History and exam
Key diagnostic factors
common
dental pain/toothache
Prior history of pain/toothache may be a clue for periapical abscess.
Pain typically precedes swelling in periapical abscess; whereas, the reverse occurs in periodontal abscess.
Multiple factors affect severity of pain, including anatomic location, medications, and patient’s psychological state.
Facial pain may also be present.
Absence should direct the clinician to consider alternative etiologies.
thermal sensitivity of teeth
History of hot and/or cold sensitivity suggests a periapical abscess is more likely.
Formal thermal testing and/or electric pulp testing can be performed by a dental professional to help verify the vitality status of a tooth, and to help localize the source of symptoms and infection prior to treatment when multiple teeth are suspect.
fever
Temperature is a good predictor of acute infection and provides a means to help monitor a patient’s response to therapy.
Higher admission temperatures and peak temperatures have shown an association with increased length of hospital stay.[41]
intraoral and/or extraoral edema
Swelling over or near the root apex preceded by pain is more likely to be due to a periapical abscess. With a periodontal abscess, swelling tends to start closer to the gingival margin and typically precedes the pain.
Location and whether the swelling is fluctuant or nonfluctuant is important to note. Fluctuance indicates localized pus accumulation, and may be a good site to obtain an aspirate for culture. Cellulitis is generally nonfluctuant.
intraoral and/or extraoral erythema
Redness with warmth to touch may be an early clinical sign that precedes edema, or may be seen concurrently with visible or palpable edema.
intraoral and/or extraoral discharge
Purulent drainage tends to develop via a fistula (parulis) near the apex of the involved tooth with periapical abscess.[Figure caption and citation for the preceding image starts]: Panoramic radiograph with gutta percha tracking of intraoral fistula; shows large periapical radiolucency related to failed root canal treatment (note the multiple root canal-treated teeth)From the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].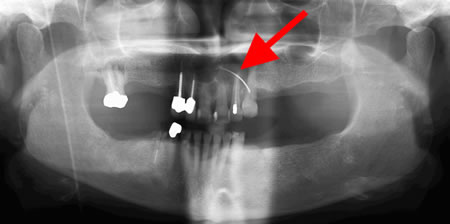 [Figure caption and citation for the preceding image starts]: Extraoral sinus tract in the right anterior neck related to retained necrotic mandibular first molarFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
[Figure caption and citation for the preceding image starts]: Extraoral sinus tract in the right anterior neck related to retained necrotic mandibular first molarFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
With a periodontal abscess, drainage is more likely to develop via the periodontal pocket.
As infections progress to involve multiple fascial spaces, spontaneous drainage develops and will occur via the path of least resistance. This may be intraoral and/or extraoral.
trismus
May be seen, as some odontogenic infections involve the muscles of mastication, floor of the mouth, and neck.
Normal mouth opening typically ranges from 35 to 45 mm. An interincisal opening of <10 mm suggests severe trismus, while an opening of 10 to 20 mm indicates moderate trismus, and 20 to 30 mm indicates mild trismus.[34]
In severe cases, trismus can limit oral intake and affect the patient’s nutritional and hydration status, and can also limit the physician’s ability to perform an intraoral exam.
An indicator of severe infection.[15]
tooth percussion sensitivity
Can indicate which teeth are involved. Typically, a periodontal abscess will be more tender with lateral percussion and a periapical abscess will be more tender to apical (vertical) percussion.
mobile teeth
May be due to local trauma, inflammation related to a periapical abscess (often with associated extrusion of the involved tooth), or secondary to supporting bone loss related to advanced periodontal disease.
deep periodontal pockets, bleeding, gingival recession
Dental probing is done by a dental professional to check the depth of the gingival sulcus that surrounds the tooth.
Deep periodontal pockets (i.e., >3 mm) occur with bone loss related to periodontal disease. These pockets can become obstructed, leading to a periodontal abscess.
Bleeding associated with probing indicates inflammation consistent with gingivitis or periodontitis. When longstanding periodontal disease is present, gingival recession is frequently seen often with partial root exposure and tooth mobility.
bone loss around teeth
Seen with advanced periodontal disease.
Clinically, patients often have associated gingival recession, often with some root exposure.
Seen as horizontal and/or vertical bone loss on periapical or panoramic radiographs.[Figure caption and citation for the preceding image starts]: Panoramic radiograph showing generalized advanced horizontal periodontal bone loss with periapical radiolucency (see arrow) related to left mandibular first molar consistent with combined endodontic/periodontal abscessFrom the personal collection of Melanie S. Lang and Thomas B. Dodson; used with permission [Citation ends].
elevated/extruded tooth
Occurs with inflammation related to a periapical abscess, often with some associated physiologic tooth mobility and severe pain with biting/chewing due to hyperocclusion.
Resolves with treatment of the periapical pathology and resolution of the associated inflammation.
tachypnea
In a mild-to-moderate infection, respiratory rate may show a mild increase with normal depth of respirations. However, in a severe infection with impending airway obstruction, respirations may become rapid and shallow.
uncommon
dysphagia/drooling
May develop with moderate-to-severe infections of the neck and floor of the mouth, as well as with a parapharyngeal or retropharyngeal abscess or Ludwig angina (cellulitis of floor of mouth).
Can limit oral intake and affect the patient’s nutritional and hydration status.
An indicator of severe infection.[15]
dysphonia
Informally described as a "hot potato" voice.
A muffled voice is concerning due to its association with pharyngeal/peritonsillar involvement and the potential for impending airway compromise.[20]
dyspnea/respiratory stridor
Patients who show any substantial signs of respiratory difficulty require immediate evaluation and intervention to prevent full respiratory obstruction.
posturing
Serious sign seen with partial airway obstruction in which patients may position themselves to try to straighten the airway and allow poorly controlled secretions to move outward and away from the airway.
uvular deviation
A very concerning sign for impending airway impairment.
Seen with a lateral pharyngeal space infection with the tonsil, lateral pharyngeal wall, and uvula being deflected to the opposing side.
Patients typically have an extremely sore throat and mild trismus.
floor of mouth elevation
May be seen with an abscess above the mylohyoid muscle involving the sublingual space.
Patients often report difficulty swallowing, or extending their tongues.
Concerning sign for impending airway impairment.
hypotension
Significant decreases in BP may be associated with volume depletion or sepsis.
Other diagnostic factors
common
halitosis/bad taste in mouth
Occurs secondary to bacteria that cause decay, releasing a sulfur compound that gives the breath an offensive odor and leaves a bad/bitter taste in the mouth.
Common finding with decay and subsequent development of a dental infection.
uncommon
xerostomia
Can be a short-term issue related to a serious odontogenic infection with dysphagia and trismus, which limits oral intake, or a more long-term issue related to prior head and neck radiation, salivary gland disease, Sjogren syndrome, diabetes, or an adverse effect of a medication.
Regardless of the etiology, when salivary flow is reduced, the risk for gingivitis and dental decay increases.
neurologic signs
Neurologic changes of any type are very concerning for progression of an infection.
Can range from local nerve impingement/compression (e.g., paresthesia) to the development of central nervous system (CNS) changes (related to meningitis, cerebral abscess, cavernous sinus thrombosis, or a decreased level of consciousness secondary to poor respiratory perfusion with impending airway obstruction).
With any significant CNS complication, eye signs (e.g., eye pain, photophobia, diplopia, proptosis, papillary dilation, papilledema, ophthalmoplegia, vision loss) are often seen.[20]
Risk factors
strong
poor oral hygiene
Poor general dental health predisposes people to the spread of odontogenic infections, and these people more commonly have multiple fascial space involvement.[Figure caption and citation for the preceding image starts]: Poor oral hygiene with lack of dental care and resultant rampant decayFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
Systemic response to infection, and course of infection, is more severe in patients with poor dental health with the absence of prior dental care. These patients have multiple infection focus sites compared with other patient groups.[12][13][14]
dental caries
In a prospective study of severe odontogenic infections warranting hospital admission, dental caries was found to be the most frequent cause in 65% of patients.[15][Figure caption and citation for the preceding image starts]: Poor oral hygiene with lack of dental care and resultant rampant decayFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
periodontal disease
Gingivitis can lead to periodontal disease with irreversible loss of supporting periodontal bone and compromise of the periodontal ligament. With bacterial invasion, a periodontal abscess can develop.
Periodontal disease is always preceded by gingivitis; however, with appropriate treatment, not all cases of gingivitis progress to periodontitis.
partially erupted or impacted tooth
dental trauma
Local trauma can lead to tooth injury or fracture with subsequent pulpal necrosis and development of a periapical abscess, or induction of a foreign body and development of a gingival abscess.
Teeth can develop immediate or delayed complications with the potential for internal or external resorption or pulpal necrosis following trauma. In some cases, this can be years later.
fractured teeth
Fractures may be due to trauma, decay, bruxism, or advanced periodontal disease. They can extend into the enamel, dentin, or pulp with the development of irreversible pulpitis or pulpal necrosis and periapical pathology.
excessive occlusal wear
May be due to coarse dietary intake, habits, or opposing porcelain restorations. When this occurs slowly there may be atrophy of the pulpal tissue; however, when it occurs more rapidly, pulpal necrosis occurs, which if left untreated causes a dental abscess to develop.
alcohol or drug misuse
Chronic drug misuse or excessive alcohol consumption is often associated with a poor nutritional status and a reduction in the body’s defense mechanisms, as well as local predisposing factors such as poor oral hygiene, rampant caries, uncontrolled periodontal disease, and other social, family, and psychological factors.[17]
People who use methamphetamine have high rates of dental disease. Perhaps unexpectedly, smoking or inhaling the drug is less of a risk factor than injecting it.[18]
low socioeconomic status
Retrospective demographic studies have shown patterns of association between lower socioeconomic status and poor health that are thought to be related to difficulty in accessing services; lower education level, with lack of awareness of the importance of timely management of dental infections; increased prevalence of trauma; and poor health habits related to diet, smoking, alcohol consumption, and substance misuse.[1][19]
malnutrition
Overall nutritional status affects a patient’s ability to resist infection, as well as recover from an existing infection. Malnutrition can occur chronically in many patient groups related to various factors, including age, dietary habits, socioeconomic factors, drug and alcohol misuse, or medical problems affecting nutrient absorption. More acute nutritional issues can develop secondary to decreased oral intake related to a dental infection.[20]
age extremes
Young infants may not have fully developed immune systems or antibody production. Older patients may have decreased T-cell function, along with concurrent medical conditions that affect their defense mechanisms. In addition, nutritional compromise and volume depletion can develop rapidly in these populations.[20]
prior radiation therapy
Systemic effects of radiation therapy can include a reduction in leukocyte activity and antibody production, which increases the risk of infection.
Head and neck radiation can lead to xerostomia, which increases the risk of dental caries.
High-dose head and neck radiation can predispose patients to osteoradionecrosis, which can occur spontaneously with minor trauma or following surgery that may be necessary to manage a dental abscess.[20]
certain medications
Some medications (e.g., antihistamines, anticholinergics, antidepressants, antipsychotics) can cause xerostomia, which increases the risk for gingivitis and dental caries.
Chronic pain management with opioid analgesics may mask initial symptoms for patients, leading to a delay in presentation with more advanced infections.
Recent antibiotic use can lead to more aggressive infections with drug-resistant microorganisms.
Chemotherapy agents, corticosteroids, and other immunosuppressants can significantly increase the risk of infections and predispose patients to more aggressive infections due to the decrease in the normal host defense mechanisms.
Bisphosphonates and denosumab can cause osteonecrosis of the jaw.[21] Osteonecrosis can lead to loss of vitality of adjacent teeth with the development of an associated dental abscess or infection.
weak
large dental restorations
Large restorations may be near the dental pulp and lead to irreversible pulpitis and subsequent pulpal necrosis. A prospective clinical trial reported a relationship between the presence of amalgam restorations and radiolucency size in patients who develop clinical signs of odontogenic infections.[27]
bruxism
Chronic tooth grinding can lead to dentin exposure or a cracked/fractured tooth which, if left untreated, can lead to pulpal necrosis and the development of a dental abscess.
prior root canal treatment failure
Root canal (endodontic) treatment involves removing inflamed or necrotic pulpal tissue, which is a source for a dental abscess/infection. The majority of root canal treatments are successful; however, in 5% to 15% of cases,[28][29] endodontic treatment fails due to accessory canals, incomplete obturation, root fracture, or a residual periapical cyst with development of a dental abscess or infection related to the tooth/area of endodontic failure.[Figure caption and citation for the preceding image starts]: Panoramic radiograph showing decayed bilateral mandibular third molars and failed root canal treatment with periapical lesion related to the right mandibular first molar (middle arrow); also shows carious bilateral mandibular third molars on both sidesFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
Use of this content is subject to our disclaimer