Tests
1st tests to order
resting ECG
Test
Resting ECG is appropriate for initial evaluation of all patients with known or suspected coronary disease.[24]
In addition to providing diagnostic and prognostic information, the presence of baseline ECG abnormalities may also guide use of further testing such as echocardiography and stress testing.[Figure caption and citation for the preceding image starts]: ECG showing nonspecific ST depressions in V5 and V6, which may indicate ischemia. There are nonspecific ST-segment changes in III and aVFFrom the collection of Dr S.D. Fihn; used with permission [Citation ends].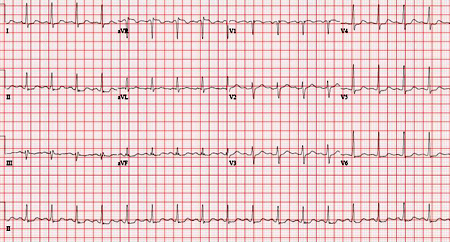 [Figure caption and citation for the preceding image starts]: Normal ECGFrom the collection of Dr S.D. Fihn; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Normal ECGFrom the collection of Dr S.D. Fihn; used with permission [Citation ends]. ECG may also reveal comorbid atrial fibrillation.
ECG may also reveal comorbid atrial fibrillation.
Result
often normal, but may reveal ST-T changes suggestive of ischemia or Q waves indicative of prior infarction
hemoglobin
Test
Anemia results in additional cardiac workload and reduced oxygen delivery to the heart, which can exacerbate angina. Severe anemia may cause angina without obstructive coronary lesions.[23]
Result
reduced in anemia
lipid profile
Test
Dyslipidemia is an important risk factor for coronary disease.
Result
elevated LDL cholesterol is associated with increased risk; elevated HDL is protective
fasting blood glucose or HbA1c
Test
Diabetes is an important risk factor for coronary disease and a common comorbidity.
Result
elevated in diabetes
Tests to consider
coronary CT angiography (CCTA)
Test
CCTA has high sensitivity and specificity and an increasing evidence base for prognosis and risk stratification. Severe coronary calcification can limit diagnostic quality. Risks are primarily related to contrast and radiation, although administration of beta-blockers or nitrates may also be required during the test.
For initial diagnosis, current US and European guidelines recommend either CCTA or stress testing with imaging. Exercise ECG has a limited role.[23][24] UK guidelines emphasize CCTA as the initial diagnostic test for chronic coronary disease and advise against exercise ECG.[92][93]
Result
typically luminal narrowing of >50% is considered positive, although the presence of lesser lesions is prognostically relevant; identification of "soft plaques" is also considered positive
exercise or pharmacologic stress with imaging
Test
Imaging options include single photon emission CT (SPECT), echocardiography, cardiac magnetic resonance (CMR), and positron-emission tomography (PET).
Imaging identifies the extent and distribution of inducible ischemia or irreversible infarct. The difference in summed scores for perfusion/wall motion from rest to stress adds prognostic information from ECG which is also recorded.
The addition of imaging improves sensitivity and perhaps specificity over exercise ECG. Imaging is required when patients' baseline ECG precludes the detection of ischemia or when a pharmacologic rather than exercise stress is used. Stress testing with imaging is also used for prognosis or to guide revascularization decisions in patients with known chronic coronary disease (CCD). Risks include inducing cardiac stress and (for SPECT and PET) the use of radiation.
Choice of imaging modality may be influenced by patient factors, and the exact questions being asked, as well as local availability and expertise. Stress echocardiography and SPECT are the best studied and most available. Echocardiography provides more detailed information about cardiac anatomy but is more operator dependent. US guidelines suggest a possible preference for PET over SPECT due to fewer nondiagnostic studies.[24]
For initial diagnosis, current US and European guidelines recommend either CCTA or stress testing with imaging. Exercise ECG has a limited role.[23][24] UK guidelines emphasize CCTA as the initial diagnostic test for CCD and advise against exercise ECG.[92][93]
Result
ST-segment elevation and depression on the ECG identify ischemia, as do wall motion or perfusion abnormalities on the imaging component
exercise ECG (without imaging)
Test
Patients use a treadmill, stationary cycle, or other device at increasing levels of speed and resistance while under medical supervision. In addition to ECG before, during, and in recovery from exercise, interpretation should include exercise capacity and heart rate achieved, as well as symptoms and hemodynamic response during and after exercise.
Scores such as the Duke treadmill score aid in determination of cardiac risk.
Risks are primarily related to inducing cardiac stress.
Not routinely recommended in European, UK or current US guidelines.[23][24][92][93]
Inappropriate for patients with baseline ECGs that make interpretation of exercise ST-segment changes difficult (left bundle branch block, baseline ST depression >1 mm, paced rhythm, digitalis use, preexcitation).
Inappropriate for patients who have limited exercise capacity (i.e., <4-5 METS) due to poor conditioning, obesity, physical impairments, or coexisting illness.[24][Figure caption and citation for the preceding image starts]: Baseline exercise ECG in a 55-year-old man with a 1-month history of angina on exertionFrom the collection of Dr S.D. Fihn; used with permission [Citation ends].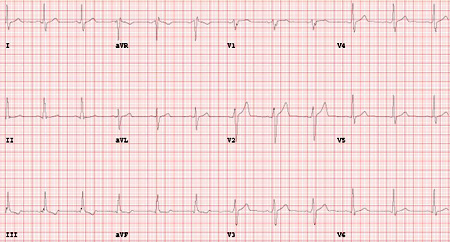 [Figure caption and citation for the preceding image starts]: Maximal exercise ECG in a 55-year-old man with a 1-month history of angina on exertion with ST depressions in II, III, aVF diagnostic of ischemia, and normal ST changes in V4-6 (rapid upsloping)From the collection of Dr S.D. Fihn; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Maximal exercise ECG in a 55-year-old man with a 1-month history of angina on exertion with ST depressions in II, III, aVF diagnostic of ischemia, and normal ST changes in V4-6 (rapid upsloping)From the collection of Dr S.D. Fihn; used with permission [Citation ends].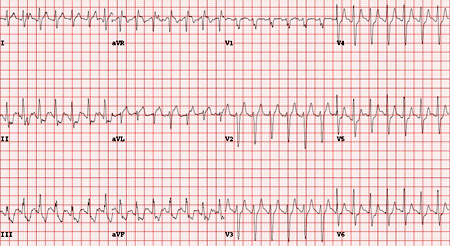 [Figure caption and citation for the preceding image starts]: Computerized summary of exercise ECG in a 55-year-old man with a 1-month history of angina on exertionFrom the collection of Dr S.D. Fihn; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computerized summary of exercise ECG in a 55-year-old man with a 1-month history of angina on exertionFrom the collection of Dr S.D. Fihn; used with permission [Citation ends].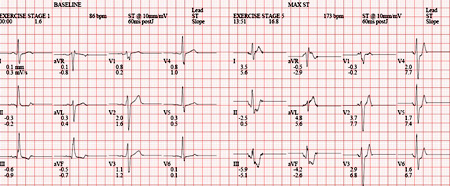
Result
ST-segment elevation and depression identify ischemia
invasive coronary angiography
Test
Coronary angiography is the conventional reference standard for diagnosis of coronary artery disease. Angiography also provides details about the overall coronary anatomy. Fractional flow reserve (FFR) is increasingly used to clarify the functional significance of stenoses, particularly when intervention is being considered without prior functional testing.
Risks include the use of radiation and administration of contrast, as well as thrombosis or hemorrhage related to vascular access, arrhythmia, and atheroembolism.
Invasive angiography is not typically used for initial diagnosis of chronic coronary disease, although in patients with a high pretest probability it may be used for confirmation of the diagnosis, risk stratification, and to identify appropriate candidates for revascularization. It may also be used for diagnosis when initial noninvasive testing is inconclusive.[24][Figure caption and citation for the preceding image starts]: Angiogram (right anterior oblique caudal projection) in a 55-year-old man with a 1-month history of angina on exertion. A 90% proximal stenosis of obtuse marginal 1 is present, explaining the patient's lateral ischemiaFrom the collection of Dr S.D. Fihn; used with permission [Citation ends].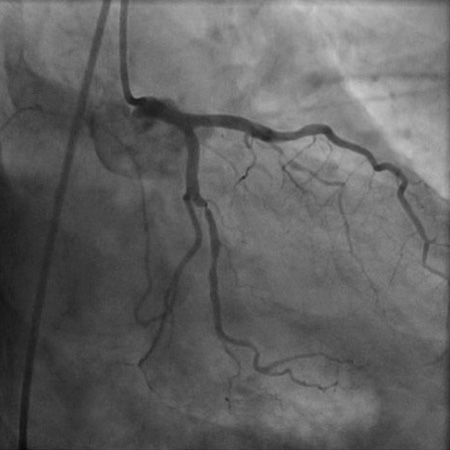 [Figure caption and citation for the preceding image starts]: Angiogram (right anterior oblique cranial projection) in a 55-year-old man with a 1-month history of angina on exertion. The image shows a 90% proximal stenosis of obtuse marginal 1 (explaining the patient's lateral ischemia), 90% proximal stenosis of the first diagonal, and 99% subtotal occlusion of the second diagonal (explaining the patient's anterior and anterolateral ischemia)From the collection of Dr S.D. Fihn; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Angiogram (right anterior oblique cranial projection) in a 55-year-old man with a 1-month history of angina on exertion. The image shows a 90% proximal stenosis of obtuse marginal 1 (explaining the patient's lateral ischemia), 90% proximal stenosis of the first diagonal, and 99% subtotal occlusion of the second diagonal (explaining the patient's anterior and anterolateral ischemia)From the collection of Dr S.D. Fihn; used with permission [Citation ends].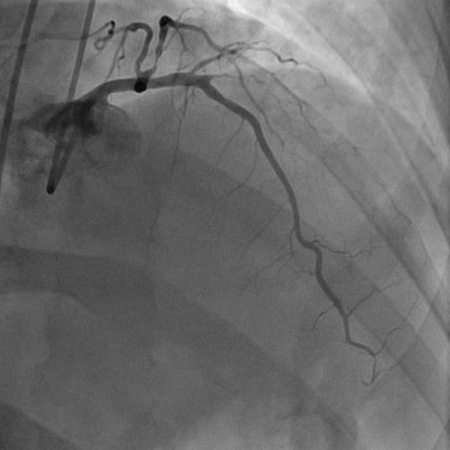
Result
50% to 70% luminal diameter narrowing is considered coronary obstruction, although presence of lesser lesions is prognostically relevant
thyroid function tests
Test
Testing of thyroid function may be included when thyroid disease is considered a possible contributor to angina.[23]
Result
below normal range (hyperthyroidism); elevated (hypothyroidism)
CXR
Test
X-ray may reveal alternate causes of chest symptoms.
Result
usually normal in chronic coronary disease
rest echocardiography
Test
European guidelines recommend routine echocardiography in patients with known or suspected CCD.[23] It can be used to identify prior MI; suggest alternative causes of chest symptoms; aid in diagnosis of comorbid conditions, such as heart failure, and provide prognostic information in patients with CCD. However, the value of this additional testing is not well established in patients without a history, exam, or ECG findings suggestive of prior event or associated condition.
Result
often normal in chronic coronary disease (CCD); focal wall motion abnormalities may indicate prior myocardial infarction (MI) and the extent of any impact on cardiac function; other findings may indicate alternative valvular, myocardial, or pericardial causes of chest symptoms
Emerging tests
CT myocardial perfusion (CTP) and fractional flow reserve CT (FFRCT)
Test
Both techniques add to coronary CT angiography and are designed to improve specificity by identifying functionally significant stenoses.[106][107][113]
CTP assesses myocardial uptake of contrast on CT scans with and without a pharmacologic stress. FFRCT uses computational fluid dynamics to assess flow in vessels based on data from coronary CT angiography without a pharmacologic stress phase.
Result
CTP shows perfusion in areas of myocardium, FFRCT shows flow in vessels
coronary artery calcium (CAC) scoring
Test
Calcium scoring can identify the overall burden of calcified atherosclerosis without characterizing the severity of specific stenoses. The test involves radiation but no contrast or induced cardiac stress. CAC scoring does not play a significant role in workup of chest pain or dyspnea. CAC is recommended for risk stratification in select asymptomatic patients considering interventions for primary prevention of coronary disease, such as initiating a statin medication.[44][99]
For symptomatic patients, an existing CAC score may be incorporated into calculation of a pretest probability to determine whether further diagnostic testing is indicated.[23][24][100]
However, do not use CAC scoring in patients with known atherosclerotic disease, including those with stents and bypass grafts, as it offers limited incremental prognostic value for patients with known disease.[24][103][104][105]
Result
overall calcification is usually reported in ranges from 0 to >400
tests for vasospasm and microcirculatory dysfunction
Test
Some patients have symptoms consistent with angina but lack the classic stenosis of epicardial coronary arteries. Patients with nonexertional symptoms suggestive of vasospastic angina may undergo ambulatory ECG monitoring and/or intracoronary acetylcholine testing. Patients with mixed exertional and nonexertional symptoms suggestive of microvascular dysfunction may undergo invasive or noninvasive assessment of coronary flow reserve and microcirculatory resistance as well as intracoronary acetylcholine testing.[23] Limited evidence shows improved symptoms with tailored therapy.[25]
Result
may show arteriolar dysregulation or increased microcirculatory resistance
Use of this content is subject to our disclaimer