Tests
1st tests to order
CT head
Test
All patients with possible ischemic stroke should initially undergo a CT scan of the brain to rule out intracranial hemorrhage.[102][119][Figure caption and citation for the preceding image starts]: Noncontrast CT scan of brain showing subacute isolated left basal ganglion infarction with left frontal horn mass effectCourtesy of BMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1139 [Citation ends].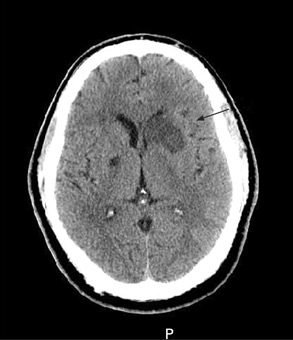
Most important test, needed to differentiate hemorrhagic from ischemic stroke, as an essential step in acute stroke therapy.[136]
Use the Alberta stroke program early CT score (ASPECTS) 1 (a 10-point quantitative topographic CT scan score) to assess early changes due to ischemic stroke.
In many cases, CT is normal within the first few hours of an ischemic stroke.[137]
Result
hypoattenuation (darkness) of the brain parenchyma; loss of gray matter-white matter differentiation, and sulcal effacement; hyperdensity in an artery is indicative of a possible thrombosis; direct visualization of thrombus or absence of venous filling may indicate cerebral venous thrombosis
MRI brain
Test
MRI of the brain, particularly with diffusion-weighted and gradient-echo sequences, provides more accurate information about the stroke lesion than CT, clearly highlights the area of ischemic infarct, and may provide further clues about the cause(s).[Figure caption and citation for the preceding image starts]: (A) Noncontrast T1-weighted MRI. (B) Post-contrast T1-weighted MRI showing minimal increase in leptomeningeal vessels over the right frontal region. (C) Diffusion-weighted image (DWI) showing a hyperintense area in the right frontal region. (D) Apparent diffusion coefficient (ADC) map shows hypointense lesion, indicating restricted diffusion that correlates with high intensity on DWI and exponential diffusion. (E) ADC value is 0.22 x 10¯³ mm²/second, corresponding to a hyperacute infarctFrom the personal collection of Eric E. Smith; used with permission [Citation ends].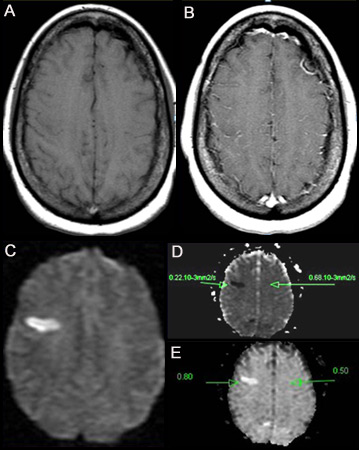 [Figure caption and citation for the preceding image starts]: (A) T2-weighted MRI image showing hyperintense signal representing prolonged T2. Shows abnormal T2 of 153.38 ms on the left, compared with the normal contralateral side (96 ms). Note that the lesion is located on the ascending frontal gyrus. (B) Gradient echo images detect hemosiderin compounds due to magnetic susceptibility of iron. In this case the result is negativeFrom the personal collection of Eric E. Smith; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: (A) T2-weighted MRI image showing hyperintense signal representing prolonged T2. Shows abnormal T2 of 153.38 ms on the left, compared with the normal contralateral side (96 ms). Note that the lesion is located on the ascending frontal gyrus. (B) Gradient echo images detect hemosiderin compounds due to magnetic susceptibility of iron. In this case the result is negativeFrom the personal collection of Eric E. Smith; used with permission [Citation ends].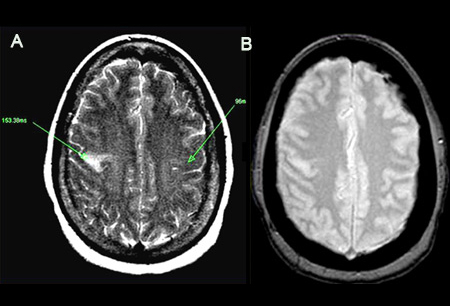
However, MRI may take more than 30 minutes to complete, and it is not universally available.
Has higher sensitivity for infarction and equivalent sensitivity for hemorrhage compared with CT.[138] In patients who awake with stroke or have unclear time of onset >4.5 hours from baseline or last known well, MRI can be used to identify diffusion-positive fluid-attenuated inversion recovery (FLAIR)-negative lesions. This mismatch between diffusion-weighted imaging and FLAIR findings on MRI can be useful for selecting those who may benefit from intravenous alteplase administration within 4.5 hours of stroke symptom recognition, or within 10 hours of last known well.[119] MRI scan using diffusion-weighted imaging (DWI) and FLAIR sequences can identify salvageable brain tissue (appears as a lesion that is visible on DWI but not on FLAIR sequences) in acute stroke patients with wake-up stroke, or in patients in whom time of stroke onset in the past 24 hours is unknown.[121] Both of these groups of patients may benefit from intravenous thrombolysis.[122][123]
Contraindicated in patients with certain metallic implants such as pacemakers.
Some specialized stroke centers use MRI as the initial imaging of choice, replacing CT.
May be implemented in the subacute phase after CT in some centers.
Result
acute ischemic infarct appears bright on diffusion-weighted imaging (DWI); at later stages, T2 images may also show increased signal in the ischemic territory; a lesion seen on DWI sequence but not on fluid attenuation inversion recovery (FLAIR) sequence more than 4.5 hours after stroke onset may indicate the presence of salvageable brain tissue; direct visualization of thrombus or absence of venous filling may indicate cerebral venous thrombosis
CT angiography or magnetic resonance angiography
Test
All patients with suspected large vessel occlusion who present within 6 hours of stroke onset and indications for mechanical thrombectomy should have CT angiography (CTA) or magnetic resonance angiography, to assess whether thrombectomy is indicated. In patients with symptomatic anterior circulation cerebral infarction or transient ischemic attack (TIA) who are candidates for revascularization, noninvasive cervical carotid imaging with carotid ultrasonography, CTA, or MR angiography is recommended to screen for stenosis of, or plaques within, the intracranial, carotid, or aortic vessels.[102][120] CTA of the head is the most rapid means of assessment of the intracranial vasculature for large vessel occlusion stroke.[120] CTA of the neck can be rapidly acquired together with CTA of the head, can provide further information about the etiology of the stroke, and may be useful for endovascular surgical planning for endovascular therapy.[102][120]
Result
identifies arterial occlusion or stenosis
CT or MRI perfusion
Test
For stroke patients with wake-up stroke or time of onset within the past 24 hours, CTA or magnetic resonance angiography plus CT perfusion or MRI perfusion should be performed to look for opportunities for thrombectomy between 6 and 24 hours after the patient was last known to be well.[119][120][123]
Result
a mismatch between perfusion and diffusion scans indicates the presence of penumbra and suggests that treatment may still be effective after usual cut-off times
serum glucose
Test
To exclude hypoglycemia as a cause for focal neurologic signs.
Hyperglycemia has been associated with poor outcome and risk of hemorrhagic transformation of ischemic stroke.[139][140][141]
Every patient with TIA or stroke should be screened for diabetes mellitus by measuring fasting plasma glucose or hemoglobin A1c, or with an oral glucose tolerance test.[102]
Assessment of blood glucose must precede initiation of intravenous thrombolysis.[119]
Result
may exclude hypo/hyperglycemia
serum electrolytes
Test
To exclude electrolyte disturbance as a cause for focal neurologic signs.
Result
may exclude electrolyte disturbance, such as hyper- or hyponatremia, or hyper- or hypokalemia
serum BUN and creatinine
Test
Renal failure may be a potential contraindication to some stroke interventions.
Result
may exclude renal failure
cardiac enzymes
Test
Stroke may be associated with concomitant myocardial infarction.[102]
Result
may exclude myocardial infarction
ECG
Test
Performed to exclude cardiac arrhythmia or ischemia, which are relatively common in ischemic stroke.[102]
Diagnostic protocols suggest a minimum of 24 hours of ECG monitoring after an ischemic stroke to exclude atrial fibrillation. ECG monitoring along with use of an insertable cardiac monitor has been reported to be superior to conventional ECG monitoring in diagnosing atrial fibrillation in patients with cryptogenic stroke.[124]
Patients with cryptogenic stroke or TIA who are 55 years old or older should have noninvasive ambulatory ECG with a target of 30 days because this enables clinicians to diagnose and treat paroxysmal atrial fibrillation.[125] Long-term rhythm monitoring (with mobile cardiac outpatient telemetry, implantable loop recorder, or other approach) is reasonable to detect intermittent atrial fibrillation in patients with stroke of indeterminate etiology.[102]
Result
may exclude arrhythmia or ischemia
CBC
Test
Used to detect conditions that may be potential contraindications for some acute stroke treatments and interventions. Excludes anemia or thrombocytopenia prior to possible initiation of thrombolytics, anticoagulants, or antithrombotics.
Result
may exclude anemia, thrombocytopenia, or polycythemia
coagulopathy screen
Test
If patient has no history of anticoagulant use, or of coagulopathy or a condition that may lead to it, intravenous thrombolysis does not need to be delayed until the test results are available.[119] In patients with cryptogenic stroke and confirmed cerebral venous thrombosis, it is reasonable to perform tests for inherited or acquired hypercoagulable state.[8][102]
Result
may show coagulopathy
Tests to consider
serum toxicology screen
Test
Performed in selected patients if suspicion of ingestion of toxic substances. In patients with cryptogenic stroke, it is reasonable to perform tests for illicit drug use (e.g., cocaine and amphetamines). Signs and symptoms may mimic stroke.[102]
Result
may exclude alcohol and drug abuse
infection screen
Test
In patients with cryptogenic stroke, it is reasonable to perform tests for bloodstream or cerebral spinal fluid infections, and for infections that can cause central nervous system vasculitis (e.g., varicella zoster virus, HIV and syphilis).[102] In patients with confirmed cerebral venous thrombosis, it is reasonable to perform tests for infections such as COVID-19.[8][92][93]
Result
positive if infection present (e.g., varicella zoster virus, HIV, syphilis, COVID-19)
genetic testing
Test
In patients with cryptogenic stroke or confirmed cerebral venous thrombosis, it is reasonable to perform tests for genetic tests for inherited diseases associated with stroke as clinically indicated.[8][102] Testing may identify single gene disorders with stroke as a primary manifestation (e.g., cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy [CADASIL], cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy [CARASIL], familial cerebral amyloid angiopathy).[126]
Result
may show evidence of a genetic disorder
CXR
Test
In the presence of cardiopulmonary signs or symptoms, a CXR can detect other relevant conditions.
Result
normal; or cardiomegaly, aortic dissection, pneumonia
CT or magnetic resonance or digital subtraction venography
Test
If routine imaging studies fail to show arterial occlusion, and if the infarct imaging and clinical presentation show characteristics of venous stroke (e.g., ischemic tissue not conforming to a vascular territory, severe hemorrhagic transformation and/or edema, intractable seizures at presentation, signs of increased intracranial pressure), patency of cerebral venous sinuses can be assessed by CT, magnetic resonance, or digital subtraction venography.[8] Magnetic resonance venography is recommended to confirm the diagnosis of cerebral venous sinus thrombosis.[8] CT venography is a reasonable alternative in centers with limited resources or if the pretest probability is low.[8] Digital subtraction venography is typically used only when invasive treatments are being considered.[8]
Result
identifies filling defects (“empty delta sign”), venous infarcts
carotid ultrasound
Test
More frequently performed in the subacute stage to investigate for carotid stenosis, or in patients who cannot have contrast or MRI.
Result
identifies cervical artery occlusion or critical stenosis
echocardiogram
Test
In patients with cryptogenic stroke, echocardiography with or without contrast is reasonable to evaluate for possible cardiac sources of or transcardiac pathways for cerebral embolism.[102] Cardioaortic embolism to the brain accounts for approximately 15% to 30% of ischemic strokes.[2][127] Transthoracic echocardiography (TTE) is preferred over transesophageal echocardiography (TEE) for the detection of left ventricular (LV) thrombus, but TEE is superior to TTE in detecting left atrial thrombus, aortic atheroma, prosthetic valve abnormalities, native valve abnormalities, atrial septal abnormalities, and cardiac tumors.[102]
Do not use TEE to detect cardiac sources of embolization if a source has been identified and it will not change the patient management.[128]
Result
identifies atrial and ventricular thrombus, aortic atheroma, prosthetic valve abnormalities, native valve abnormalities, atrial septal abnormalities, and cardiac tumors
transcranial Doppler ultrasound
Test
In patients with ischemic stroke or TIA in whom patent foramen ovale (PFO) closure is contemplated, transcranial Doppler with embolus detection might be reasonable to screen for right-to-left shunt.[102] Transcranial Doppler compares favorably with transthoracic echocardiography for detecting right-to-left shunting, which is usually the result of PFO.[102]
May be used to identify arterial occlusion of the major arterial branches of the circle of Willis. Especially useful for detecting vasospasm in patients with subarachnoid hemorrhage, and sickle cell anemia in children.
Spatial resolution is limited compared with CT and magnetic resonance angiography.[120]
Result
detects intracardiac shunt such as a PFO, or intrapulmonary arterial-venous shunt; artery to artery emboli; may reveal intracranial artery occlusion or critical stenosis; monitors for vasospasm and for sickle cell anemia in children
conventional (invasive) angiography
Test
Has the highest spatial and temporal resolution of any vascular imaging study. Due to the invasive nature of catheter-directed angiography, other modalities are typically preferred in the initial work-up for stroke.[120] Reserved for patients in whom endovascular intervention is an option, or if more information is needed to better understand the hemodynamic status of ischemic brain (e.g., to define collateral blood supply) for further management (e.g., revascularization).[102][120]
Result
vascular occlusion or stenosis, vasculitis, arterial dissection, reversible cerebral vasoconstriction syndrome, Moyamoya disease (vascular occlusion affecting circle of Willis), fibromuscular dysplasia
Use of this content is subject to our disclaimer