The goals of the initial evaluation are to identify the stroke syndrome, ensure medical stability, perform an abbreviated neurologic exam (e.g., National Institutes of Health Stroke Scale [NIHSS]),
[
NIH Stroke Score
Opens in new window
]
and rapidly transport the patient to the computed tomography (CT) or magnetic resonance imaging (MRI) scanner to begin scanning as soon as possible.[117]Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011 Sep;42(9):2651-65.
https://www.ahajournals.org/doi/full/10.1161/strokeaha.111.615336
http://www.ncbi.nlm.nih.gov/pubmed/21868727?tool=bestpractice.com
Because of time constraints, parts of the history and physical examination may be deferred until after scanning and the decision to perform thrombolysis. This is because the sensitivity and specificity to correctly diagnose and localize ischemic stroke from the neurologic history and examination are fairly low. Additionally, many other neurologic conditions can mimic stroke. Craniocervical CT or MRI is required for the proper diagnosis of ischemic stroke and to exclude intracranial hemorrhage.
In many cases, consultation with a stroke physician is helpful. This is particularly true when thrombolysis or other acute reperfusion therapies are contemplated; guidelines recommend that thrombolysis is given by stroke physicians following institutional written care protocols.[117]Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011 Sep;42(9):2651-65.
https://www.ahajournals.org/doi/full/10.1161/strokeaha.111.615336
http://www.ncbi.nlm.nih.gov/pubmed/21868727?tool=bestpractice.com
Time of onset
The most important information in the history, apart from the presence of neurologic symptoms, is the time of onset. Time from stroke onset is the main factor that determines eligibility for acute stroke treatments.
Time of stroke onset is not always easy to determine, particularly if onset was not witnessed and the patient is unable to communicate; symptoms are mild and not immediately noticeable; or there is a stuttering or fluctuating course. When onset was unwitnessed, the appropriate operational definition of symptom onset is the time when the patient was "last known normal" (i.e., did not have any stroke symptoms). This also implies that if signs and symptoms completely resolve during a fluctuating course, the clock for determining eligibility for recanalization may be reset.
Prior medical information relevant to the acute management of stroke
Includes:
Recent stroke
Atrial fibrillation
Seizure or epilepsy
Myocardial infarction
Recent surgery
Recent trauma
Bleeding
History of hemorrhagic stroke
Comorbidities (specifically hypertension and diabetes)
Current or past illicit drug use
Medications (specifically anticoagulants, insulin, and antihypertensives).
Other risk factors include older age (with the exception of cerebral venous thrombosis which occurs most frequently in younger women), history of transient ischemic attack (TIA), African-American or Hispanic/Latino ancestry, smoking, other comorbid cardiac conditions, carotid artery stenosis, and sickle cell disease.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
[10]Seth SM, Aaron WA, Zaid IA, et al. 2024 Heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2024 Jan 24;149:e347-913.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001209
[11]Tsao CW, Aday AW, Almarzooq ZI, et al; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation. 2023 Feb 21;147(8):e93-621.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001123
http://www.ncbi.nlm.nih.gov/pubmed/36695182?tool=bestpractice.com
[12]Gardener H, Sacco RL, Rundek T, et al. Race and ethnic disparities in stroke incidence in the Northern Manhattan Study. Stroke. 2020 Apr;51(4):1064-9.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7093213
http://www.ncbi.nlm.nih.gov/pubmed/32078475?tool=bestpractice.com
[13]Howard G, Moy CS, Howard VJ, McClure LA, et al. Where to focus efforts to reduce the Black-White disparity in stroke mortality: incidence versus case fatality? Stroke. 2016 Jul;47(7):1893-8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4927373
http://www.ncbi.nlm.nih.gov/pubmed/27256672?tool=bestpractice.com
[15]Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011 Jul;42(7):2091-116.
https://www.ahajournals.org/doi/full/10.1161/STR.0b013e3182213e24
http://www.ncbi.nlm.nih.gov/pubmed/21617147?tool=bestpractice.com
[29]Kissela BM, Khoury JC, Alwell K, et al. Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology. 2012 Oct 23;79(17):1781-7.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475622
http://www.ncbi.nlm.nih.gov/pubmed/23054237?tool=bestpractice.com
[30]Adams RJ, McKie VC, Hsu L, et al. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med. 1998 Jul 2;339(1):5-11.
https://www.nejm.org/doi/10.1056/NEJM199807023390102
http://www.ncbi.nlm.nih.gov/pubmed/9647873?tool=bestpractice.com
[35]Shahjouei S, Sadighi A, Chaudhary D, et al. A 5-decade analysis of incidence trends of ischemic stroke after transient ischemic attack: a systematic review and meta-analysis. JAMA Neurol. 2021 Jan 1;78(1):77-87.
https://www.doi.org/10.1001/jamaneurol.2020.3627
http://www.ncbi.nlm.nih.gov/pubmed/33044505?tool=bestpractice.com
[36]Lioutas VA, Ivan CS, Himali JJ, et al. Incidence of transient ischemic attack and association with long-term risk of stroke. JAMA. 2021 Jan 26;325(4):373-81.
https://www.doi.org/10.1001/jama.2020.25071
http://www.ncbi.nlm.nih.gov/pubmed/33496774?tool=bestpractice.com
[44]Chambers BR, Norris JW. Outcome in patients with asymptomatic neck bruits. N Engl J Med. 1986 Oct 2;315(14):860-5.
http://www.ncbi.nlm.nih.gov/pubmed/3528855?tool=bestpractice.com
[45]Barnett HJ, Taylor DW, Haynes RB, et al; North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991 Aug 15;325(7):445-53.
https://www.nejm.org/doi/10.1056/NEJM199108153250701
http://www.ncbi.nlm.nih.gov/pubmed/1852179?tool=bestpractice.com
Physicians, as well as the emergency medical team attending to the patient in the field, should establish contact with witnesses or next of kin (or healthcare proxy). This is necessary not only to obtain an accurate and relevant history but also to seek consent for invasive tests or treatments if needed.
Presenting symptoms
The presenting symptoms are highly variable depending on the mechanism and location of stroke. In most cases, the symptoms of ischemic stroke appear rapidly, over seconds or minutes.
The most common symptoms of anterior circulation stroke are ipsilateral:
Posterior circulation stroke often presents with:
Arterial dissections may present with:
Lacunar strokes often present with:
Limb and/or facial weakness (typically affects face, leg, and arm equally)
Speech difficulty
Ataxia
Paresthesias or numbness (typically affects face, leg, and arm equally)
Cerebral venous thrombosis is often associated with:[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Headache
Nausea and/or vomiting
Visual loss or diplopia
Seizures
Physical exam and neurologic assessment
To ensure a timely and adequate neurologic evaluation in acute stroke, assessment using the NIHSS should be performed as a priority. This helps to determine stroke severity and provides useful information to guide the treatment decision-making process.
[
NIH Stroke Score
Opens in new window
]
Initial assessment should aim to identify airway, breathing, and circulatory insufficiencies requiring urgent treatment. General systemic exam should seek evidence of risk factors: for example, cardiac arrhythmias or valvular pathology. Arrhythmias, murmurs, and pulmonary edema are associated with cardiac comorbidities, which predispose patients to stroke. Infections for example, otitis, mastoiditis, facial infection are associated with cerebral venous thrombosis.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Other detailed neurologic exam can be done as needed once the treatment paradigm has been determined.
As with symptoms, presenting signs of stroke can be highly variable depending on its mechanism and location.
Anterior circulation strokes are commonly associated with:
Partial or total loss of strength in face and upper and/or lower extremities (usually unilateral)
Expressive and/or receptive language dysfunction (dysphasia)
Sensory loss in face and upper and/or lower extremities (associated with sensory neglect if nondominant hemisphere stroke)
Vision loss in one eye or visual field deficit
Monocular vision loss may occur and is often transient.[118]Tao WD, Liu M, Fisher M, et al. Posterior versus anterior circulation infarction: how different are the neurological deficits? Stroke. 2012 Aug;43(8):2060-5.
https://www.doi.org/10.1161/STROKEAHA.112.652420
http://www.ncbi.nlm.nih.gov/pubmed/22678088?tool=bestpractice.com
This is a common early warning signal for cervical carotid stenosis. It can present as amaurosis fugax or retinal stroke (branch or central retinal artery occlusion); recognize and investigate with the same urgency.
Gaze paresis (often horizontal and unidirectional). Wrong-way eye deviation (i.e., gaze deviation away from the side of the brain lesion, toward the hemiparetic side) should prompt consideration of seizure but can also occur with strokes affecting the pons or thalamus. Horner syndrome suggests ipsilateral carotid dissection.
Posterior circulation strokes are more commonly associated with:
Specific cranial nerve deficits: for example, unilateral tongue weakness, diplopia
Horner syndrome (hemilateral triad of miosis, ptosis, and facial anhidrosis)
Visual field loss
Dysarthria
Nausea and/or vomiting
Difficulty with fine motor coordination and gait
"Crossed" syndromes:
Possible altered level of consciousness and coma
Lacunar strokes are associated with:
Cerebral venous thrombosis is commonly associated with:[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Headache
Nausea and/or vomiting
Visual symptoms; for example, transient visual obscurations or vision loss, papilledema, and diplopia
Other cranial neuropathies and focal neurologic deficits
Seizures
Because stroke can be the result of a general medical illness, such as a hypercoagulable state associated with a malignancy, or cardiac ischemia or arrhythmia, a thorough history is often very helpful to tailor specific management.
Imaging studies
After initial life support including management of airway, breathing, and circulation (see Management), the next immediate goal for all patients with TIA or possible ischemic stroke is to rapidly obtain a brain image.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
In patients suspected of having a stroke or TIA, CT or MRI of the brain is recommended to confirm the diagnosis of symptomatic ischemic cerebral vascular disease.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
Typically patients undergo a noncontrast head CT, in order to exclude a brain hemorrhage and guide treatment.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
In patients who awake with stroke or have unclear time of onset >4.5 hours from baseline or last known well, MRI can be used to identify diffusion-positive fluid-attenuated inversion recovery (FLAIR)-negative lesions. This mismatch between diffusion-weighted imaging and FLAIR findings on MRI can be useful for selecting those who may benefit from intravenous alteplase administration within 4.5 hours of stroke symptom recognition, or within 10 hours of last known well.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
CT perfusion or MRI of the brain, particularly with diffusion-weighted and gradient-echo sequences, provides more accurate information than CT about the stroke lesion, clearly highlights the area of ischemic infarct, shows any hemorrhagic changes, and may provide further clues about the cause(s).[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
However, MRI may take more than 30 minutes to complete, and is not universally available. CT and MRI data should be reviewed and interpreted by a physician with expertise in stroke imaging.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
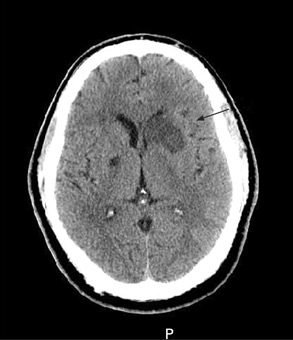
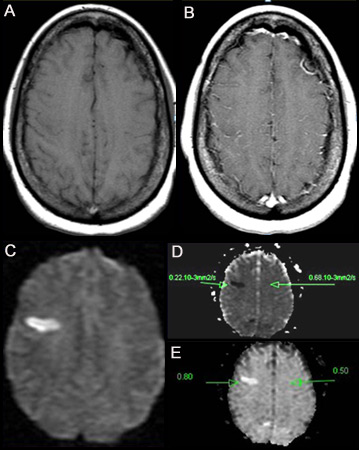
[Figure caption and citation for the preceding image starts]: (A) Noncontrast T1-weighted MRI. (B) Post-contrast T1-weighted MRI showing minimal increase in leptomeningeal vessels over the right frontal region. (C) Diffusion-weighted image (DWI) showing a hyperintense area in the right frontal region. (D) Apparent diffusion coefficient (ADC) map shows hypointense lesion, indicating restricted diffusion that correlates with high intensity on DWI and exponential diffusion. (E) ADC value is 0.22 x 10¯³ mm²/second, corresponding to a hyperacute infarctFrom the personal collection of Eric E. Smith; used with permission [Citation ends].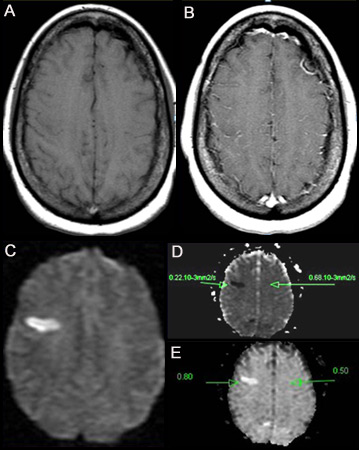 [Figure caption and citation for the preceding image starts]: (A) T2-weighted MRI image showing hyperintense signal representing prolonged T2. Shows abnormal T2 of 153.38 ms on the left, compared with the normal contralateral side (96 ms). Note that the lesion is located on the ascending frontal gyrus. (B) Gradient echo images detect hemosiderin compounds due to magnetic susceptibility of iron. In this case the result is negativeFrom the personal collection of Eric E. Smith; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: (A) T2-weighted MRI image showing hyperintense signal representing prolonged T2. Shows abnormal T2 of 153.38 ms on the left, compared with the normal contralateral side (96 ms). Note that the lesion is located on the ascending frontal gyrus. (B) Gradient echo images detect hemosiderin compounds due to magnetic susceptibility of iron. In this case the result is negativeFrom the personal collection of Eric E. Smith; used with permission [Citation ends].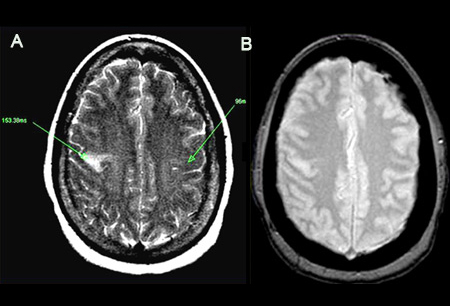 [Figure caption and citation for the preceding image starts]: Noncontrast CT scan of brain showing subacute isolated left basal ganglion infarction with left frontal horn mass effectCourtesy of BMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1139 [Citation ends].
[Figure caption and citation for the preceding image starts]: Noncontrast CT scan of brain showing subacute isolated left basal ganglion infarction with left frontal horn mass effectCourtesy of BMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1139 [Citation ends].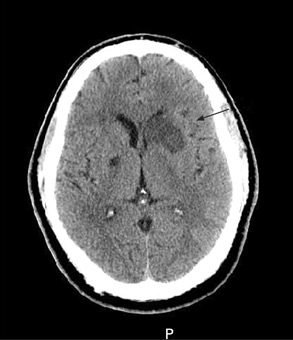
MRI scan using diffusion-weighted imaging (DWI) and FLAIR sequences can identify salvageable brain tissue (appears as a lesion that is visible on DWI but not on FLAIR sequences) in acute stroke patients with wake-up stroke, or in patients in whom time of stroke onset in the past 24 hours is unknown.[121]Schwamm LH, Wu O, Song SS, et al; MR WITNESS Investigators. Intravenous thrombolysis in unwitnessed stroke onset: MR WITNESS trial results. Ann Neurol. 2018 May;83(5):980-93.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6095471
http://www.ncbi.nlm.nih.gov/pubmed/29689135?tool=bestpractice.com
Both of these groups of patients may benefit from intravenous thrombolysis.[122]Campbell BC, Ma H, Ringleb PA, et al; EXTEND, ECASS-4, and EPITHET Investigators. Extending thrombolysis to 4·5-9 h and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet. 2019 Jul 13;394(10193):139-47.
http://www.ncbi.nlm.nih.gov/pubmed/31128925?tool=bestpractice.com
[123]Campbell BCV, Ma H, Parsons MW, et al. Association of reperfusion after thrombolysis with clinical outcome across the 4.5- to 9-hours and wake-up stroke time window: a meta-analysis of the EXTEND and EPITHET randomized clinical trials. JAMA Neurol. 2021 Feb 1;78(2):236-40.
http://www.ncbi.nlm.nih.gov/pubmed/33137171?tool=bestpractice.com
For patients with acute stroke presenting within 6 hours of onset and with suspected large vessel occlusion and indications for mechanical thrombectomy, CT head plus CT angiography (CTA) or magnetic resonance (MR) angiography should be performed.
For stroke patients with wake-up stroke or time of onset in the past 24 hours, CTA or MR angiography plus CT perfusion or MR perfusion should be performed to look for opportunities for thrombectomy between 6 and 24 hours after the patient was last known to be well.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
[123]Campbell BCV, Ma H, Parsons MW, et al. Association of reperfusion after thrombolysis with clinical outcome across the 4.5- to 9-hours and wake-up stroke time window: a meta-analysis of the EXTEND and EPITHET randomized clinical trials. JAMA Neurol. 2021 Feb 1;78(2):236-40.
http://www.ncbi.nlm.nih.gov/pubmed/33137171?tool=bestpractice.com
CT or MRI may show signs that increase suspicion for cerebral venous thrombosis for example, direct visualization of the thrombus or the absence of venous filling.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
The diagnosis of cerebral venous thrombosis should be confirmed with vascular imaging.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Other tests
While transport to CT/MRI is being organized, an intravenous catheter should be placed with blood sampling for:
The recommended target time for intravenous thrombolysis with alteplase (if indicated) is as soon as possible, and ideally no longer than 60 minutes from emergency department arrival.[117]Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011 Sep;42(9):2651-65.
https://www.ahajournals.org/doi/full/10.1161/strokeaha.111.615336
http://www.ncbi.nlm.nih.gov/pubmed/21868727?tool=bestpractice.com
[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
Only the assessment of blood glucose must precede the initiation of intravenous alteplase in all patients.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
Hypoglycemia has been associated with autonomic and neurologic symptoms, including stroke mimics and seizures, and hyperglycemia has been associated with intracerebral bleeding and worse clinical outcomes in patients treated with alteplase; both hypoglycemia and hyperglycemia can be excluded by bedside glucose test. Blood glucose should be normalized before initiation of thrombolysis.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
Treatment with alteplase must not be delayed by any additional tests unless a specific contraindication is suspected and needs to be ruled out.
ECG
An ECG should be performed to exclude cardiac arrhythmia or ischemia, which are relatively common in ischemic stroke.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Diagnostic protocols suggest a minimum of 24 hours of ECG monitoring after an ischemic stroke to exclude atrial fibrillation.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
ECG monitoring along with use of an insertable cardiac monitor has been reported to be superior to conventional ECG monitoring in diagnosing atrial fibrillation in patients with cryptogenic stroke.[124]Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014 Jun 26;370(26):2478-86.
https://www.nejm.org/doi/10.1056/NEJMoa1313600
http://www.ncbi.nlm.nih.gov/pubmed/24963567?tool=bestpractice.com
Long-term rhythm monitoring (with mobile cardiac outpatient telemetry, implantable loop recorder, or other approach) is reasonable to detect intermittent atrial fibrillation in patients with stroke of indeterminate etiology.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Patients with cryptogenic stroke or TIA who are 55 years old or older should have noninvasive ambulatory ECG with a target of 30 days because this enables clinicians to diagnose and treat paroxysmal atrial fibrillation.[125]Gladstone DJ, Spring M, Dorian P, et al; EMBRACE Investigators and Coordinators. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014 Jun 26;370(26):2467-77.
https://www.nejm.org/doi/10.1056/NEJMoa1311376
http://www.ncbi.nlm.nih.gov/pubmed/24963566?tool=bestpractice.com
Subsequent testing
Includes:
Serum toxicology screen. Performed in selected patients if there is a suspicion of ingestion of toxic substances. Signs and symptoms may mimic stroke.
In the presence of cardiopulmonary signs or symptoms, a chest x-ray can detect other relevant conditions such as cardiomegaly, aortic dissection, or pneumonia.
In patients with cryptogenic stroke, it is reasonable to perform tests for inherited or acquired hypercoagulable state, bloodstream or cerebral spinal fluid infections, infections that can cause central nervous system vasculitis (e.g., HIV and syphilis), illicit drug use (e.g., cocaine and amphetamines), and markers of systemic inflammation, and to perform genetic tests for inherited diseases associated with stroke, as clinically indicated.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Testing may identify single-gene disorders with stroke as a primary manifestation (e.g., cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy [CADASIL], cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy [CARASIL], familial cerebral amyloid angiopathy).[126]Boehme AK, Esenwa C, Elkind MS. Stroke risk factors, genetics, and prevention. Circ Res. 2017 Feb 3;120(3):472-95.
https://www.doi.org/10.1161/CIRCRESAHA.116.308398
http://www.ncbi.nlm.nih.gov/pubmed/28154098?tool=bestpractice.com
In patients with confirmed cerebral venous thrombosis, it is reasonable to perform tests for predisposing factors or associated medical conditions; for example, infections (e.g., COVID-19), inherited or acquired hypercoagulable state, autoimmune conditions (e.g., antiphospholipid antibody syndrome, systemic lupus erythematosus, Behçet disease, sarcoidosis) and to perform genetic tests for inherited diseases associated with confirmed cerebral venous thrombosis (e.g., MTHFR (C677T) polymorphism).[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Vascular imaging
In patients with symptomatic anterior circulation cerebral infarction or TIA who are candidates for revascularization, noninvasive cervical carotid imaging with carotid ultrasonography, CTA, or MR angiography is recommended to screen for stenosis of, or plaques within, the intracranial, carotid, or aortic vessels.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
CTA of the head is the most rapid means of assessment of the intracranial vasculature for large vessel occlusion stroke.[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
CTA of the neck can be rapidly acquired together with CTA of the head, and can provide further information about the etiology of the stroke, and may be useful for endovascular surgical planning for endovascular therapy.[119]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
High-resolution imaging of the intracranial large arteries and imaging of the extracranial vertebrobasilar arterial system can also be effective to identify atherosclerotic disease, dissection, moyamoya disease, or other etiologically relevant vasculopathies.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
Ultrasound of intracranial vessels (transcranial Doppler) or cervical carotids may be helpful to complement MR or CT angiographic data, and can continuously monitor changes in flow velocity. In patients with ischemic stroke or TIA in whom patent foramen ovale (PFO) closure is contemplated, transcranial Doppler with embolus detection might be reasonable to screen for right-to-left shunt.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Transcranial Doppler compares favorably with transthoracic echocardiography for detecting right-to-left shunting, which is usually the result of PFO.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Transcranial Doppler can also be used to identify arterial occlusion of the major arterial branches of the circle of Willis. It is specially useful for detecting vasospasm in patients with subarachnoid hemorrhage, and sickle cell anemia in children. Spatial resolution is limited compared with CT and MR angiography.[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
Cerebral angiography has the highest spatial and temporal resolution of any vascular imaging study. Due to the invasive nature of catheter-directed angiography, other modalities are typically preferred in the initial workup for stroke.[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
In ischemic stroke, conventional angiography is reserved for patients in whom endovascular intervention is an option, or if more information is needed to better understand the hemodynamic status of ischemic brain (e.g., to define collateral blood supply) for further management (e.g., revascularization).[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
[120]American College of Radiology. ACR appropriateness criteria: cerebrovascular diseases-stroke and stroke-related conditions. 2023 [internet publication].
https://acsearch.acr.org/docs/3149012/Narrative
If routine imaging studies fail to show arterial occlusion, and if the infarct imaging and clinical presentation show characteristics of venous stroke (e.g., ischemic tissue not conforming to a vascular territory, severe hemorrhagic transformation and/or edema, intractable seizures at presentation, signs of increased intracranial pressure), patency of cerebral venous sinuses can be assessed by venography (CT or MRI).[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
MRI venography is recommended to confirm the diagnosis of cerebral venous sinus thrombosis.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
CT venography is a reasonable alternative in centers with limited resources or if the pretest probability is low.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Digital subtraction venography is typically used only when invasive treatments are being considered.[8]Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e77-90.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000456
http://www.ncbi.nlm.nih.gov/pubmed/38284265?tool=bestpractice.com
Echocardiogram
In patients with cryptogenic stroke, echocardiography with or without contrast is reasonable to evaluate for possible cardiac sources of or transcardiac pathways for cerebral embolism.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
Cardioaortic embolism to the brain accounts for approximately 15% to 30% of ischemic strokes.[2]Adams HP Jr, Bendixen BH, Kappelle LJ, et al; TOAST Investigators. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial (TOAST - Trial of Org 10172 in Acute Stroke Treatment). Stroke. 1993 Jan;24(1):35-41.
https://www.ahajournals.org/doi/pdf/10.1161/01.STR.24.1.35
http://www.ncbi.nlm.nih.gov/pubmed/7678184?tool=bestpractice.com
[127]Kamel H, Healey JS. Cardioembolic stroke. Circ Res. 2017 Feb 3;120(3):514-26.
https://www.doi.org/10.1161/CIRCRESAHA.116.308407
http://www.ncbi.nlm.nih.gov/pubmed/28154101?tool=bestpractice.com
Transthoracic echocardiography (TTE) is preferred over transesophageal echocardiography (TEE) for the detection of left ventricular (LV) thrombus, but TEE is superior to TTE in detecting left atrial thrombus, aortic atheroma, prosthetic valve abnormalities, native valve abnormalities, atrial septal abnormalities, and cardiac tumors.[102]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
However, do not use TEE to detect cardiac sources of embolization if a source has been identified and it will not change the patient management.[128]American Society of Echocardiography. Five things physicians and patients should question. Choosing Wisely, an initiative of the ABIM Foundation. 2022 [internet publication].
https://web.archive.org/web/20230311070603/https://www.choosingwisely.org/societies/american-society-of-echocardiography
Assessing stroke risk after a TIA
One or more TIAs, which may be stereotypic, sometimes precede a stroke. Their prompt identification with proper intervention is essential in stroke prevention.
The ABCD2 score is a risk assessment tool that can help predict short-term stroke risk following TIA.[129]Johnston SC, Nguyen-Huynh MN, Schwarz ME, et al. National Stroke Association guidelines for the management of transient ischemic attacks. Ann Neurol. 2006 Sep;60(3):301-13.
http://onlinelibrary.wiley.com/doi/10.1002/ana.20942/full
http://www.ncbi.nlm.nih.gov/pubmed/16912978?tool=bestpractice.com
[
ABCD2 Score to Predict Stroke Risk after TIA
Opens in new window
]
The score is optimized to predict the risk of stroke within 2 days after a TIA, but can also predict stroke risk within 90 days.
ABCD3 and ABCD3-I scores are more detailed risk assessment tools that incorporate number of TIAs in the previous week and MRI findings. ABCD3 and ABCD3-I are more accurate than ABCD2 for predicting subsequent stroke.[130]Kiyohara T, Kamouchi M, Kumai Y, et al. ABCD3 and ABCD3-I scores are superior to ABCD2 score in the prediction of short- and long-term risks of stroke after transient ischemic attack. Stroke. 2014 Feb;45(2):418-25.
https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.113.003077
http://www.ncbi.nlm.nih.gov/pubmed/24335223?tool=bestpractice.com
[131]Zhao M, Wang S, Zhang D, et al. Comparison of stroke prediction accuracy of ABCD2 and ABCD3-I in patients with transient ischemic attack: a meta-analysis. J Stroke Cerebrovasc Dis. 2017 Oct;26(10):2387-95.
http://www.ncbi.nlm.nih.gov/pubmed/28647418?tool=bestpractice.com
[132]Mayer L, Ferrari J, Krebs S, et al; Austrian Stroke Unit Collaborators. ABCD3-I score and the risk of early or 3-month stroke recurrence in tissue- and time-based definitions of TIA and minor stroke. J Neurol. 2018 Mar;265(3):530-4.
https://link.springer.com/article/10.1007/s00415-017-8720-8
http://www.ncbi.nlm.nih.gov/pubmed/29327286?tool=bestpractice.com
ABCD3I calculator
Opens in new window
The UK National Institute for Health and Care Excellence (NICE) recommends that all people with suspected TIA are considered as potentially high risk for stroke, with specialist assessment and investigation within 24 hours of symptom onset. This is based on evidence that risk prediction scores used in isolation are poor at discriminating low and high risk of stroke after TIA.[133]National Institute for Health and Care Excellence. Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. April 2022 [internet publication].
https://www.nice.org.uk/guidance/ng128
 [Figure caption and citation for the preceding image starts]: (A) T2-weighted MRI image showing hyperintense signal representing prolonged T2. Shows abnormal T2 of 153.38 ms on the left, compared with the normal contralateral side (96 ms). Note that the lesion is located on the ascending frontal gyrus. (B) Gradient echo images detect hemosiderin compounds due to magnetic susceptibility of iron. In this case the result is negativeFrom the personal collection of Eric E. Smith; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: (A) T2-weighted MRI image showing hyperintense signal representing prolonged T2. Shows abnormal T2 of 153.38 ms on the left, compared with the normal contralateral side (96 ms). Note that the lesion is located on the ascending frontal gyrus. (B) Gradient echo images detect hemosiderin compounds due to magnetic susceptibility of iron. In this case the result is negativeFrom the personal collection of Eric E. Smith; used with permission [Citation ends].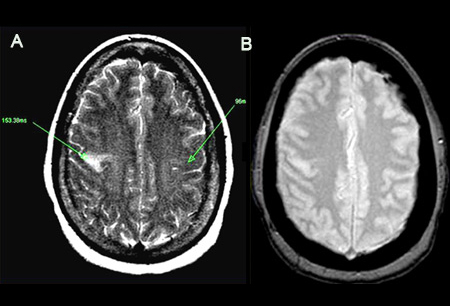 [Figure caption and citation for the preceding image starts]: Noncontrast CT scan of brain showing subacute isolated left basal ganglion infarction with left frontal horn mass effectCourtesy of BMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1139 [Citation ends].
[Figure caption and citation for the preceding image starts]: Noncontrast CT scan of brain showing subacute isolated left basal ganglion infarction with left frontal horn mass effectCourtesy of BMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1139 [Citation ends].