Criteria
Histologic features
Diagnosis of melanoma is made following histologic analysis of tissue; usually skin but in some cases from lymph nodes and other organ tissues.
Key histologic characteristics of melanoma include:[79]
Severe atypical melanocytes
Architectural disorder characterized by asymmetric growth pattern within the epidermis
Pagetoid scatter of melanocytes above the basal cell layer of the epidermis, confluent growth with a loss of the normal nested growth pattern of junctional melanocytes
Absence of maturation of the dermal melanocytic component with depth in the dermis.
Other abnormal features include regression (seen as dermal fibrosis with pigmented melanophages) and mitotic figures in the dermal melanocytic component.[79]
Prognostic information is also provided with a skin biopsy of a melanoma, including tumor thickness measured as Breslow thickness (depth of invasion measured in millimeters from the top of the granular cell layer to the point of deepest tumor penetration in the dermis or subcutis), ulceration, mitotic count, vascular invasion, and microscopic satellites.[14][63]
Breslow thickness
Depth of invasion (measured with a micrometer on a microscope during histopathologic evaluation of a biopsy specimen) in millimeters from the top of the granular cell layer to the point of deepest tumor penetration in the dermis or subcutis:[63]
Thin: <1 mm
Intermediate thickness: 1 mm to 4 mm
Thick: >4 mm.
Melanoma confined to the epidermis is termed melanoma in situ.
Clark level
Clark level is a measure of tumor thickness, but is less accurate than Breslow thickness. Use of the Clark level is primarily restricted to assessment of tumors <1 mm thickness. Clark level is determined by the level of invasion of malignant cells in the dermis or subcutis, with:[80]
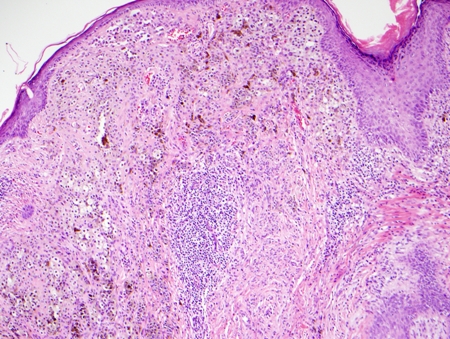
Level I corresponding to in-situ melanoma [Figure caption and citation for the preceding image starts]: Photomicrograph of melanoma in situFrom the personal collection of Dr Hobart Walling and Dr Brian Swick. [Citation ends].

Level II corresponding to invasion within the papillary dermis
Level III corresponding to invasion filling the papillary dermis
Level IV corresponding to invasion within the reticular dermis [Figure caption and citation for the preceding image starts]: Photomicrograph of Clark level IV invasive melanomaFrom the personal collection of Dr Hobart Walling and Dr Brian Swick. [Citation ends].
Level V corresponding to invasion into the subcutis.
Clinical staging of melanoma: American Joint Committee on Cancer TNM staging system (8th Edition)[62]
The American Joint Committee on Cancer (AJCC) staging system describes the extent of disease based on the following anatomic factors: size and extent of the primary tumor (T); regional lymph node involvement (N); and presence or absence of distant metastases (M). Nonanatomic prognostic factors (e.g., tumor grade, biomarkers) may be used to supplement the staging of certain cancers.
In general, cutaneous melanoma is categorized as:[14]
Localized disease (no evidence of metastases, stage I-II)
Regional disease (stage III)
Distant metastatic disease (stage IV).
Use of this content is subject to our disclaimer