Monitoring
Survivors of acute myocardial infarction should be closely followed up for adequate modification of risk factors and development of complications.[3][69] Patients should be evaluated within 2 to 3 weeks of discharge and evaluated periodically based on the extent of myocardial damage and patient condition.[Figure caption and citation for the preceding image starts]: 12-Lead ECG showing inferior and anterior ST-elevation with reciprocal changes in the lateral leadsFrom the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].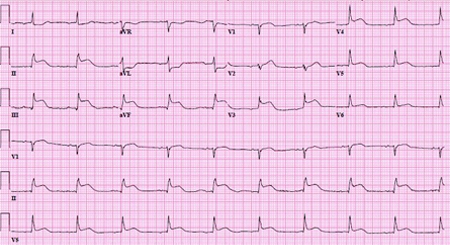 [Figure caption and citation for the preceding image starts]: 12-Lead ECG immediately after successful revascularization showing ST segments returning to baselineFrom the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 12-Lead ECG immediately after successful revascularization showing ST segments returning to baselineFrom the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].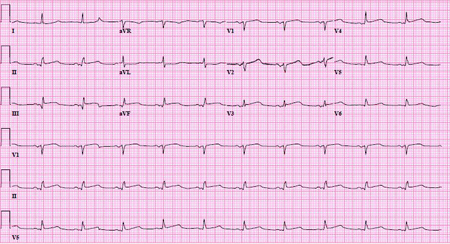 [Figure caption and citation for the preceding image starts]: 12-Lead ECG on follow-up 7 months later with normal ST segments and the absence of Q wavesFrom the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 12-Lead ECG on follow-up 7 months later with normal ST segments and the absence of Q wavesFrom the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].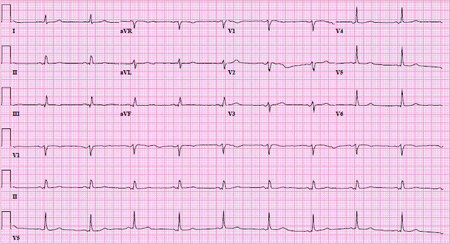
Initiating risk-factor modification and aggressive medical management prior to discharge has been associated with increased patient adherence. All patients should continue the optimal medical regimen indefinitely. This includes aspirin, P2Y₁₂ inhibitor (up to 1 year), beta-blockers, statins, and ACE inhibitors (especially in patients with decreased ejection fraction).
Ejection fraction is assessed by echocardiography 3 months after the acute episode and then periodically thereafter, depending on left ventricular (LV) function and symptoms.[79] Patients with ejection fraction <35% at 3 months' follow-up should be referred to an electrophysiologist for consideration of an implantable cardioverter defibrillator, as there is a high risk for arrhythmias in this population. Patients who develop diminished LV function and congestive heart failure should be followed up and managed appropriately.
Patients with a history of myocardial infarction are at increased risk for recurrent infarction. They should be evaluated by stress testing or cardiac catheterization if symptoms develop. Routine periodic ischemic evaluations with stress echocardiography or myocardial perfusion studies are controversial.
Use of this content is subject to our disclaimer