History and exam
Key diagnostic factors
common
creamy white or yellowish plaques, fairly adherent to oral mucosa
Typical appearance of pseudomembranous oral candidiasis, commonly known as "thrush".[1]
Removal of the plaque, by scraping, may reveal an erythematous base or a bleeding surface.
[Figure caption and citation for the preceding image starts]: Pseudomembranous candidiasis in diabetesFrom the collection of Fariba Younai, UCLA School of Dentistry, Los Angeles [Citation ends].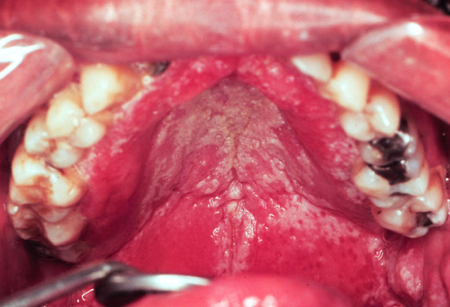 [Figure caption and citation for the preceding image starts]: Pseudomembranous candidiasis in HIVFrom the collection of Fariba Younai, UCLA School of Dentistry, Los Angeles [Citation ends].
[Figure caption and citation for the preceding image starts]: Pseudomembranous candidiasis in HIVFrom the collection of Fariba Younai, UCLA School of Dentistry, Los Angeles [Citation ends].
burning oral pain
May occur with both erythematous and pseudomembranous oral candidiasis.[1]
cracks, ulcers, or crusted fissures radiating from angles of the mouth
Typical appearance of angular cheilitis.
Frequently seen among patients with a deep fold in the corners of their mouth or a collapsed vertical dimension (bite collapse).[1]
Also seen in several types of vitamin and nutritional deficiency states.
Clinically, the lesions are moderately painful.
Other diagnostic factors
common
unpleasant taste in the mouth
Patients with pseudomembranous oral candidiasis may complain of a salty or bitter taste in their mouth.[1]
lesions on any part of the oral mucosa
Although it can occur anywhere on the oral mucosa, pseudomembranous oral candidiasis is most common on the palate, buccal mucosa, and the dorsum of the tongue.[1]
atrophic, fiery red, flat lesions on the palate
Typical appearance of erythematous oral candidiasis.[1]
patchy areas of loss of filiform papillae on the dorsum of the tongue
May occur with erythematous oral candidiasis.[1]
spotty red areas on the buccal mucosa
May occur with erythematous oral candidiasis.[1]
lesions confined to the outline of a dental prosthesis
Typical of denture stomatitis, found under removable prostheses. Lesions have a smooth and velvety or nodular surface, with varying degrees of erythema, and may be accompanied by petechial hemorrhage.[1][Figure caption and citation for the preceding image starts]: Candidiasis under a maxillary partial dentureFrom the collection of Fariba Younai, UCLA School of Dentistry, Los Angeles [Citation ends].
uncommon
dysphagia or odynophagia
rhomboid outline on the dorsal aspect of the tongue
Associated with median rhomboid glossitis; may be erythematous.[1]
Risk factors
strong
hyposalivation/xerostomia
poor oral hygiene, especially among denture wearers
advanced malignancy
Reduces effectiveness of the immune response.[37]
cancer chemotherapy and radiotherapy
HIV infection
HIV infection reduces the effectiveness of the immune response and is strongly associated with oral candidiasis.[11][12][38] However, the introduction of highly active antiretroviral therapy has led to a decrease in the incidence of cases in people living with HIV, including the number of refractory cases.[17][18]
[Figure caption and citation for the preceding image starts]: Opportunistic oral candidiasis infection in a patient with HIVPublic Health Image Library (PHIL) [Citation ends]. [Figure caption and citation for the preceding image starts]: Pseudomembranous candidiasis infection in a patient with HIVPublic Health Image Library (PHIL) [Citation ends].
[Figure caption and citation for the preceding image starts]: Pseudomembranous candidiasis infection in a patient with HIVPublic Health Image Library (PHIL) [Citation ends].
endocrine disturbance (e.g., diabetes mellitus, hypoparathyroidism, pregnancy, hypoadrenalism)
immunosuppressive agents (e.g., local or systemic corticosteroid therapy)
Reduces effectiveness of the local and systemic immune response.[32]
Risk associated with inhaled corticosteroids may be reduced by rinsing mouth with water post-dose or using a spacer device.
current or recent past use of broad-spectrum or multiple narrow-spectrum antibiotics
A result of the disturbance in normal oral flora.[32]
extremes of age
Neonates and older people have reduced immunity and are therefore predisposed to infections including those caused by Candida.[32]
weak
high carbohydrate diet
The presence of glucose enhances growth of Candida species in the saliva. Its adherence to the oral epithelium is also favored by a high carbohydrate diet.[32]
Use of this content is subject to our disclaimer