Examples include HLA-B27-associated iritis, including ankylosing spondylitis, reactive arthritis, and psoriatic arthritis, which are more common in white people. Sarcoidosis is 3 to 4 times more common in black people. Behçet disease is seen most commonly in the Turkish population and is very common in Asia and Middle Eastern countries compared with North America and Europe. Vogt-Koyanagi-Harada syndrome is the second leading cause of uveitis in Japan after Behçet disease and is seen most commonly in Asian and Native American patients.
Sexual and social habits:
Consideration of sexual and social habits may uncover conditions that could have exposed the patient to infectious causes of uveitis.
Sexual behavior is important because homosexual and young, sexually active males are more likely to contract HIV and other AIDS-related opportunistic infections. Common HIV-associated manifestations include CMV retinitis, Pneumocystis carinii choroiditis, TB-associated uveitis, toxoplasmosis retinochoroiditis, and candida endophthalmitis.
Sexually active people are more likely to acquire sexually transmitted infections, such as syphilis, gonorrhea, and HSV, that can cause a primary infectious uveitis. Chlamydia, the most common sexually transmitted infection, may trigger the HLA-B27-associated iritis in reactive arthritis. In these cases, it is important to gather a full sexual history, including sexual practices, current genitourinary symptoms, and previous sexually transmitted infections.
Other social habits may reveal further exposure risks of a uveitis patient. Intravenous drug users are at increased risk for HIV and all opportunistic infections. Patients with a history of ingesting raw or undercooked pork are at increased risk of ocular toxoplasmosis. Patients who have ingested unpasteurized milk may be exposed to Brucella. Patients with cats are at increased risk of exposure to feces containing Toxoplasma gondii. Ocular toxocariasis may also be contracted from cats or dogs carrying this parasite. Bartonella henselae, which causes cat scratch disease, may also be transmitted to patients with exposure to cats.
Environmental exposure:
Environmental exposures, whether due to geographic location, recent travel, occupation, or contact with an infected person, are important when considering several infectious causes of uveitis.
Geographic location and history of recent travel may be important. Histoplasmosis is endemic to the Mississippi-Ohio-Missouri River valleys and must be considered in patients from that area and in those who have recently traveled there. Coccidioidomycosis can be acquired by visiting or living in the southwestern parts of the US. Dysentery, TB, malaria, and leprosy are other examples of infectious diseases that may be acquired during travel or in endemic countries.
Occupational exposures to infectious organisms known to cause uveitis are also important to consider. Patients who work on farms or work closely with animals are at higher risk for certain infectious diseases, including leptospirosis (seen in sewer or laboratory workers exposed to rat urine or contaminated water), brucellosis (seen in farm or slaughterhouse workers), and cat scratch disease and toxoplasmosis (seen in patients who work with felines).
Another environmental exposure to consider is an infected human being. TB is an example of a disease that is commonly acquired from person-to-person transmission. TB is easily spread through air droplets from a person with active disease.
Physical examination
In order to determine the appropriate laboratory workup in anterior uveitis, granulomatous uveitis must be differentiated from nongranulomatous uveitis. The appearance of the keratic precipitates (KPs) aids in differentiation. Granulomatous uveitis has large "mutton fat" KPs as well as clusters of cells in the anterior chamber (Busacca nodules), trabecular meshwork (Berlin nodules), or pupillary border (Koeppe nodules), whereas nongranulomatous uveitis has fine keratic precipitates over the corneal endothelium. These changes can be seen on dilated fundoscopic examination. Intermediate and posterior uveitis requires a dilated fundus examination to look for signs of vitritis (retinal exudates in the vitreous) and retinitis (retinal vascular sheathing, macular edema, optic disk swelling, and retinal hemorrhages). In cases of chronic inflammation, a posterior subcapsular cataract may be visualized as well.
Upon slit-lamp examination with tonometry, anterior uveitis may show conjunctival injection with exacerbation around the limbus (ciliary flush), a slight decrease in visual acuity, a decrease in intraocular pressure (rarely increased), lymphocyte aggregates in the corneal endothelium (keratic precipitates), corneal edema, and white blood cells or protein in the anterior chamber (flare). In nongranulomatous disease, fine cells are seen, but in granulomatous disease, mutton fat precipitates are found. Synechiae (iris adherence) to either the cornea (anterior synechia) or lens (posterior synechia) typically form during acute inflammation and can also be seen on slit-lamp examination. In cases of chronic inflammation, a posterior subcapsular cataract and band keratopathy may be visualized as well. A constricted, nonreactive pupil may also be seen.[Figure caption and citation for the preceding image starts]: Anterior uveitis with posterior synechiaeCourtesy of Mr Hugh Harris; used with permission [Citation ends].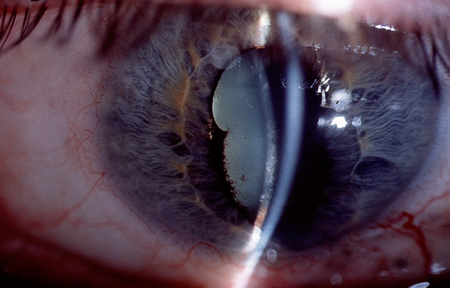 [Figure caption and citation for the preceding image starts]: Posterior synechiae (iris adhesions to anterior lens capsule) in this patient as a result of uveitisBMJ Case Reports 2012; doi:10.1136/bcr.12.2011.5418. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Posterior synechiae (iris adhesions to anterior lens capsule) in this patient as a result of uveitisBMJ Case Reports 2012; doi:10.1136/bcr.12.2011.5418. Used with permission [Citation ends].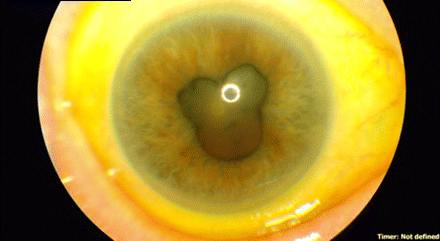
Laboratory testing
The list of potential laboratory tests for uveitis is very extensive. The initial focus is to narrow the workup based on the location of the uveitis (anterior, intermediate, posterior, panuveitis) as well as the type of uveitis (nongranulomatous versus granulomatous). Possible causes classified by location and type include:
Anterior uveitis
Granulomatous
Infectious: viral (HSV and varicella zoster virus [VZV]), TB, syphilis, Lyme disease
Autoimmune: sarcoidosis, Vogt-Koyanagi-Harada syndrome, granulomatosis with polyangiitis, sympathetic ophthalmia
Nongranulomatous
HLA-B27-associated anterior uveitis, juvenile idiopathic arthritis associated anterior uveitis, traumatic iritis, postoperative inflammation
With associated iris atrophy: viral (HSV, VZV, Epstein-Barr virus, CMV), syphilis, Fuchs heterochromic iridocyclitis
With associated keratitis: viral (HSV, VSV), sarcoidosis, syphilis, SLE
With associated scleritis: viral (HSV, VSV), sarcoidosis, syphilis, SLE, granulomatosis with polyangiitis, polyarteritis nodosa, relapsing polychondritis.
Intermediate uveitis
Infectious: Lyme disease, syphilis
Autoimmune: sarcoidosis, inflammatory bowel disease, multiple sclerosis, pars planitis.
Posterior uveitis
Infectious: toxoplasmosis chorioretinitis, toxocariasis, acute retinal necrosis, CMV retinitis, syphilis
Autoimmune: serpiginous choroiditis, APMPPE, birdshot chorioretinopathy, multifocal choroiditis.
Panuveitis
Infectious: syphilis, bacterial or fungal endophthalmitis (traumatic or endogenous)
Autoimmune: sarcoidosis, Vogt-Koyanagi-Harada syndrome, Behçet disease, SLE,
A greater emphasis is placed on finding infectious etiologies, since they are often more aggressive and may lead to permanent blindness long term. Once infectious etiologies are ruled out, the ophthalmologist can often collaborate with a rheumatologist and other medical specialties to investigate the autoimmune-mediated etiologies.
In patients with a first-episode unilateral, nongranulomatous uveitis without symptoms or systemic manifestations, no further evaluation is warranted. This is also true for patients with a recent history of trauma or surgery or with clinical signs of HSV or herpes zoster virus infection.
If the patient presents with bilateral, recurrent, or granulomatous uveitis, further evaluation is needed. Complete blood count, ACE level (elevated in sarcoidosis), syphilis serology, and HLA-B27 should be ordered to help identify a related systemic disease. Testing for rheumatoid factor and anti-cyclic citrullinated peptide antibodies should be done in the setting of possible rheumatoid arthritis. Antinuclear antibodies (ANA) and anti-double-stranded DNA (anti-dsDNA) antibodies are important diagnostic markers for SLE. Other HLA antigens may point to the presence of specific disorders. Elevated levels of anti-neutrophil cytoplasmic antibodies point to the presence of a vasculitic condition. Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and urinalysis can be useful nonspecific tests. CRP should be used ahead of ESR to check for inflammation in undiagnosed conditions due to increased sensitivity and specificity in the acute phase.[18]
Rapid plasma reagin (RPR), venereal disease research laboratory (VDRL), and fluorescent treponemal antibody (FTA-ABS) testing can help to identify syphilis infection. Ocular manifestations of syphilis involve secondary, tertiary, and neurosyphilis, and RPR and VDRL are usually positive in these patients. A positive FTA-ABS test result does not necessarily indicate active syphilis but a history of syphilis at some point, since the test remains positive for life after syphilis infection. False-positive results may occur in Lyme disease, leprosy, and diseases with high antinuclear antibody (ANA) levels. False-negative results may occur in tertiary syphilis.
If the patient has a history of known exposure or is suspected to be at high risk as a result of occupation, lifestyle, or hobbies, relevant tests should be performed: Lyme titer for Borrelia burgdorferi; purified protein derivative (PPD) skin testing for those with HIV, history of alcohol abuse, or suspected TB; toxoplasma titer; Bartonella henselae titer if cat-scratch disease is suspected. Special considerations should be taken when interpreting a PPD in patients who have had a previous Bacillus Calmette-Guérin vaccination or who are immunosuppressed. In patients with retinal vasculitis, ANA and anti-neutrophil cytoplasmic antibodies are needed. ANA is likely to be positive in JIA and so may be a particularly useful test in children.
Polymerase chain reaction may be considered to confirm suspected HSV, VZV, or CMV infection. Among viral causes, HSV and VZV are much more common.[13][14]
Vitrectomy (removal of vitreous humor) for cytological analysis, flow cytometry, and culture is not widely used at present, but when available it can be used to assist in identifying the etiology and thus guide treatment.
Use of this content is subject to our disclaimer