Approach
The presentation of OP depends on the type. To establish whether there is any underlying cause, it is essential to take a full medical, surgical, and drug history and consider any possible occupational or environmental exposures. Most often, diagnosis is made using clinico-radiologic criteria and usually in the setting of a multidisciplinary team.
[Figure caption and citation for the preceding image starts]: Algorithmic approach to organizing pneumonia. ∗ A formal MDD may not be required in all cases, especially if the combination of clinical context and radiographic pattern is sufficiently convincing of the OP diagnosis. In such cases, a discussion between the physician and the radiologist is strongly encouraged. CRP = C-reactive protein; DAH = diffuse alveolar hemorrhage; Dx = diagnosis; ESR = erythrocyte sedimentation rate; GGO = ground-glass opacification; HRCT = high-resolution CT; MDD = multidisciplinary discussion; nl Pro-Cal C = normal procalcitonin; nl WBC = normal WBC; OP = organizing pneumoniaCherian SV, et al. Chest. 2022 Jul;162(1):156-78. doi: 10.1016/j.chest.2021.12.659. Epub 2022 Jan 14; used with permission [Citation ends].
Clinical diagnosis
Cryptogenic OP
Typically presents as a flu-like illness with mild fever, arthralgia, fatigue lasting for several days, and a mild cough lasting 1 to 3 months
Shortness of breath develops later as increasing numbers of alveoli are affected
Bilateral end-inspiratory crackles can be heard
There may be a rapidly progressive subtype presenting as bilateral infiltrates and acute hypoxic respiratory failure often requiring mechanical ventilation.
Auscultation sounds: late inspiratory crackles (rales)
Focal nodular OP
May be seen on chest x-ray or chest computed tomography (CT) scan as an incidental finding during investigation of an unrelated cough or chest pain
Nodule may be circular in 1 lung, or there may be 3 to 5 nodules in both lungs
May cause mild respiratory symptoms but is often asymptomatic
Typically low positive uptake on positron emission tomography (PET) scan[42]
Diagnosis often established after resection of a pulmonary mass thought to be a neoplastic process preoperatively.
Postinfectious OP
Develops in people who have an infectious pneumonia that initially responds to antibiotics, but the patchy infiltrates and mild respiratory symptoms persist as the inflammatory component of the infection becomes organized. Experience from the coronavirus disease 2019 (COVID-19) pandemic supports this observation.[43][44]
Drug-related OP
Occurs several weeks after medication is started
Presents with bilateral patchy infiltrates and cough that mimic infection or sometimes neoplasm, both of which must be ruled out before beginning corticosteroid therapy
Biopsy may be needed.
Connective tissue-related OP
Generally occurs months to years after diagnosis of the underlying disorder, although OP with cough, shortness of breath, and bilateral patchy infiltrates may precede the connective tissue disorder by months or even 1 to 2 years in people with polymyositis.[45][46]
OP following lung transplantation
Acute fibrinous organizing pneumonia is a feared postoperative complication of lung transplantation. This is associated with poor survival. Survivors may develop bronchiolitis obliterans syndrome.[47]
OP following breast radiation
Has emerged as an important development
May occur in up to 2% to 3% of women
Risk factors include age ≥50 years and concurrent endocrine therapy in women[21]
Tamoxifen not a risk factor
Mean latency is 4.4 months after radiation with a range of 2.3 to 7.9 months.
OP following occupational or environmental exposure
Occupational and environmental history important to exclude potential exposures
Occupational information includes job title and exposure information
Environmental information includes unusual toxic home exposures
Toxins that may trigger OP include textile printing dye,Penicillium mold dust, house fire, food spice processing, and paraffin mineral oil.[23][24][41]
Investigations
Chest x-ray is the initial investigation of choice and usually shows patchy infiltrates.[48][49] In many cases, patients are misdiagnosed with a community acquired pneumonia and are treated with a course of antibiotics.
Quite often, the symptoms persist and the chest x-ray worsens, usually with enlargement of the patchy infiltrates. [Figure caption and citation for the preceding image starts]: Chest x-ray showing bilateral patchy infiltratesFrom the collection of Gary R. Epler, MD [Citation ends]. In some situations, waxing and waning opacities may develop over a couple of weeks.
In some situations, waxing and waning opacities may develop over a couple of weeks.
A high-resolution chest computed tomography (CT) scan often shows bilateral ground-glass opacities with air bronchograms.[5][48][49][Figure caption and citation for the preceding image starts]: High-resolution chest CT showing bilateral ground-glass opacities and a posterior triangular-based infiltrate with an air bronchogramFrom the collection of Gary R. Epler, MD [Citation ends].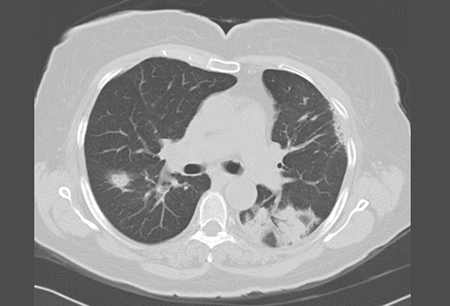 In OP, the ground-glass opacities with the air bronchograms are often in the shape of a triangle with the base of the triangle along the pleural surface and the apex toward the mediastinum ("the triangle sign").[2] Other radiographic patterns such as a diffuse infiltrative pattern, atoll sign, crazy paving, fibrotic changes and bands may be seen.
In OP, the ground-glass opacities with the air bronchograms are often in the shape of a triangle with the base of the triangle along the pleural surface and the apex toward the mediastinum ("the triangle sign").[2] Other radiographic patterns such as a diffuse infiltrative pattern, atoll sign, crazy paving, fibrotic changes and bands may be seen.
Pulmonary function tests (PFTs), if obtained, will show a decreased vital capacity and diffusing capacity with no airflow obstruction.[2][3][6]
Blood studies may show an increased WBC and erythrocyte sedimentation rate. C-reactive protein measurement, sputum culture and atypical viral screen may all help to exclude infection.[50]
A general autoimmune and myositis profile should be performed to screen for connective tissue disease if there is no obvious cause for OP as it may precede the diagnosis of connective tissue diseases by several months or years. The profile should include testing for: antinuclear antibodies, rheumatoid factor, anti-Scl-70 antibodies, anti-Sjögren-syndrome-related antigen A antibodies, anti-Sjögren-syndrome-related antigen B antibodies, cyclic citrullinated peptide antibodies, anti-ribonucleoprotein antibodies, antisynthetase antibodies, anticardiolipin antibodies, lupus anticoagulant antibodies, anti-glomerular basement membrane antibodies, and antineutrophil cytoplasmic antibodies/myeloperoxidase antibodies/proteinase 3 antibodies. Creatine kinase is useful for screening for polymyositis OP.
Often, a diagnosis of OP may be made based on clinical history, typical radiographic findings and significant negative or positive results from appropriate blood studies. Bronchoscopic investigations, including analysis of bronchoalveolar lavage fluid, may help to rule out other differential diagnoses such as eosinophilic pneumonia and to confirm that there is no active infection. The value of transbronchial biopsy is often doubtful since there is often insufficient tissue for the architecture to be evaluated, or the presence of crush artifacts which diminish its value. In one single center study, only 7 of 34 transbronchial biopsies demonstrated the pathology.[51]
Some experts feel that pathologic diagnosis is necessary. In that respect, a surgical lung biopsy represents best practice for confirmation in an atypical situation such as rapidly progressive disease, diffuse infiltrative disease, no known etiology or associated disorder, an unusual chest CT pattern, or with moderately severe symptoms. Pathologic criteria also state that the following features should not be present: extensive interstitial fibrosis, traction bronchiectasis, and histologic honeycombing.[1][2] Video-assisted thoracoscopy (VAT) is the preferred method for obtaining tissue.[28]
CT-guided transthoracic needle biopsy and transbronchial lung cryobiopsy are minimally invasive procedures that can be used as alternatives to surgical lung biopsy.[52][53][54] These may be important options in elderly or frail patients, as well as those with focal lesions. However, both procedures produce relatively small biopsy specimens that must be interpreted in the context of associated clinical and radiologic findings.[53]
Use of this content is subject to our disclaimer
